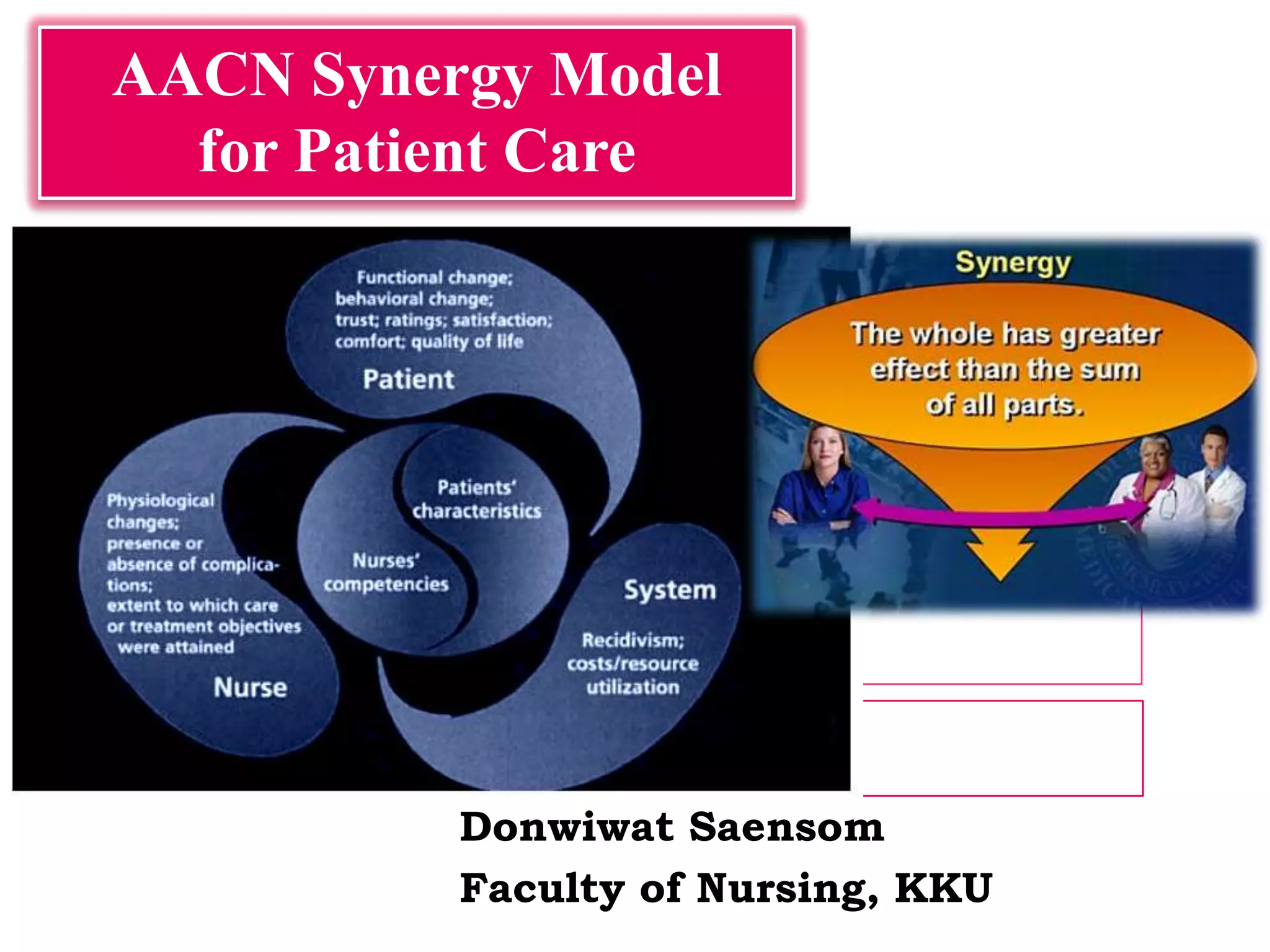
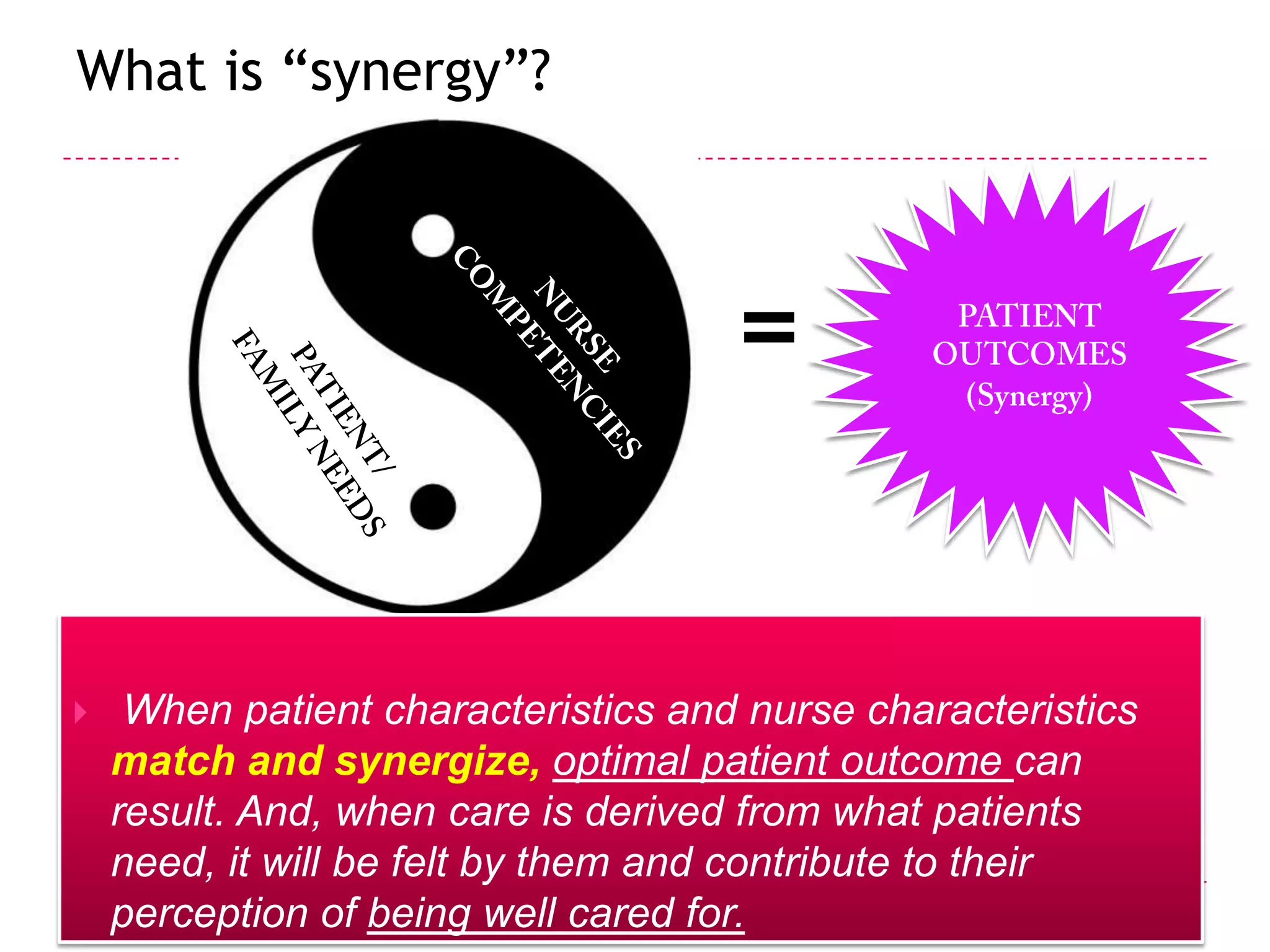
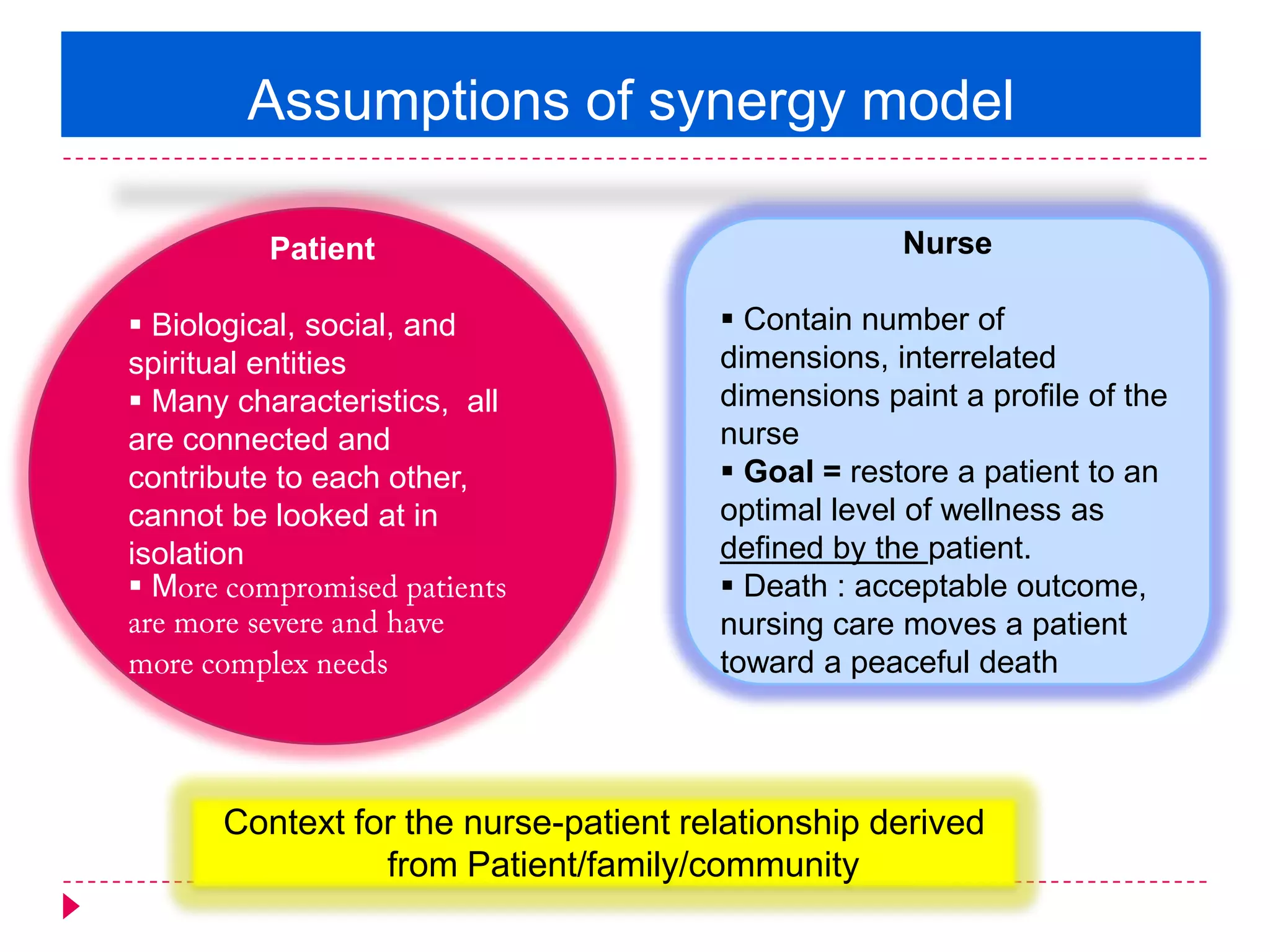
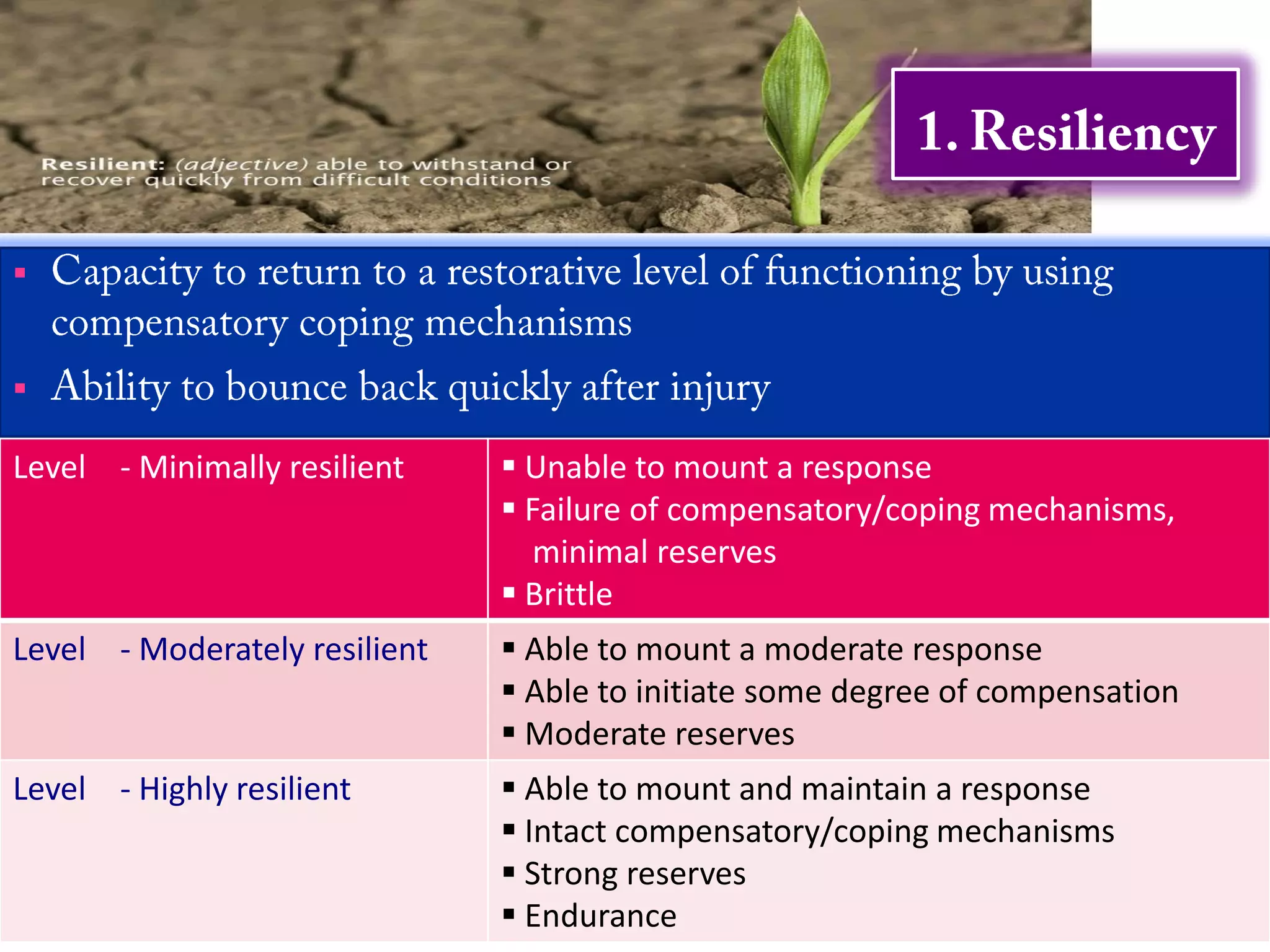
