Hydrops fetails for undergranuate
- 1. Hydrops Fetalis Dr Manal Behery 2014
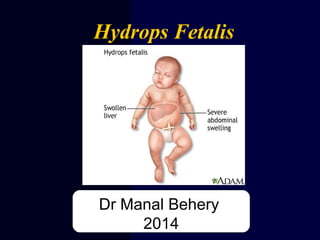
- 2. Hydrops = Generalized subcutaneous edema in the fetus or neonate
- 3. Definition 1. Excess serous fluid in at least one space (ascites, pleural effusion, or pericardial effusion) + skin edema (> 5 mm thick) 1. Excess fluid in two spaces without edema
- 4. Hydrops Fetalis Non Immune Hydrops Fetalis (90%( Immune Hydrops Fetalis (10%(
- 5. Etiology 1. Hematologic: Due to anemia (10% of cases) : A. Isoimmune hemolytic disease (RH incompatibility). 2.Cardiovascular: Due to heart failure (20% cases) A. Rhythm disturbances B. Major cardiac disease
- 6. 3. Infection (10% of cases) TORCH-Syphilis- Congenital Hepatitis, Parvovirus…. 4. Chromosomal (5% of cases) : Turner syndrome, trisomy 13,18,21
- 7. 5. Pulmonary (5% of cases) Chylothorax, diaphragmatic hernia 6. Gastrointestinal (5% of cases) : Meconium peritonitis 7. Renal (5% of cases) Nephrosis, RVT, urinary obstruction …..
- 8. 7. Maternal conditions (5% of cases) : Toxemia, diabetes, thyrotoxicosis 8. Miscellaneous (10% of cases) : Cystic hygroma, wilms’ tumor – teratoma 9. -Unknown (20% of cases) :
- 10. Four blood types ( A, B, AB, and O) Each blood type is additionally classified according to the presence or absence of the Rh factor
- 11. CDE (Rhesus) System • Clinically Important • Includes c, C, D, e, E • Rh negative status indicates the absence of D antigen • 87% of Caucasians carry the D antigen
- 12. •Rh Disease •Alloimmunization •Isoimmunization •HDFN •Erythroblastosis Fetalis Confusing Terminology
- 13. When the mother produces Abs directed against fetus RBC surface Ag. Isoimmunization
- 14. Rh Incompatibility Exposure to fetal antigens causes the mother to produce antibodies
- 15. The placenta usually acts as a barrier to fetal blood entering the maternal circulation.
- 16. Fetal cells can enter the maternal circulation through a “break” in the “placental barrier”.
- 17. Maternal production of Rhesus antibodies following introduction of Rhesus positive blood
- 18. Maternal production of Rhesus antibodies following introduction of Rhesus positive blood
- 19. Causes of RBC Transfer: “A break in the barrier” • Abortion/Ectopic Pregnancy • Partial molar pregnancy • Blighted ovum • Antepartum bleeding • Procedures (amniocentesis, cordocentesis, CVS) • External version • Platelet transfusion • Abdominal trauma • Inadvertent transfusion Rh+ blood • Postpartum (Rh+baby)
- 20. Sensitized pregnancy Non- Sensitized pregnancy Rh Incompatibility Sensitization = Rh neg person exponsed to the Rh (D) antigen and makes antibodies against that protein (antigen).
