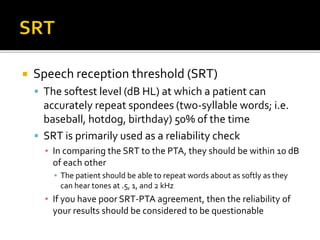
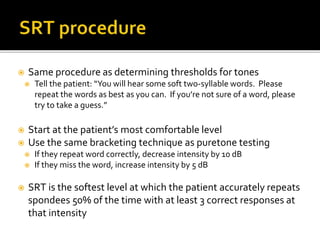
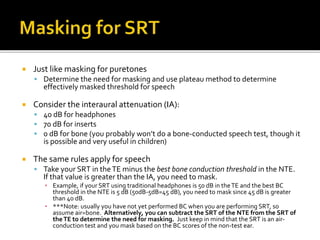
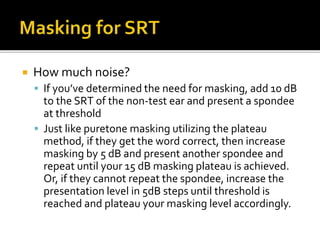
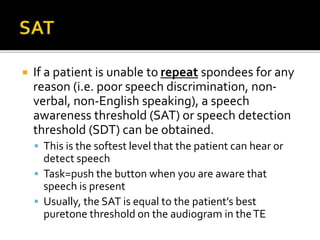
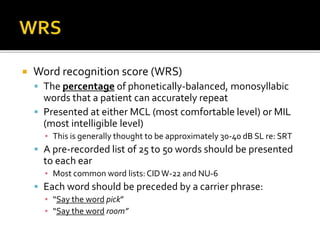
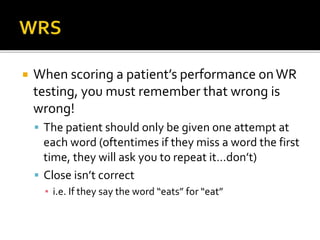
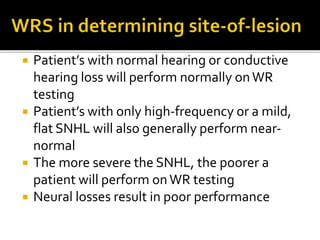
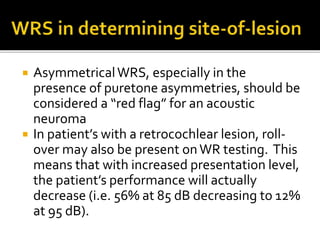
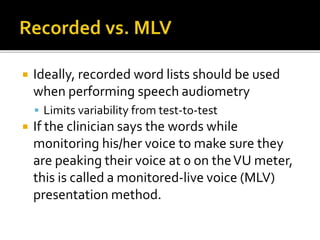
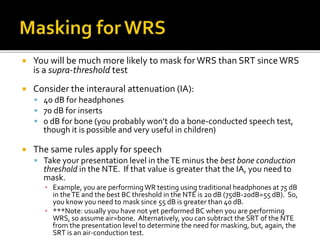
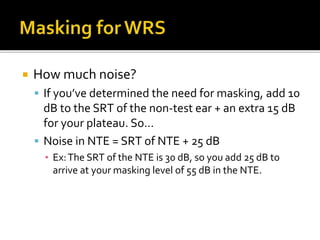
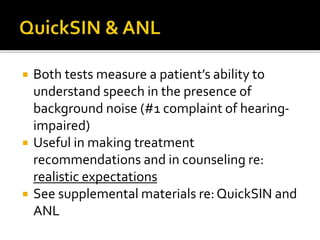
This document provides guidance on performing speech audiometry tests, including speech reception threshold (SRT), word recognition score (WRS), and speech-in-noise tests. It discusses procedures for determining SRT and WRS, considerations for non-native English speakers and those with hearing loss, and the clinical significance of test results including how they can indicate site of lesion. Masking procedures are also outlined to limit interference between ears during testing.