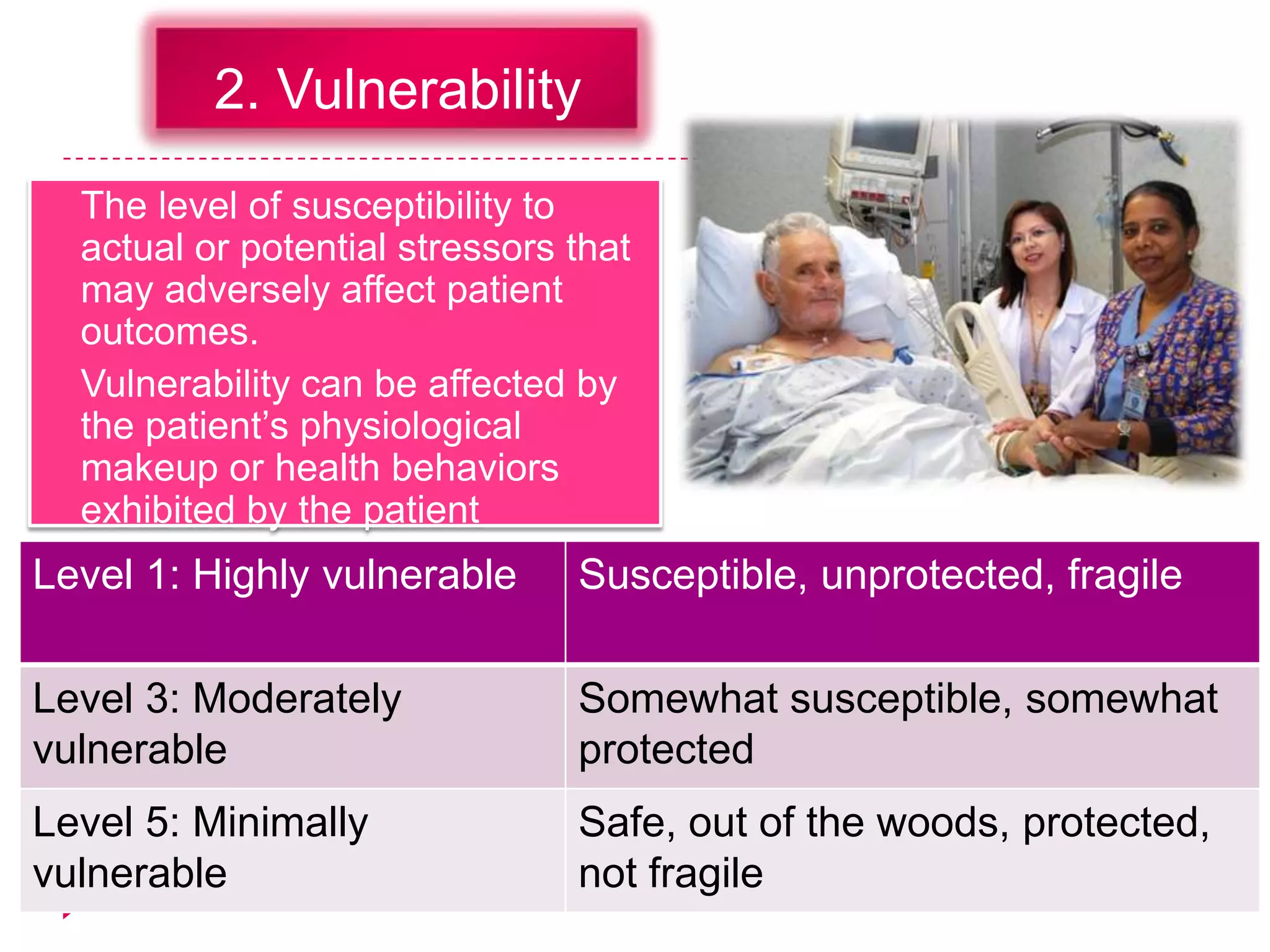
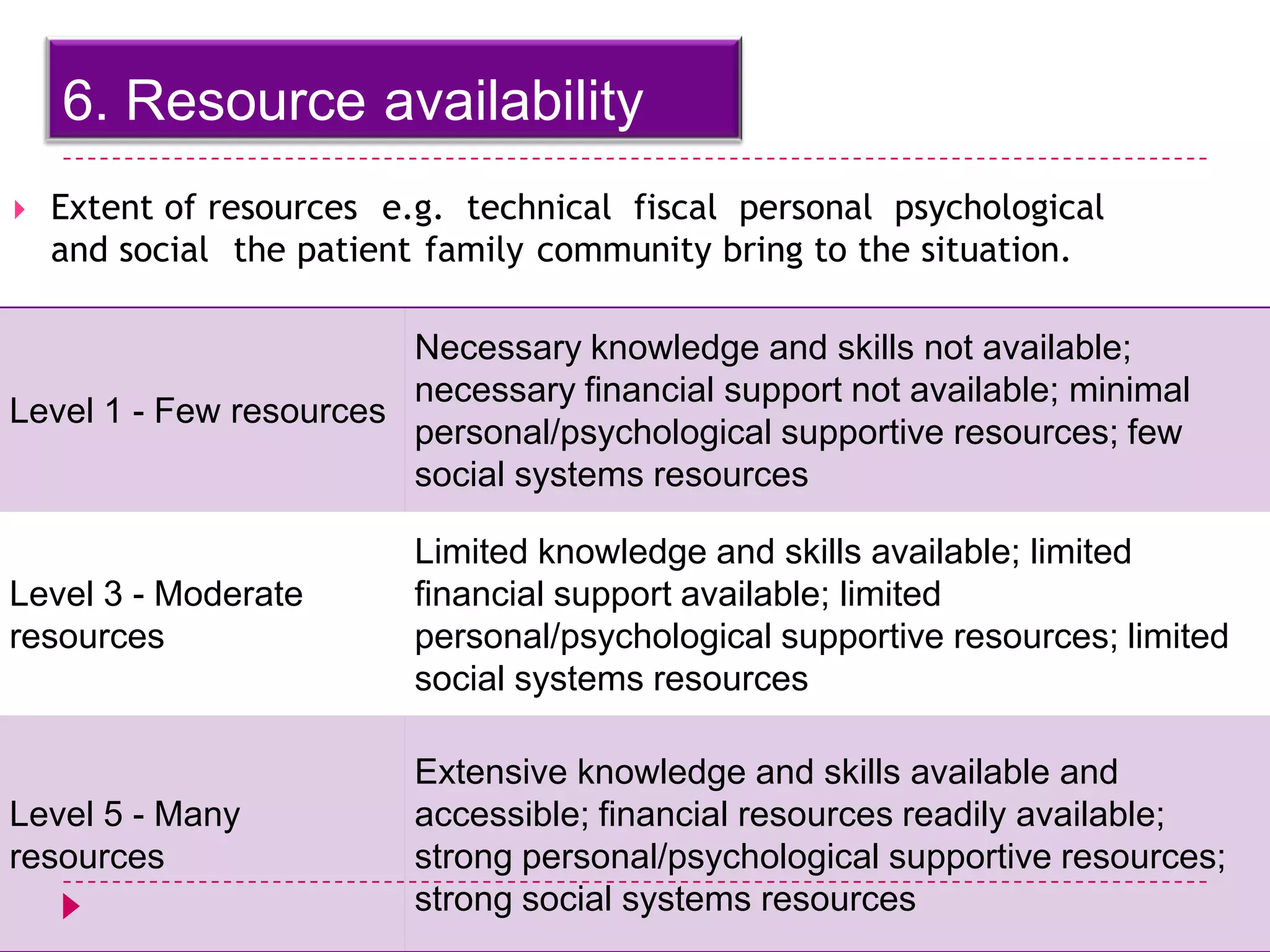
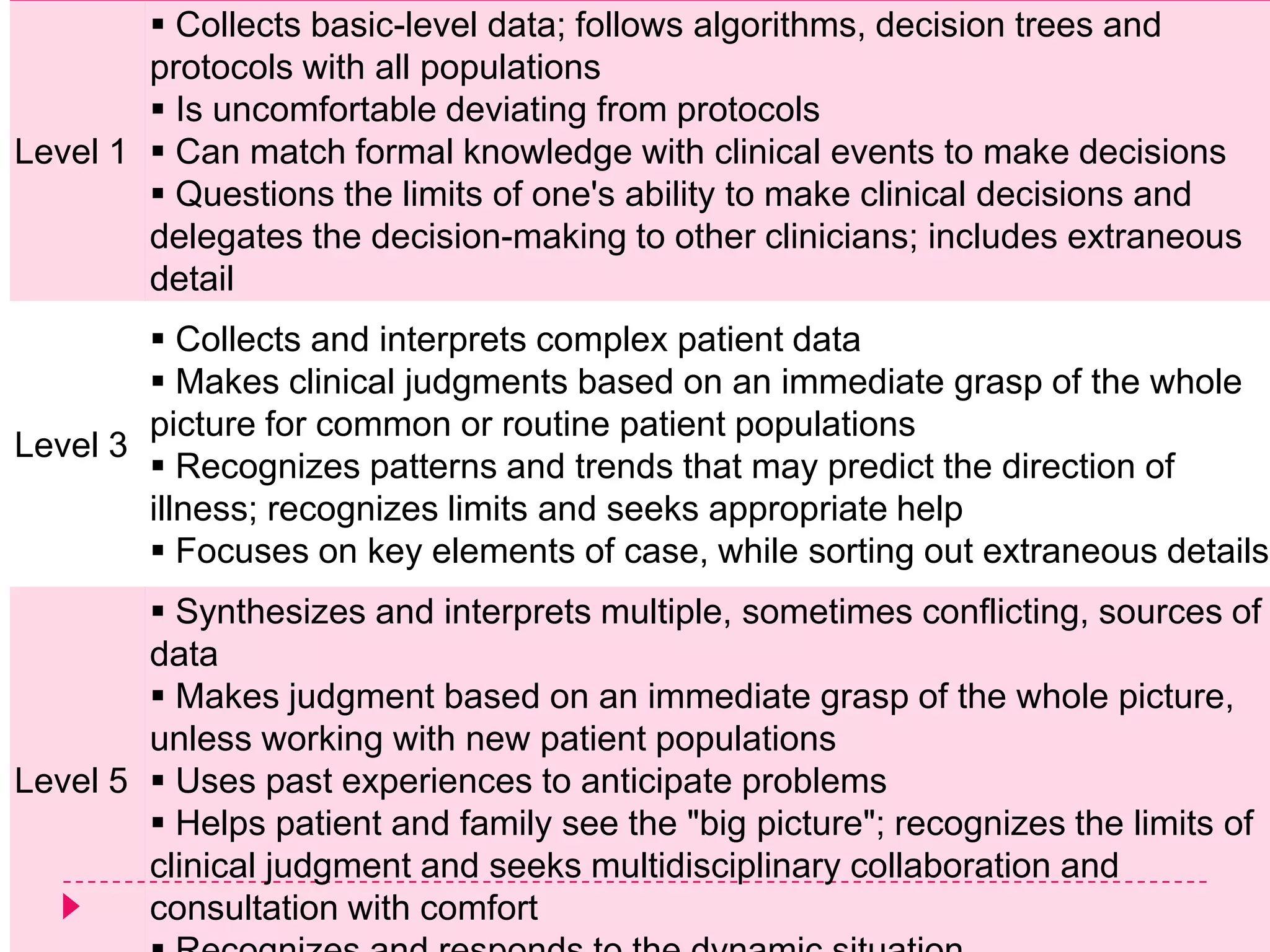
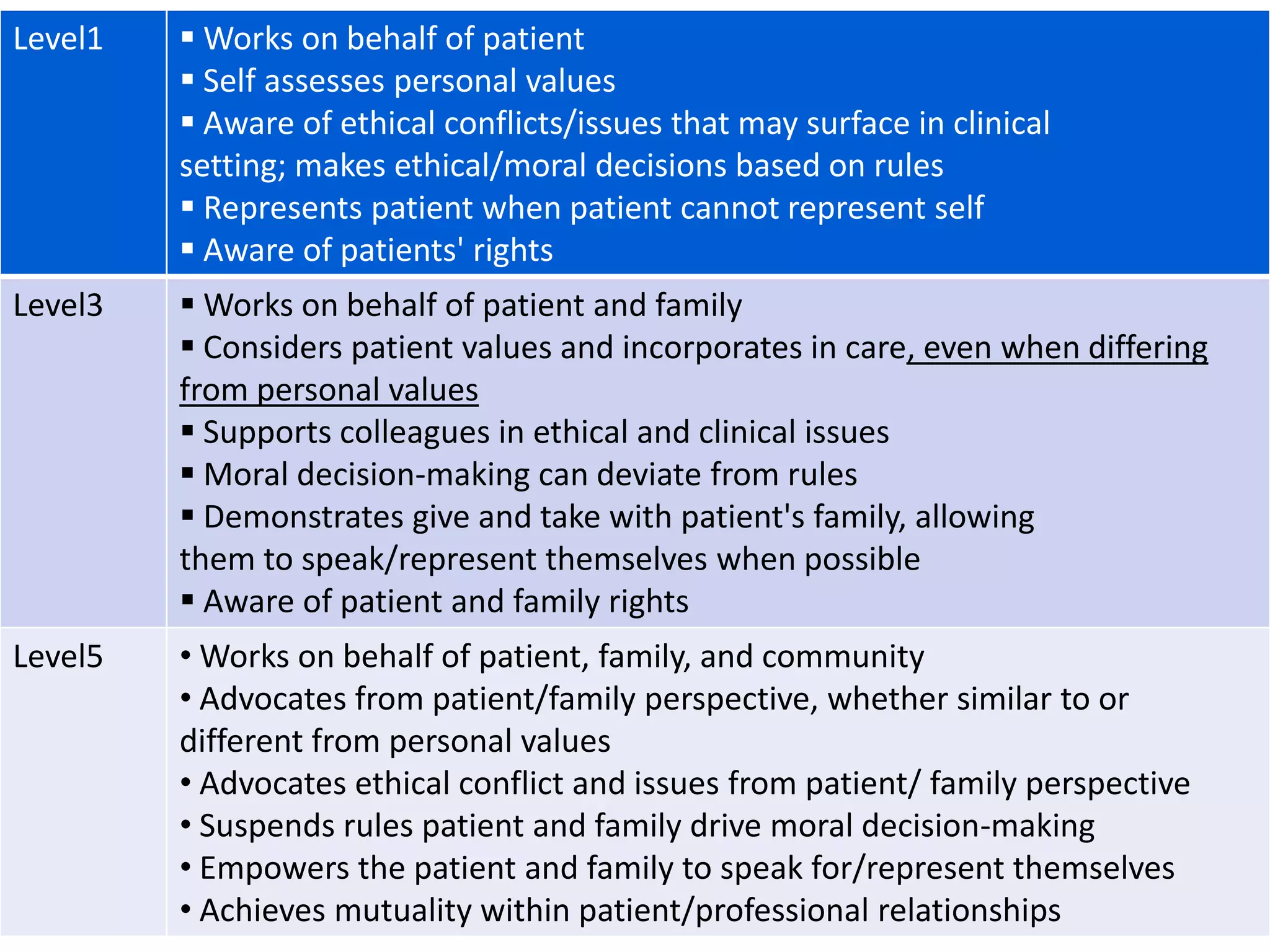
