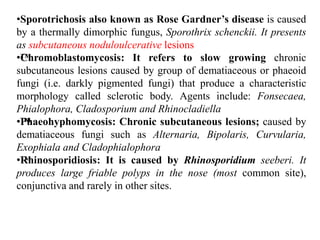
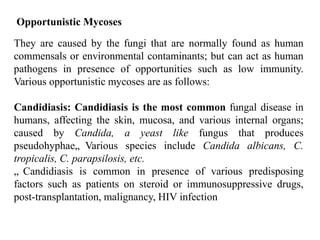
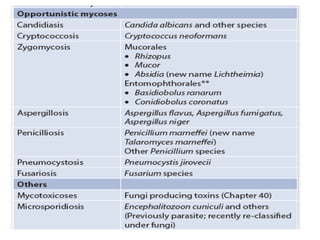
Medical mycology focuses on fungi that affect human health and classifies them into groups such as yeasts, molds, and dimorphic fungi. Important diagnostic methods include microscopy, culture, and immunological tests to identify various fungal infections, which can be superficial, subcutaneous, systemic, or opportunistic mycoses. Treatment and identification require an understanding of both the organism's morphology and its clinical presentation.