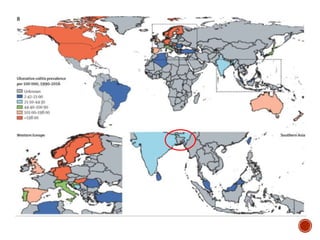
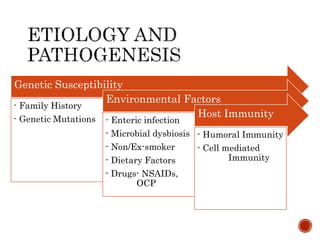
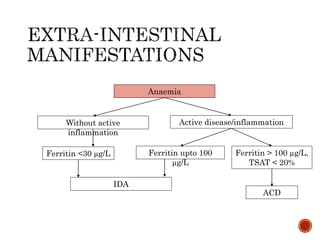
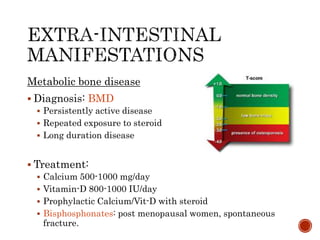
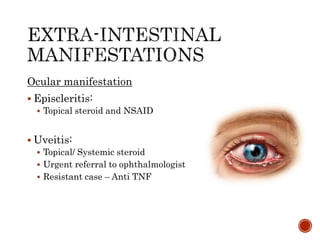
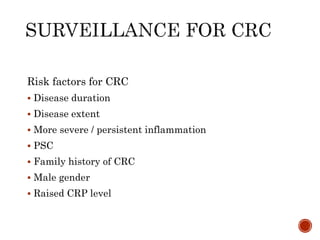
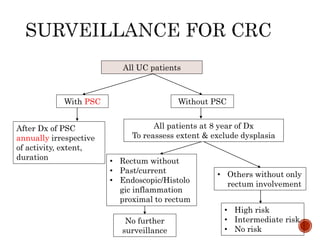
This document provides an overview of ulcerative colitis including its definition, epidemiology, etiology, pathogenesis, diagnosis, assessment, management, complications, and extra-intestinal manifestations. Some key points include:
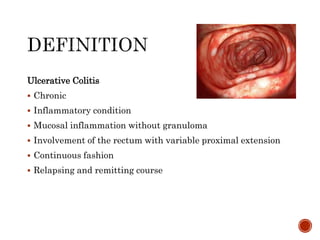
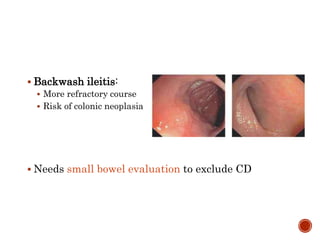
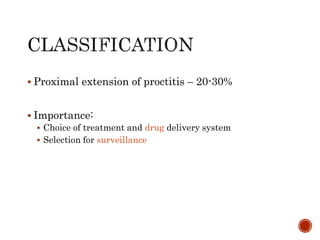
- UC is a chronic inflammatory bowel disease that involves the colonic mucosa. It typically affects the rectum and may extend proximally in a continuous pattern.
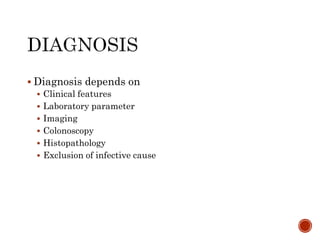
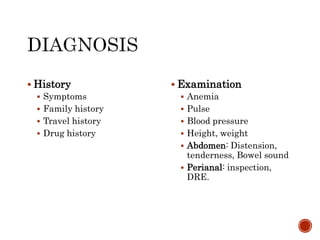
