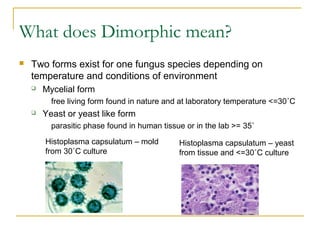
This document provides an overview of mycology, focusing on yeasts, molds, specimen collection and transport, culture media, and key pathogenic fungi such as Histoplasma capsulatum. Yeasts are unicellular and produce budding daughter cells, while molds are filamentous with hyphae that produce spores. A variety of specimens can be used for fungal culture. Important media include Sabouraud's agar and mycosel/mycobiotic agars. Dimorphic fungi like H. capsulatum exist in both mold and yeast forms depending on temperature. H. capsulatum causes histoplasmosis and has a small oval yeast phase. Identification methods for fungi include culture, microscopy
![Starting point
Molds are:
Filamentous with hyphae
Produce conidia [spores]
Colonies on solid agar are downy, fluffy,
cottony
Most mold colonies are pigmented which aid
in identification
hyphae
spores](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-3-320.jpg)
![Common Fungal Media
Mycosel/Mycobiotic agars
Selective SABS with chloramphenicol and cycloheximide
used for culture of dermatophytes – fungi that cause skin, hair and
nail infections
Brain heart infusion agar
Primary recovery of all fungal organisms
Can make it more selective by adding chloramphenicol and
cycloheximide
All fungal cultures must be incubated for 4 weeks at 30˚C
Lower temperature than bacterial culture incubation [35˚C]
If plates are used for fungal cultures the plates must be sealed with
air permeable tape for laboratory safety](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-6-320.jpg)
![Lactophenol cotton blue [LCB] adhesive tape preparations are
the standard method used for mold identification.
The LCB mounting medium consists of phenol
lactic acid, glycerol and aniline cotton blue dye.
Clear adhesive tape touches a mold colony, picking
up fungal hyphae and pressed into one drop of LCB
If LCB prep is not able to
identify a mold 16sRNA
sequencing can be used
to identify problematic
molds in reference
laboratories.
Mold Identification](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-9-320.jpg)
![Yeast cells stain blue [Gram positive]. Examine for
budding cells to confirm that it is a yeast cell and not
an artifact. Examination on oil immersion lens.
You can also detect pseudohyphae on Gram stain.
Mold can be difficult to identify on a Gram stain.
pseudohyphae
mold
pseudohyphae
Gram Stain](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-12-320.jpg)
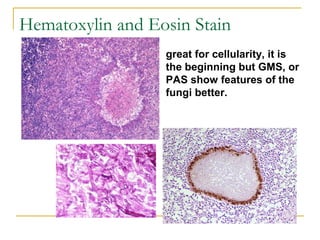
![Methenamine Silver Stain [GMS] –
yeast and hyphae stain grey to black.
Examine the hyphae for presence of septations in the
hyphae, broad or more narrow width and angle of branching.
Examine the size and budding pattern of observed yeast.
We will observe on later slides these criteria can assist in
identification.
Examination of fungi in fixed tissue](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-16-320.jpg)
![PAS-positive staining red against a
green or blue background
Periodic Acid Schiff [PAS]](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-17-320.jpg)
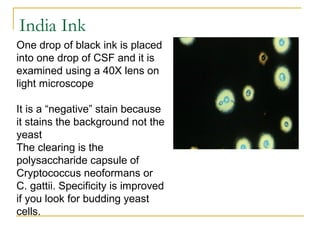
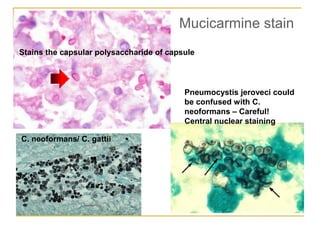
![Stain-Cryptococcus neoformans polysaccharide capsule
stains pink
Mucicarmine [Mucin] stain](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-18-320.jpg)
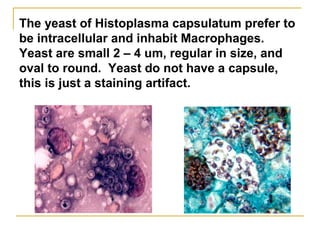
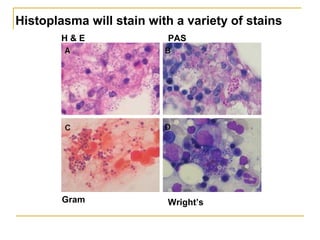
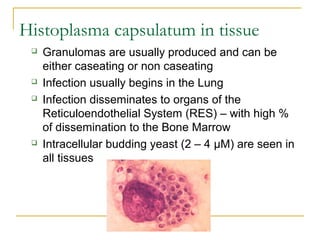
![Histoplasma capsulatum
Fungal Culture incubated at 30˚ C
Very SLOW growing taking 2 – 8 weeks to form colonies
Colony is white to brown and cottony
Microscopic appearance – tuberculated macroconidia that
are large and round (8 – 16 µM) plus small microconidia (2 -
4µM) [see picture]
Microconidia are the infectious particle growing in nature and
capable of penetrating deep into the lung
DNA probe must be used to confirm identification so there is
definitive identification
Sepedonium species looks somewhat like Histoplasma and
is considered a look a like fungus](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-28-320.jpg)
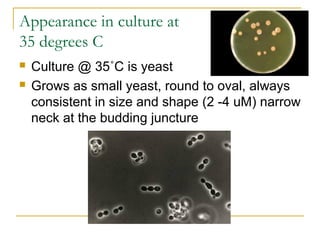
![Histoplasma capsulatum
culture at 30˚ C is white and
cottony.
