This document discusses the prevention of central line-associated bloodstream infections (CLABSI). It covers:
1. The burden of CLABSI, including mortality rates between 4-20% and annual costs ranging from $296 million to $2.3 billion in the US.
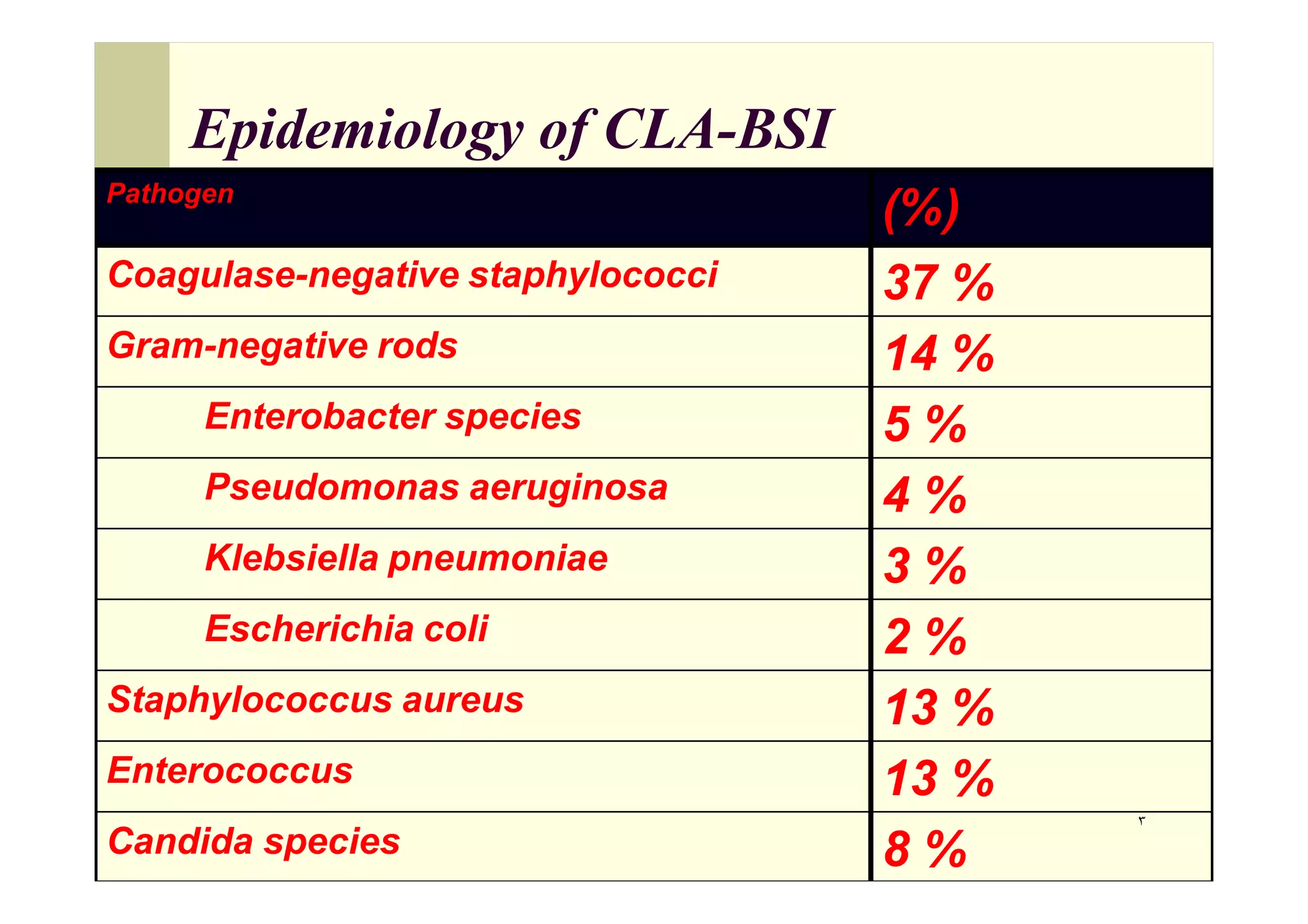
2. The epidemiology of CLABSI pathogens, with coagulase-negative staphylococci being the most common cause at 37%.