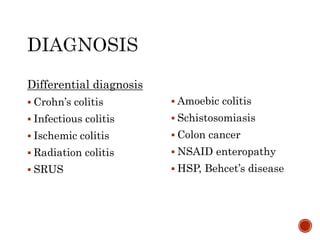
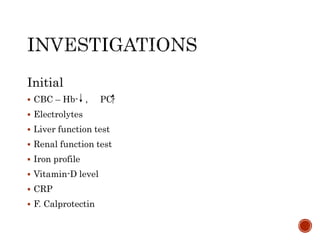
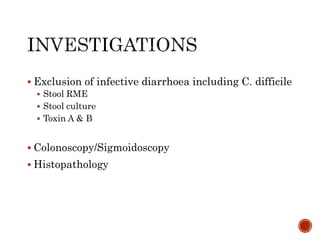
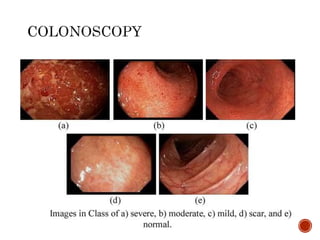
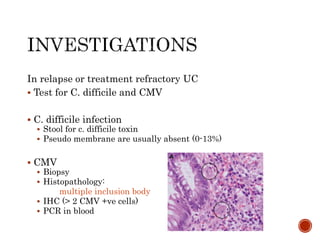
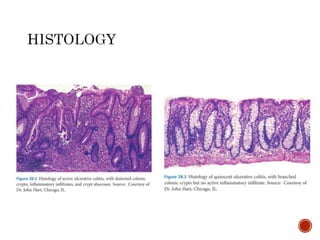
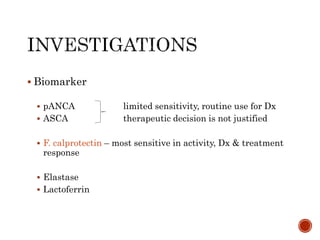
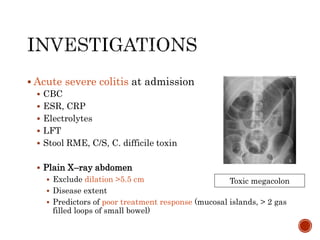
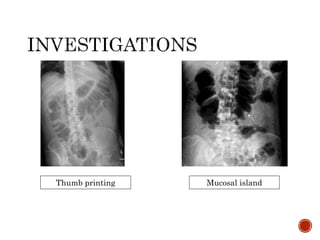
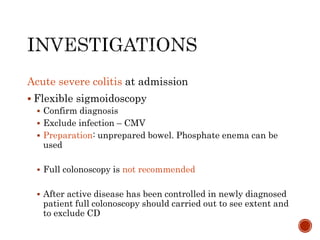
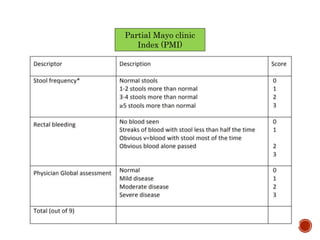
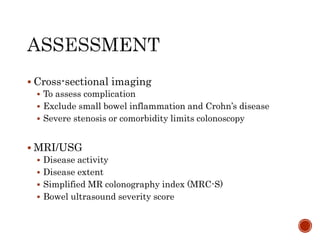
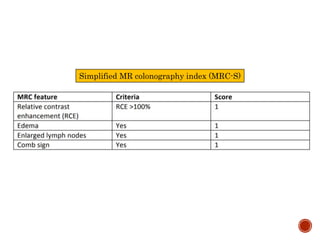
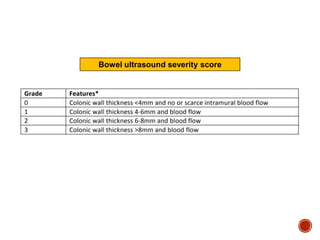
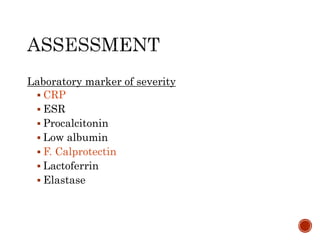
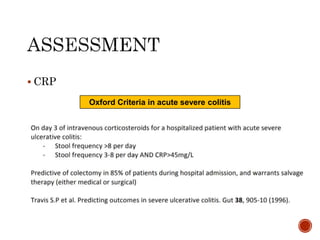
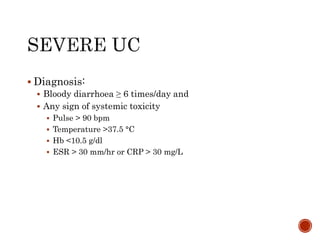
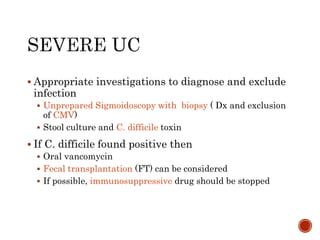
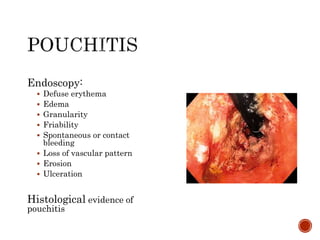
- Diagnosis involves clinical features, lab tests, endoscopy, histology, and ruling out other causes. Disease extent and severity are also assessed.