Microscopic exam:
Tuberculate [projections]
macroconidia is the
structure used for ID.
Microconidia are the
infectious particle.
Appearance in culture at 30 degrees C](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-29-320.jpg)
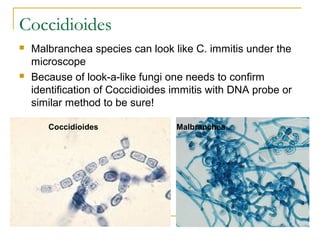
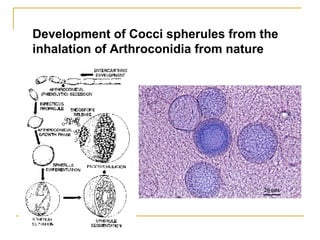
![Coccidioides immitis [posadasii]
Culture at 30˚C
Requires only 2 – 3 days to grow, colony starts waxy and
becomes wooly in around 7 – 10 days
Under the microscope one looks for foci of septated hyphae with
thick walled barrel shaped arthroconidia with clear spaces in
between. The clear spaces are dead arthroconidia.
Arthroconidia infectious particle in nature
Very infectious to laboratory personnel](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-40-320.jpg)
![Barrel shaped alternating arthroconidia are
produced in cultures grown at both 30 and 35 C.
There is no yeast phase for C. immitis [posadasii]
No yeast phase with Coccidioides!](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-42-320.jpg)
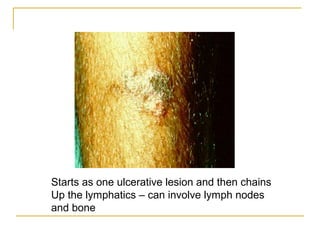
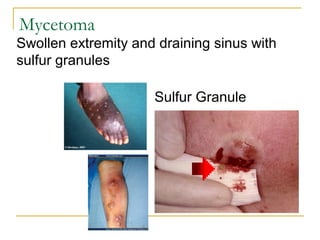
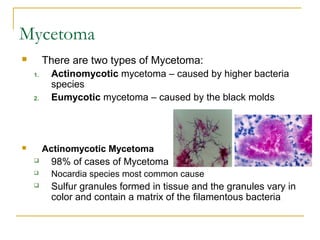
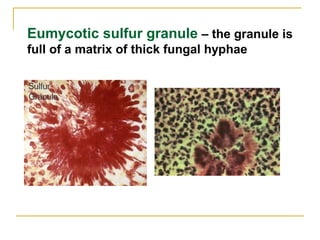
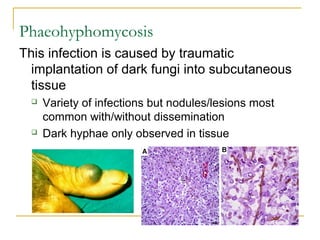
![Subcutaneous Fungal Infections
Most common will be described
Mycetoma [2 types]
Actinomycotic – caused by higher bacteria
Eumycotic – caused by dark pigmented molds
Chromomycosis [Chromoblastomycosis]
Phaeohyphomycosis
Sporotrichosis](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-57-320.jpg)
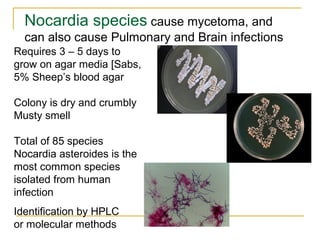
![Gram stain as filamentous Gram positive bacilli – can be
poorly staining and appear speckled.
