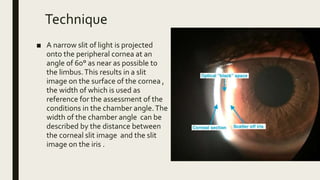
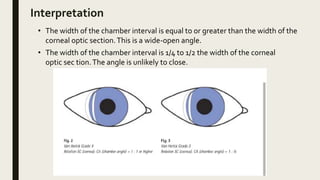
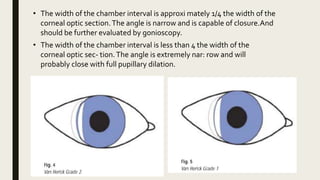
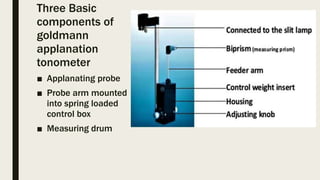
The document summarizes the Van Herick technique and Goldman applanation tonometry procedure. The Van Herick technique uses a slit lamp to estimate the angle of the anterior chamber without a gonioscopy lens. A narrow slit of light is projected onto the peripheral cornea and the width of the chamber angle is assessed. Goldman applanation tonometry uses a prism to flatten the cornea and measure the pressure needed to do so, relating it to intraocular pressure according to Imbert-Fick's law. A fluorescein-stained tear film outlines the flattened area which is used to take the measurement.