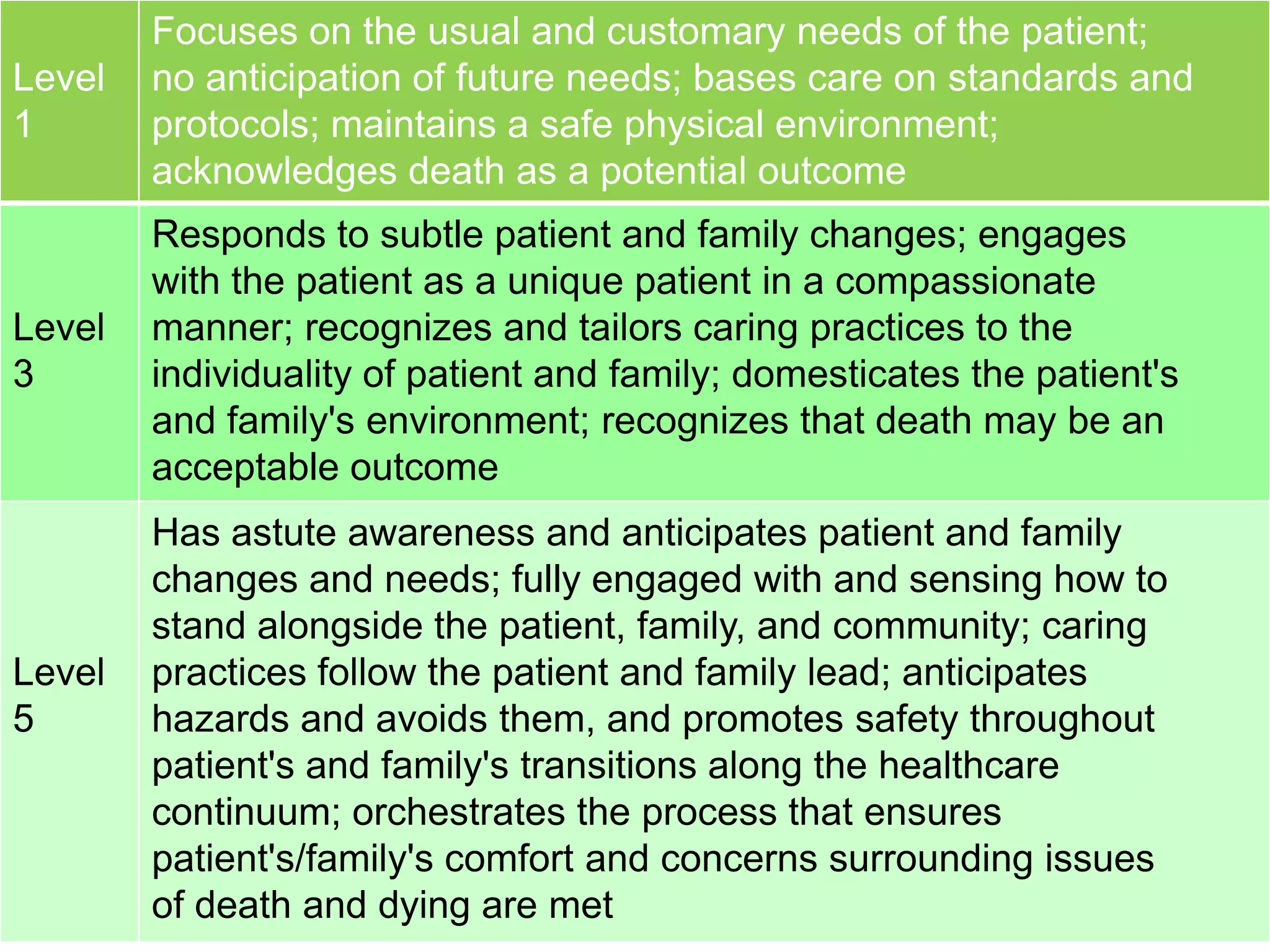
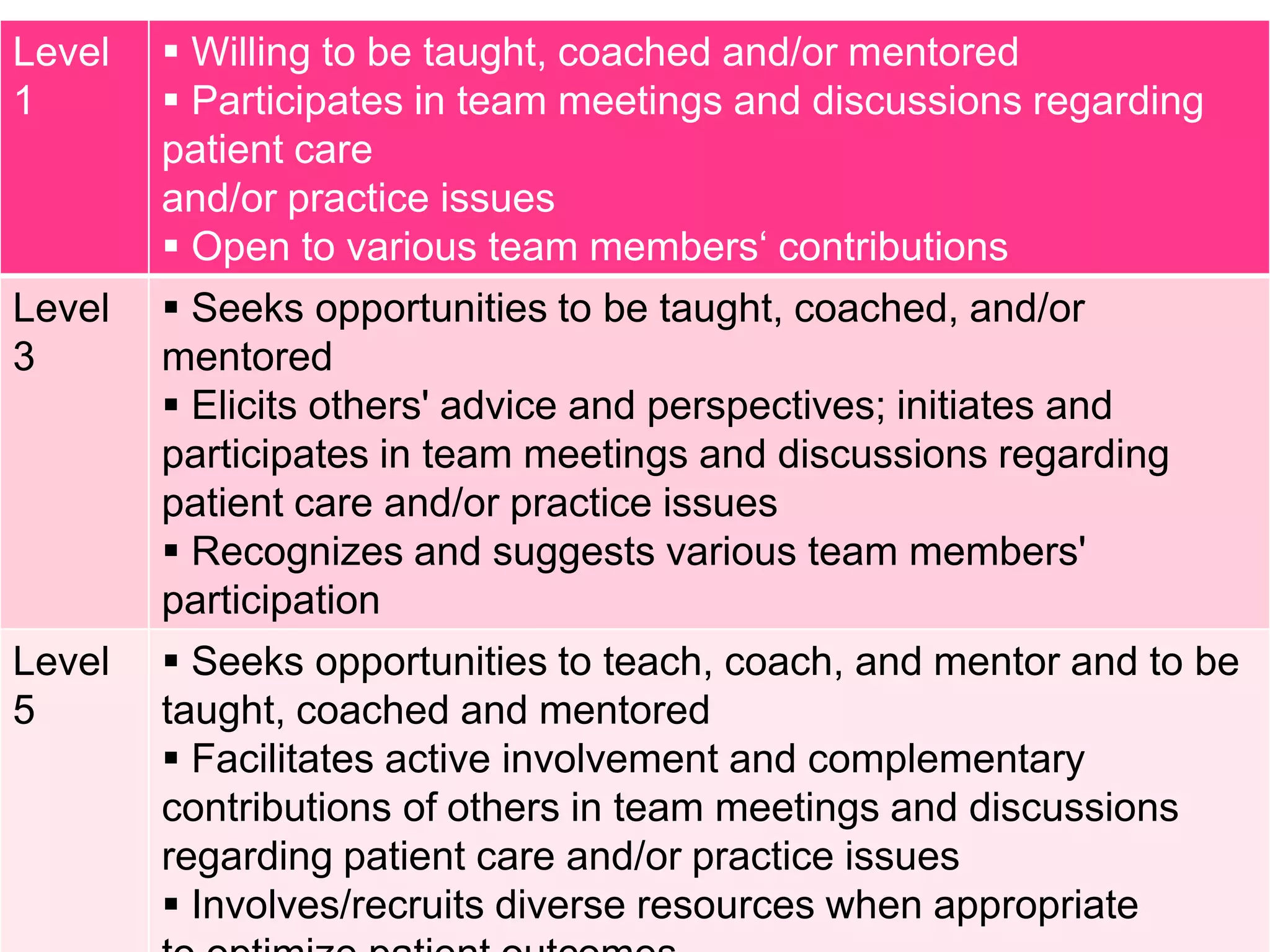
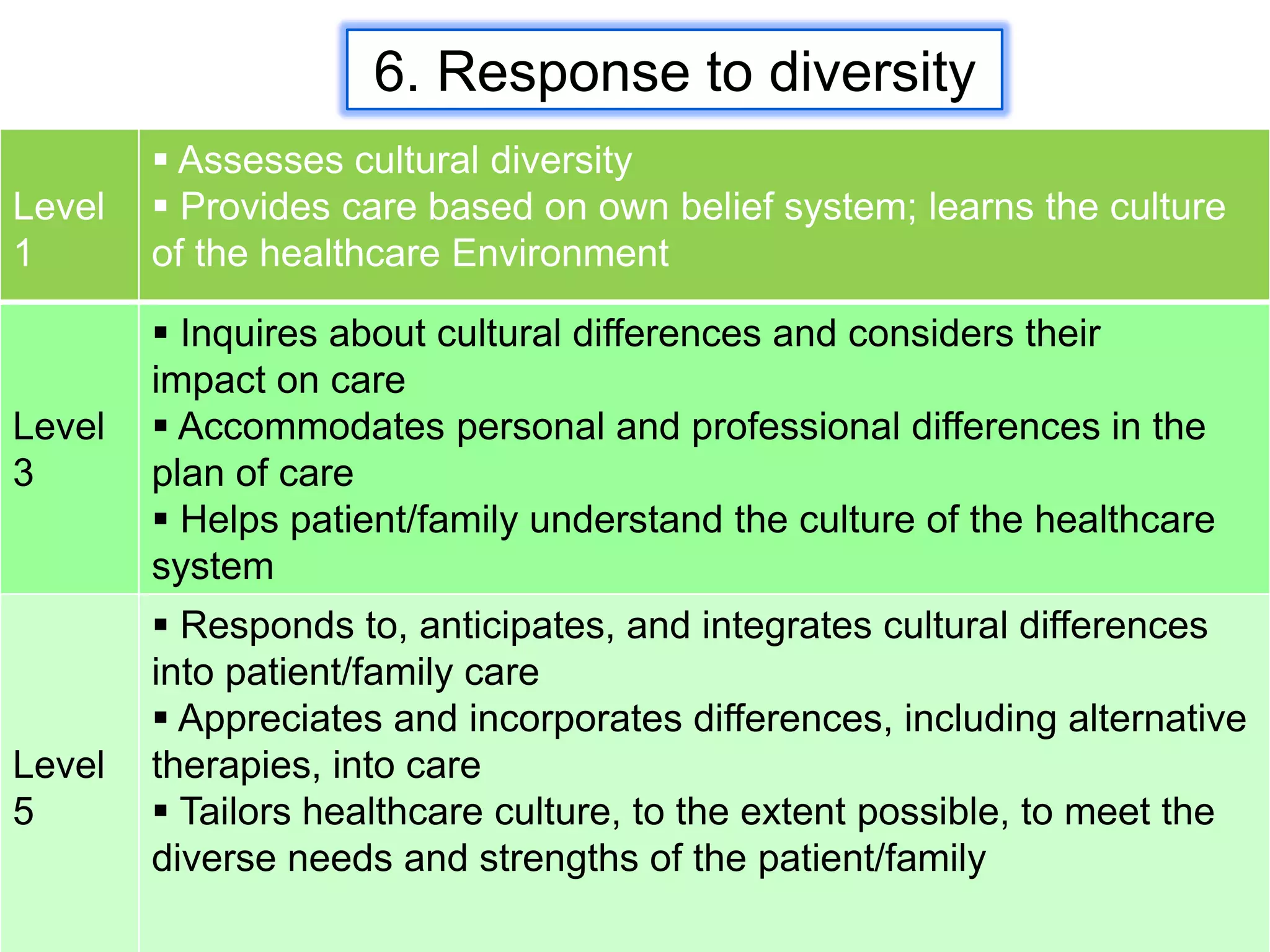
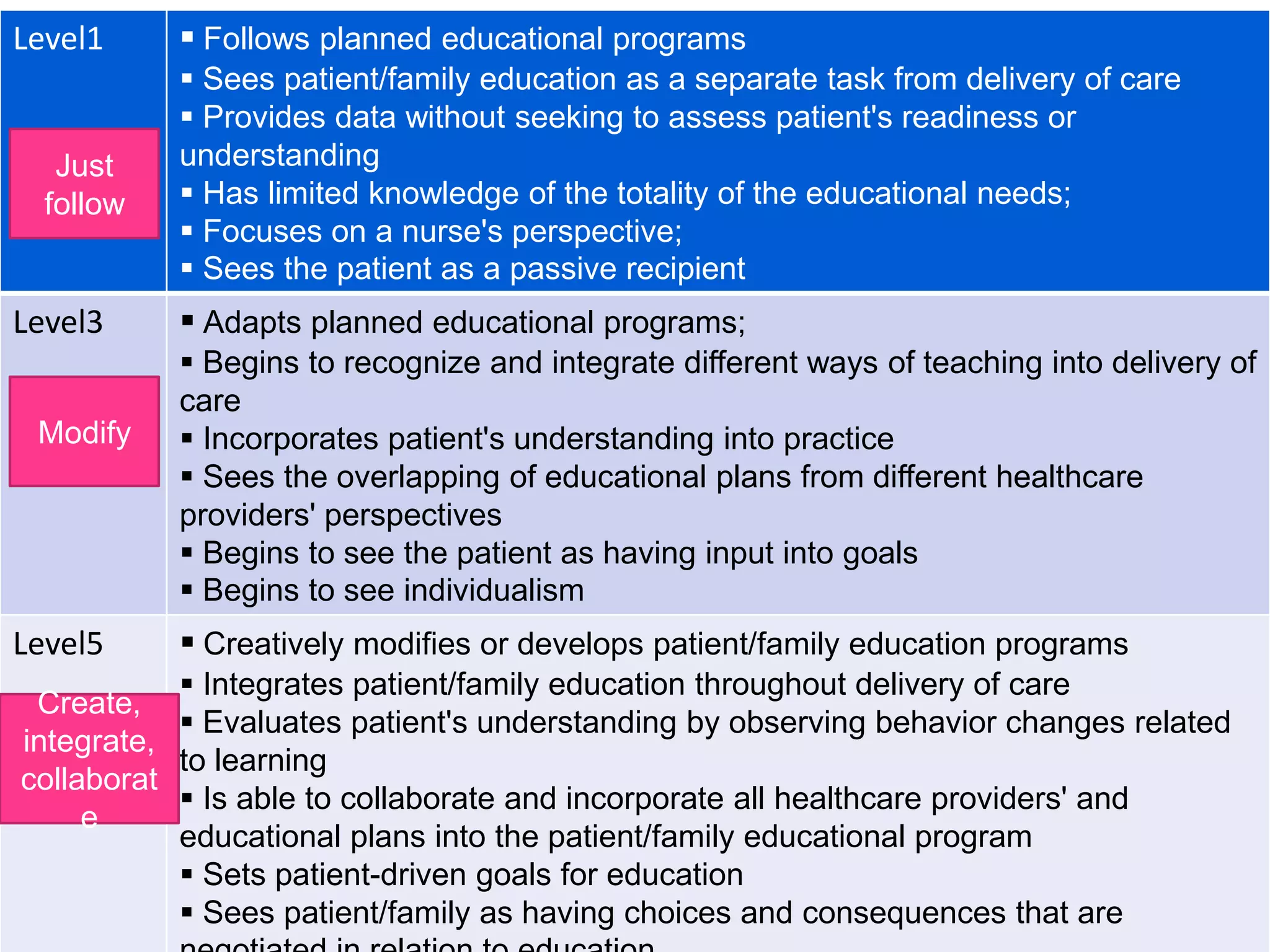
