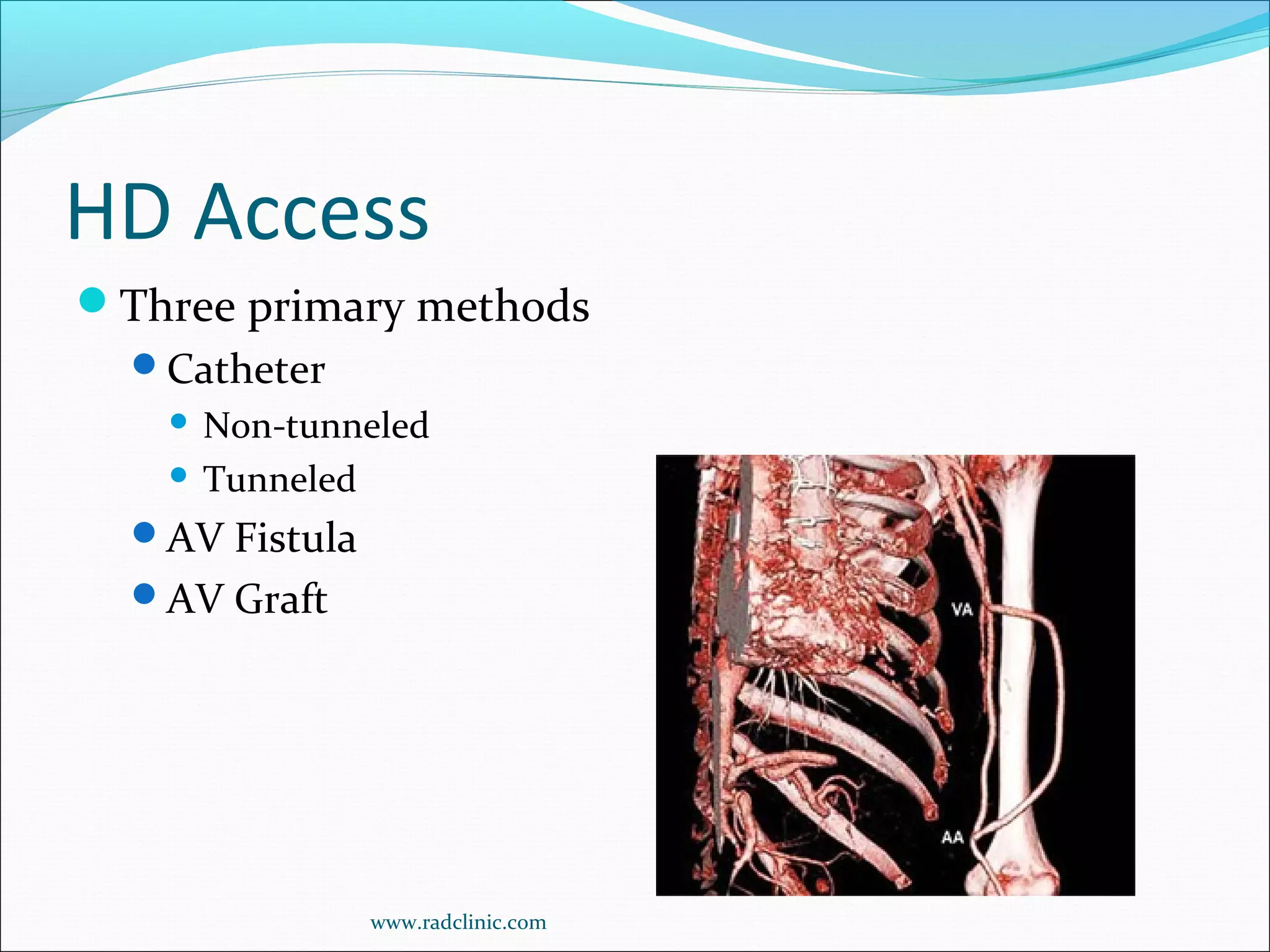
This document discusses arteriovenous (AV) access for hemodialysis, including fistulas, grafts, and catheters. It provides guidelines on creating and maintaining different types of access based on Kidney Disease Outcomes Quality Initiative (KDOQI) recommendations. Catheters are best for short-term use but carry higher infection risks than fistulas or grafts. Fistulas have the highest patency rates but take longer to mature than grafts. Early detection of access dysfunction through regular monitoring and treatment of stenoses is important to preserve access sites. Complications like infection, ischemia, and stenosis should be referred for imaging and intervention.