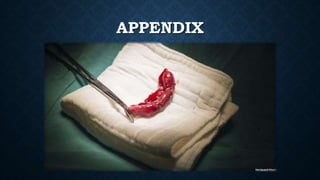
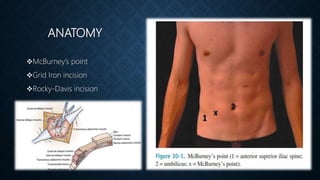
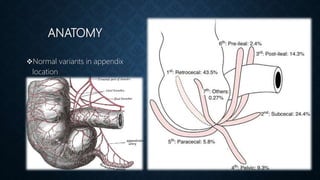
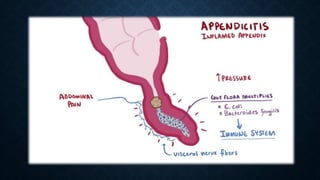
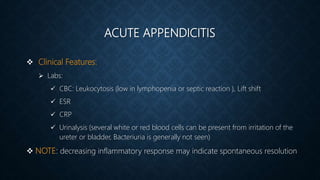
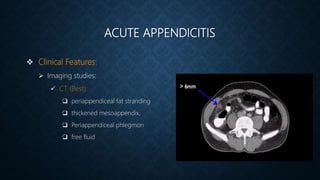
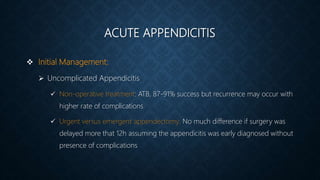
The document provides information on the appendix, including its history, anatomy, embryology, physiology, acute appendicitis, neoplasms, and variants. Some key points include: the appendix was first depicted by Leonardo da Vinci in 1492; acute appendicitis is caused by obstruction leading to distention and infection, with symptoms like migrating right lower quadrant pain; imaging like CT can help diagnose appendicitis; complications include perforation; and neoplasms like carcinoid tumors or adenocarcinomas can rarely affect the appendix.