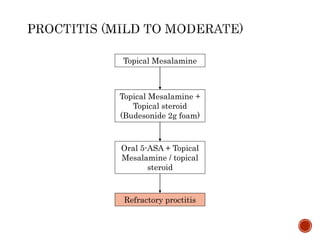
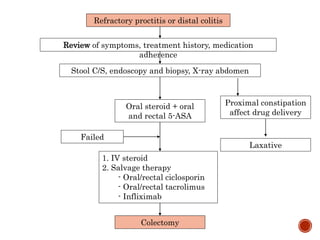
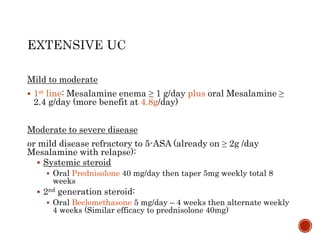
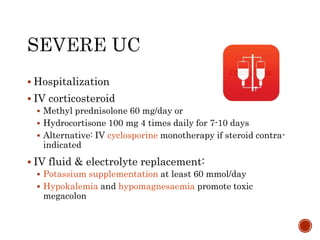
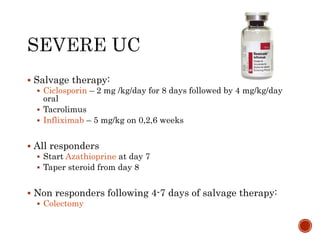
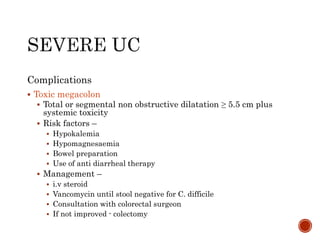
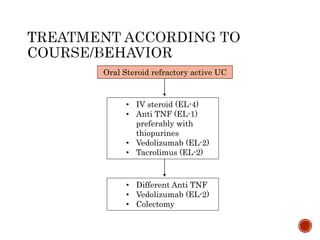
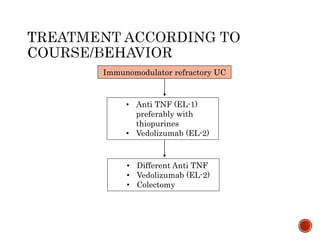
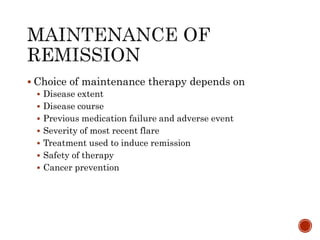
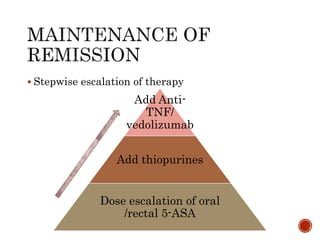
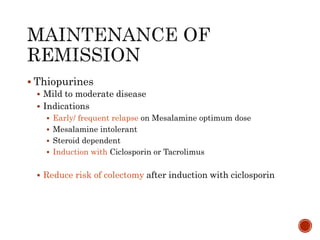
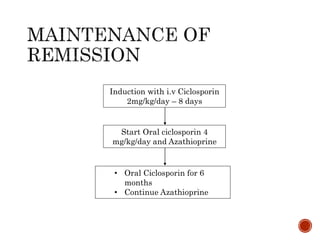
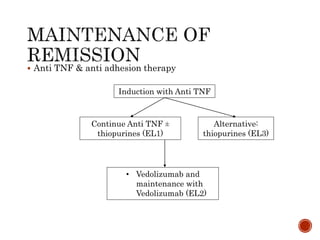
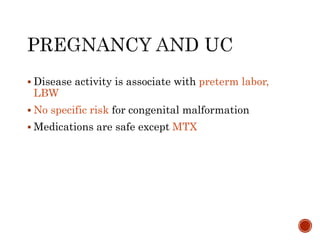
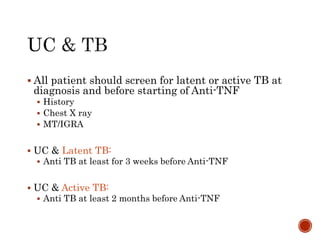
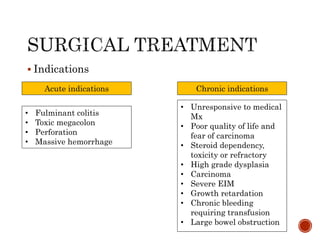
- Management depends on disease severity and extent, and may include 5-aminosalicylates, corticosteroids, immunomodulators, biologics, or colect