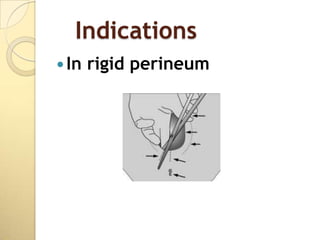
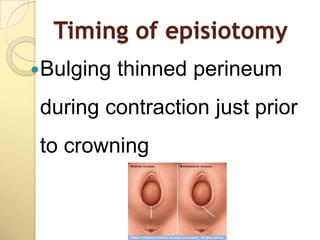
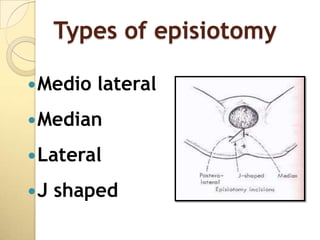
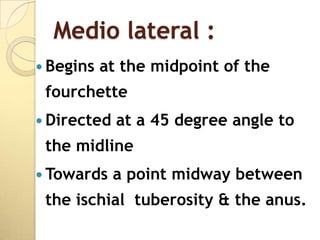
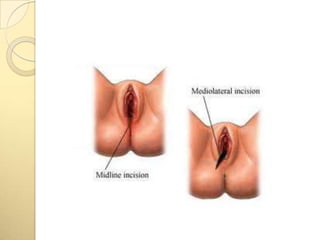
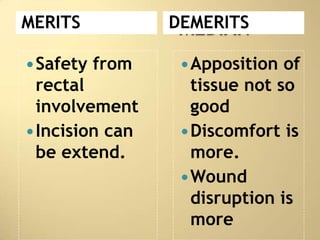
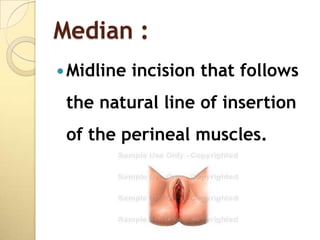
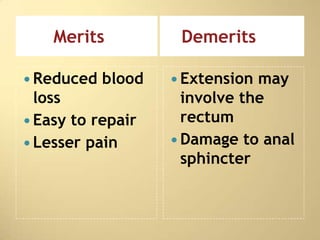
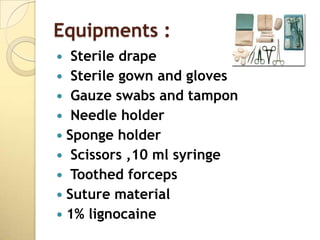
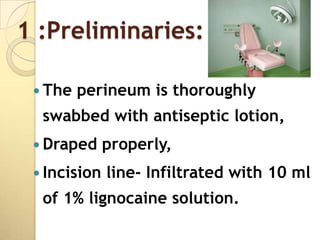
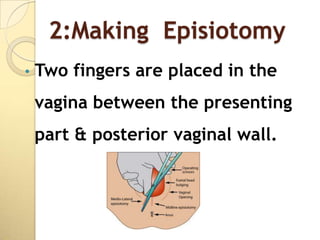
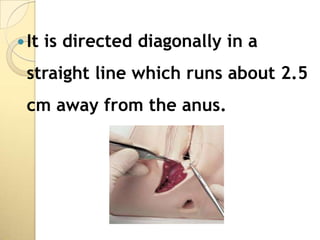
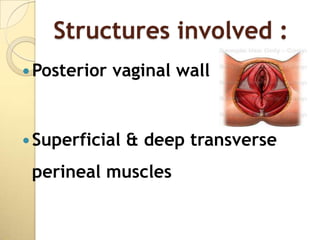
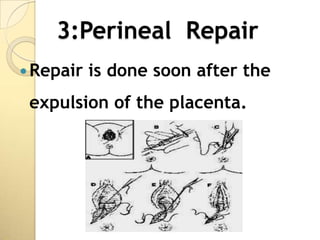
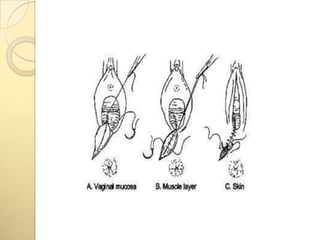
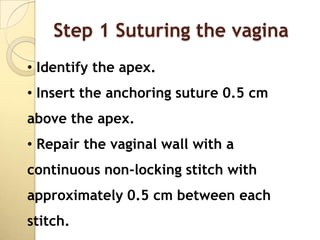
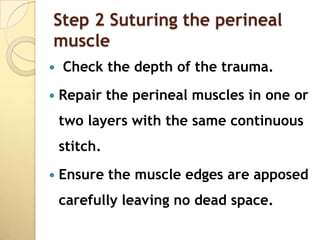
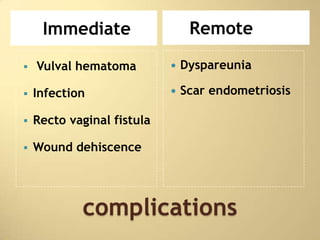
This document discusses episiotomy, including its definition as a surgically planned incision made during childbirth, purposes such as facilitating delivery and reducing perineal tearing, types (median, mediolateral, lateral), indications, advantages, repair process, post-operative care, and potential complications. The repair process involves suturing the vaginal mucosa, perineal muscles, and skin in layers to restore anatomical structure while controlling bleeding and preventing infection.