Nocardia are positive [red] on the Modified Kinyoun stain.
Modified acid-fast stain
[modified Kinyoun stain]
Gram stain of sputum
containing Nocardia
Nocardia](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-61-320.jpg)
![Edge of granule has thin filamentous bacteria
for both bacteria – Nocardia is modified acid fast
[PAF] positive and is aerobic bacteria. Actinomyces
is PAF negative and grows anaerobically.
Beware! Sulfur granule
caused by Actinomyces
israelii looks identical.
Actinomycotic sulfur granule - Nocardia](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-62-320.jpg)
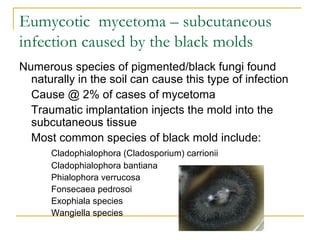
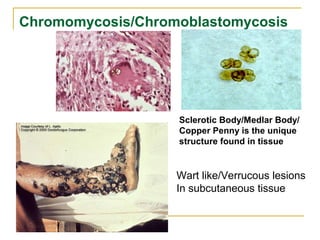
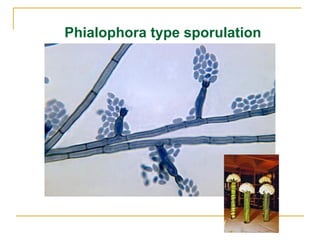
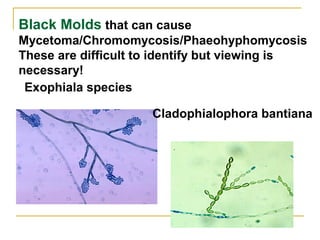
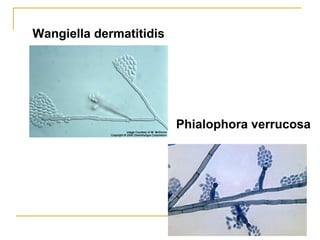
![Chromomycosis/Chromoblastomycosis
Three characteristics describe Chromomycosis
Wart like lesions in subcutaneous tissue
Sclerotic bodies observed in tissue
Growth of dark/pigmented fungi
Black mold naturally found in the soil cause
infection through abrasion/ implantation
Black molds that can cause Chromomycosis:
Cladophialophora [Cladosporium] carrionii
C. bantiana
Phialophora verrucosa
Fonsecaea pedrosoi
Exophiala species
Wangiella species](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-66-320.jpg)
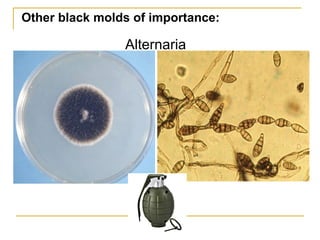
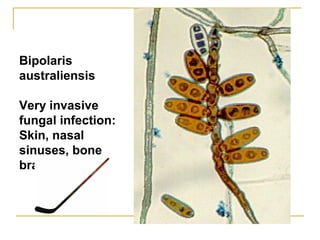
![Black molds/Dark molds
also known as Dematiaceous
fungi
Black colored colonies and the
reverse [back of colony] is also
black
Naturally brown hyphae and
spores
One of the major causes of mold
growth due to water damage!](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-70-320.jpg)
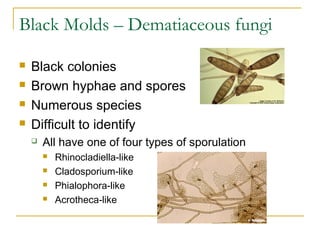
![Cladophialophora
[Cladosporium type sporulation]](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-74-320.jpg)
![Exserohilum rostrum
Associated with compounded pharmaceutical
[steroid] products contaminated with dust/dirt
Used for infections into lumbar spine and
knee joints for pain management
Meningitis
Spinal abscess
Synovial infections](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-81-320.jpg)

![Cryptococcus gattii – a closely related
relative of C. neoformans
Isolated from forested area of the Pacific Northwest
(British Columbia, Washington, and Oregon)
Infection of normal and immune suppressed hosts
Mostly Pulmonary disease [Cryptococcoma] but can
develop meningitis
Culture and staining identical to C. neoformans except
for L Canavanine glycine bromthymol blue medium –
C](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-92-320.jpg)
![Microsporum canis
Main cause of ringworm from dog and cat
White colony/ yellow on backside of colony
Tuberculate macroconidia [spiny projections]
Few if any microconidia](https://image.slidesharecdn.com/oslerbacteriologyiandii2013new-130908231032-/85/MYCOLOGY-REVIEW-102-320.jpg)