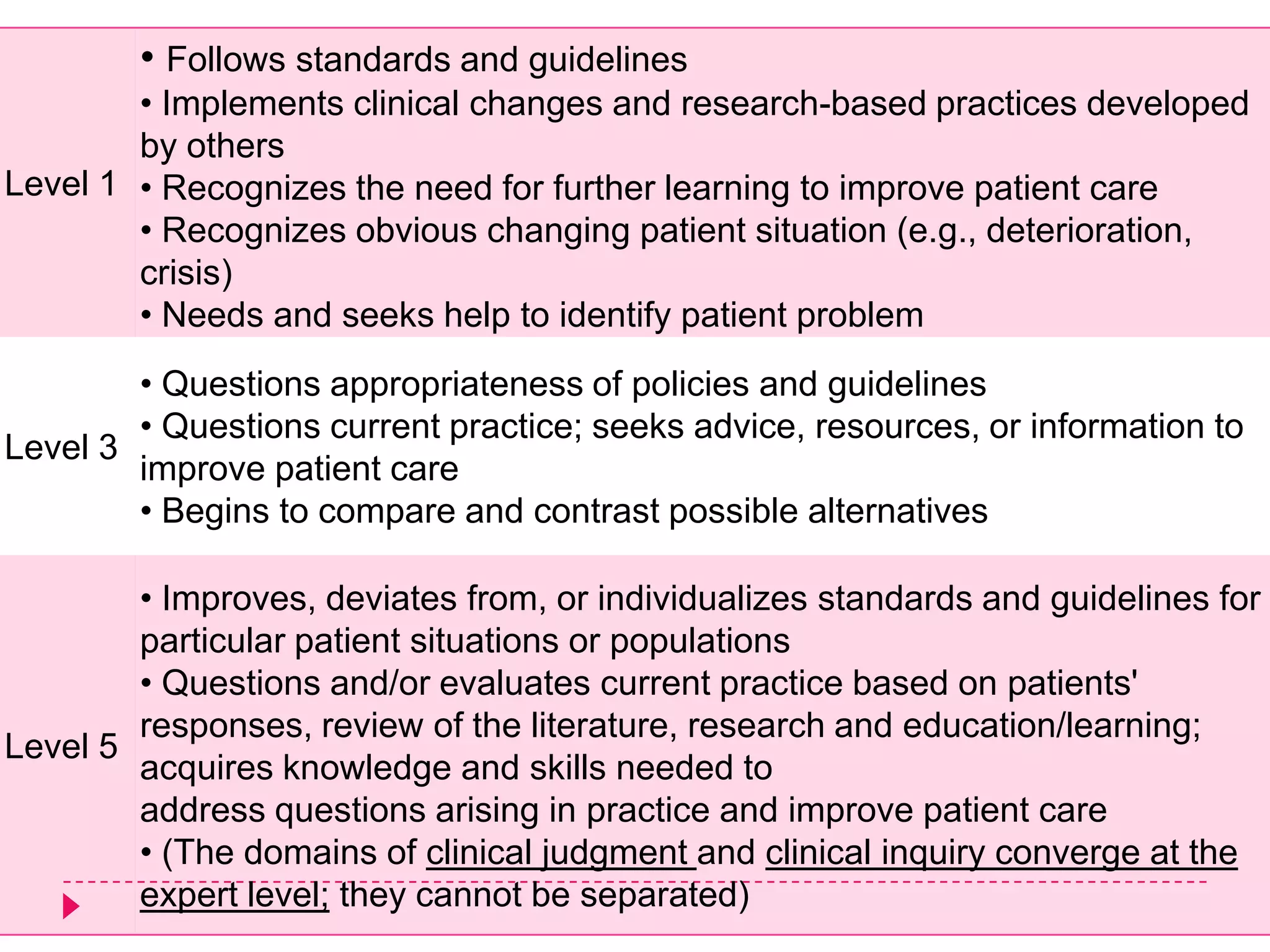
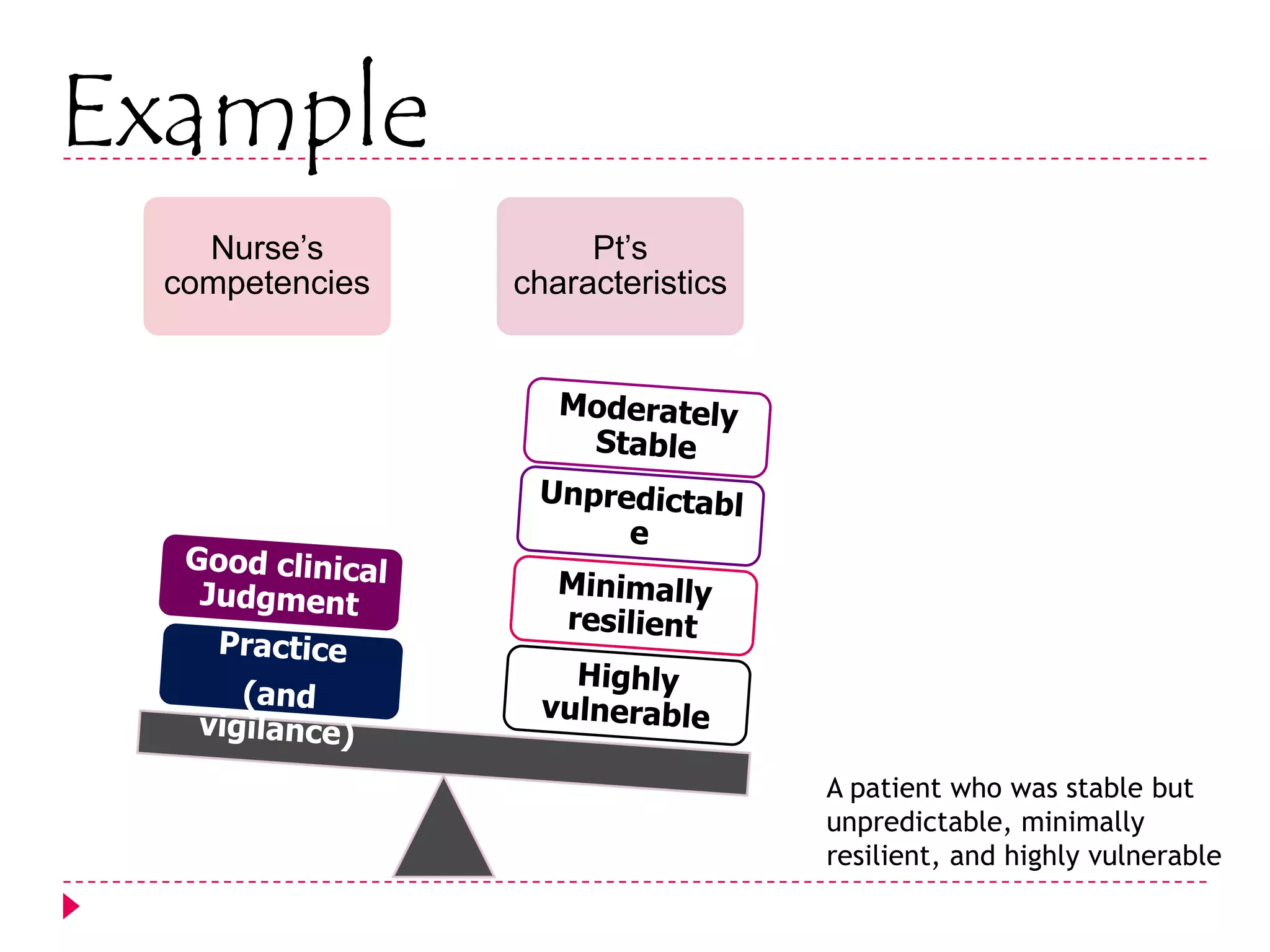
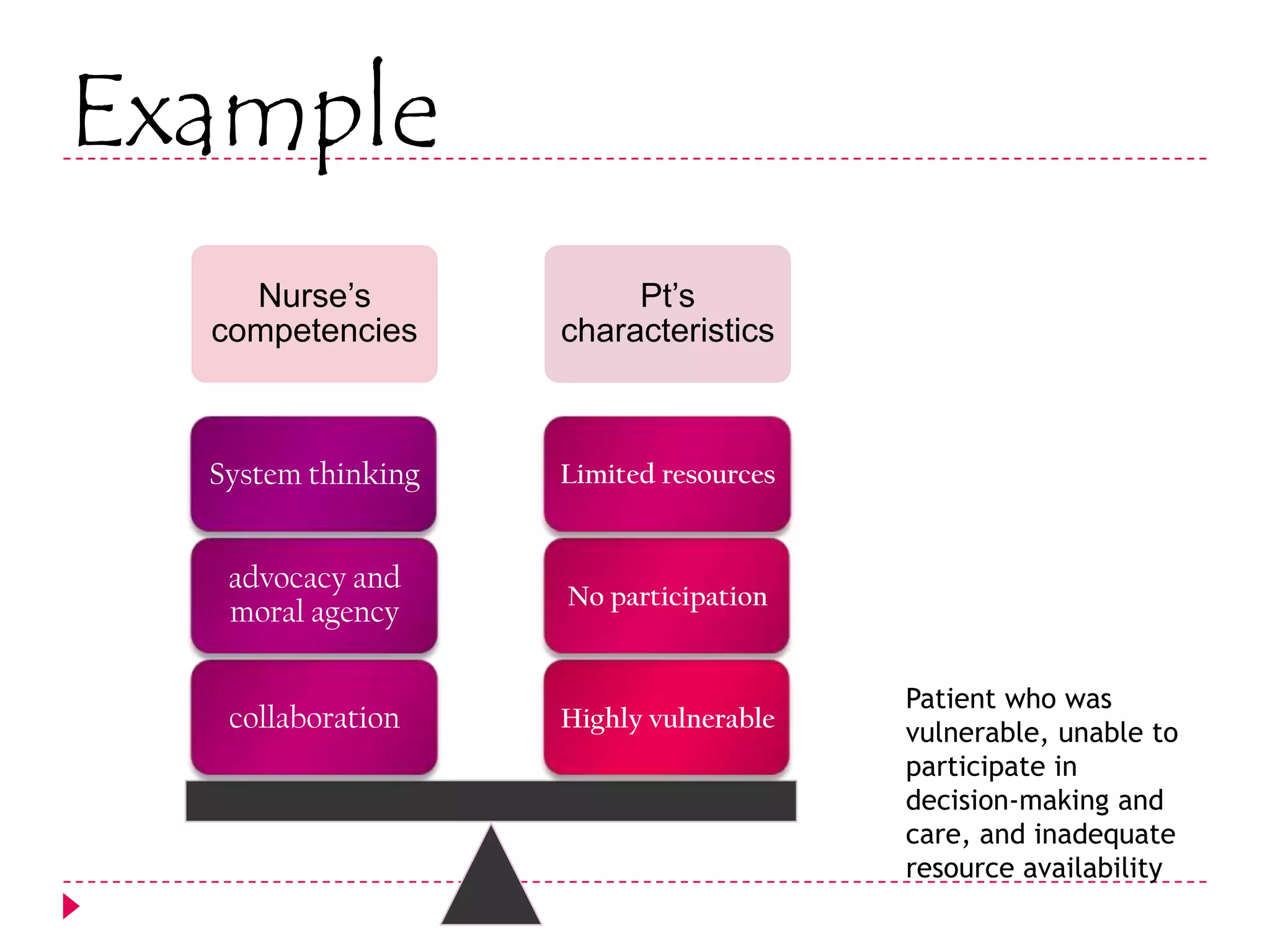
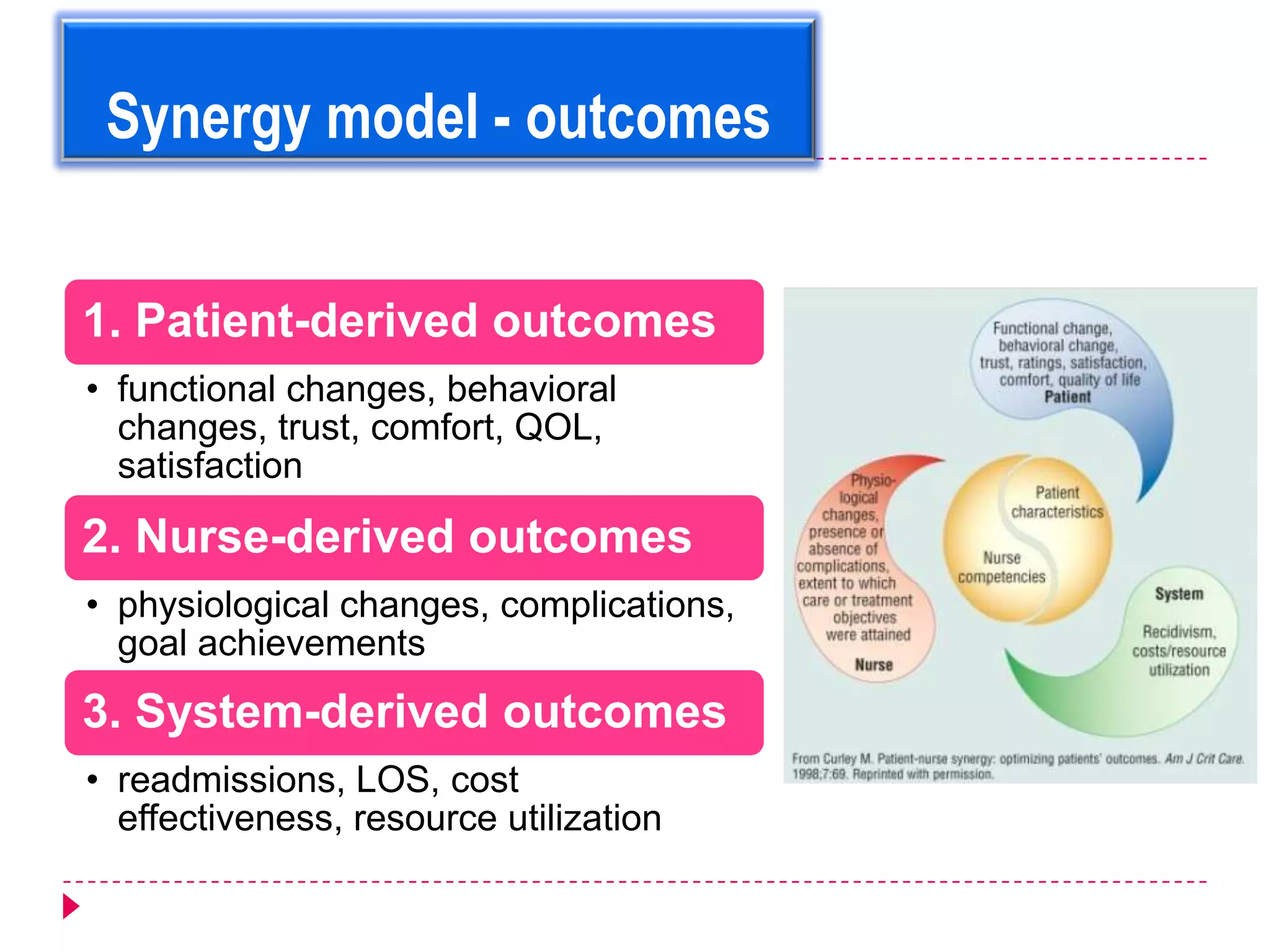
The AACN Synergy Model is a framework that matches patients' characteristics and needs with nurses' competencies in order to optimize patient outcomes. The model has 8 patient characteristics (resiliency, vulnerability, etc.) and 8 nurse competencies (clinical judgment, advocacy, caring practices, etc.) that are evaluated on a continuum. When patient needs and nurse competencies are well-matched, synergy occurs and the best outcomes can result. The document provides details on each of the patient characteristics and nurse competencies, including examples to illustrate where patients and nurses may fall on the various continua.