- 21. Rh Negative Women Man Rh positive ⇓ Fetus Rh positive Fetus → Rh+ve R.B.C.s enter Maternal circulation⇐ previously sensitized 2nd immune response IgM…IgG antibodies ⇓ Non sensitized Mother Primary immune response 1st Baby usually escapes. Mother gets sensitized? ± Fetus Haemolysis ⇓ Pathogenesis Of Rh Iso - immunisation Rh –VE Fetus no harm
- 22. Presentation Mild jaundice Erythroblastosis Fetalis Generalized Edema Hepatomegaly Ascites
- 23. Natural History •50%of affected infants have mild anemia, requiring either phototherapy or no treatment. •25%have hepatosplenomegaly , moderate anemia and progressive jundice ending in kernicterus, neonatal death •25%are hydropic and die in utero or in the neonatal period
- 24. RhoGAM has decreased HDFN caused by anti-D Give 300 mcg dose within 72 hrs of delivery to unsensitized Rh (-) women (Rh positive infant) • ACOG: 300 mcg at 28 weeks UNLESS father known to be Rh (-)
- 25. Mechanism of action • Administered antibodies will bind the fetal Rh- positive cells • Spleen captured these cells by Fc-receptors • Suppressor T cell response is stimulated • Spleen remove anti-D coated red cells prior to contact with antigen presenting cells “antigen deviation”
- 26. Kleihauer-Betke Test • % fetal RBC in maternal circulation • Fetal erythrocytes contain Hbg F which is more resistant to acid elution than HbgA so after exposure to acid, only fetal cells remain & can be identified with stain • 1/1000 deliveries result in fetal hemorrhage > 30ml • Risk factors only identify 50%
- 28. 1.1-Direct Coomb’s Test (DAT( Detects RBCs that have already been sensitized with IgG Demonstrates that in vivo coating of RBC by Ab has occurred but does NOT identify the antibody Deepa Babin @TMC Kollam 28
- 29. Detects antibodies to RBC antigens present in the patient’s serum Detects in vitro red cell sensitization if red cells contain antigen corresponding to serum antibody Procedure: STEP 1: patient’s serum (with unknown Ab) + RBC (with known Ag) STEP 2: product of step 1 + Coomb’s reagent IAT((2. Indirect Coomb’s Test Deepa Babin @TMC Kollam 29
- 30. Recognition of pregnancy at risk •First ante-natal visit check blood group, antibody screening. • If indirect coombs test is positive, the father’s Rh should be tested. • Serial maternal Anti D titers should be done every 2- 4 weeks. • If titer is less than 1/16 the fetus is not at risk. • If titer is more than 1/16 then severity of condition should be evaluated.
- 31. Prevention • Test for excessive fetal-maternal hemorrhage after blunt trauma, abruption, cordocentesis, and bleeding with previa • Give RhoGAM for partial molar pregnancy, ectopic, chorionic villus sampling, amniocentesis, external version
- 32. MCA Doppler and Fetal Anemia • Fetuses with anemia show an • increased peak velocity of systolic blood flow in MCA. • MCA Doppler is also used to follow fetal response to intrauterine transfusion and to assist in timing subsequent transfusions. • Non-invasive, • no risk for worsening isoimmunization
- 33. Normal and Abnormal MCA Dopplers
- 34. Amniocentesis - There is an excellent correlation between the amount of bilirubin in amniotic fluid and fetal hematocrit. - • - Perform serial amniocenteses • to the optical density deviation at 450 nm measures the amniotic fluid unconjugated bilirubin. • Plot values on Liley Curve at 16 weeks of gestation
- 35. Liley Curve •Measures the level of bilirubin and predicts severity of hemolytic disease after 27 weeks
- 36. Suggested management after amniocentesis for ΔOD 450 Serial Amniocentesis Lily zone I Lower Zone II Upper Zone II Zone III Hydramnios & Hydrops Repeat Amniocentesis every 2-4 weeks Delivery at or near term Repeat Amniocentesis in 7 days or FBS Hct < 25% Hct > 25% Intrauterine Transfusion Repeat Sampling 7to 14 days <35to 36 weeks And Fetal lung immaturity >35to 36 weeks Lung maturity present Intrauterine Transfusion Delivery
- 37. Cordocentesis • Gold standard for detection of fetal anemia • Complications • 2.7% total risk of fetal loss • Reserved for patients with increased MCA-PSV or delta OD450
- 39. Exchange Transfusion •. Considered if the total serum bilirubin level is approaching 20 mg/dL and continues to rise despite intense in-hospital phototherapy. Mortality rate 1%
- 40. Diagnosis and Management contd.
- 41. Review of Management for Rh Isoimmunization • Monthly indirect coombs titer (in first sensitized pregnancy) • If critical titer reached, determine paternal and fetal antigen status • Amniocentesis and delta OD450 OR MCA-PSV ** For 2nd or greater sensitized pregnancy, initiate amnio or MCA at 18-20 weeks**