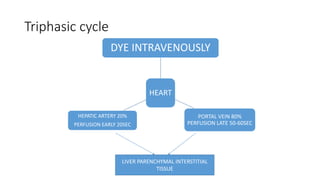
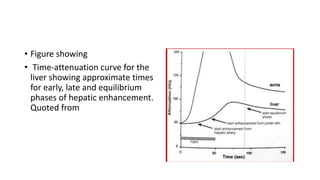
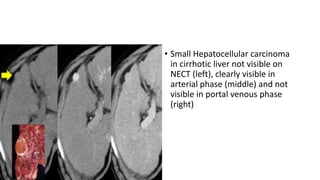
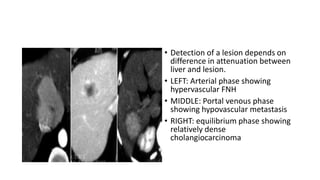
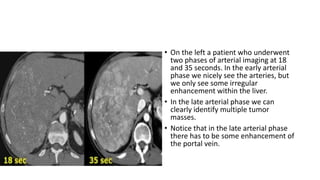
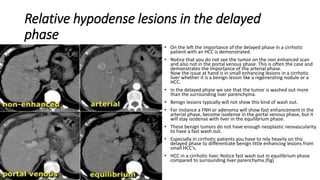
The document provides an overview of the principles and phases of hepatic contrast enhancement in triphasic CT scans, detailing how contrast agents affect the visibility of liver tumors based on their blood supply. It explains the significance of the arterial, portal venous, and equilibrium phases in detecting various types of lesions, including hypervascular and hypovascular tumors. Additionally, it outlines factors affecting characterization and diagnosis based on CT imaging patterns, highlighting the importance of contrast timing and injection rates.