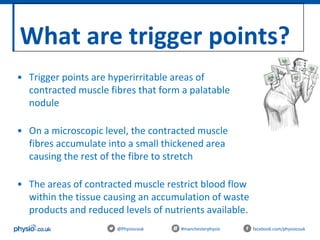
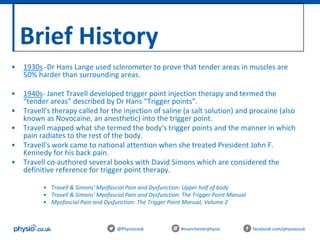
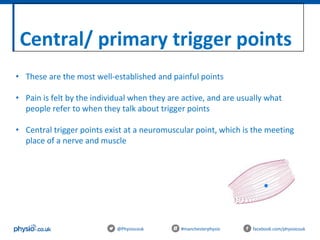
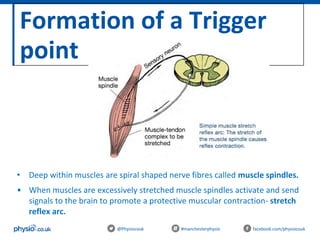
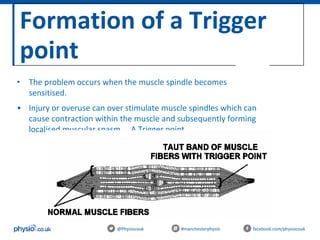
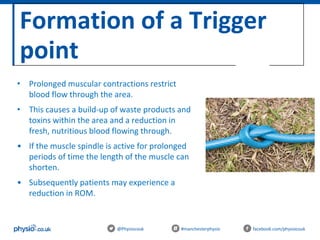
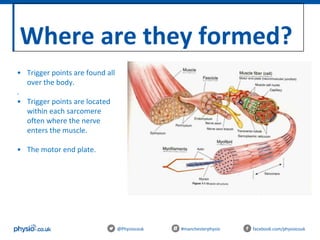
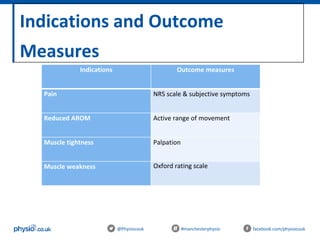
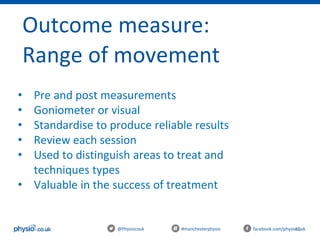
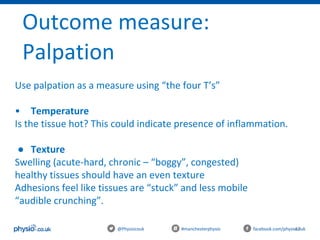
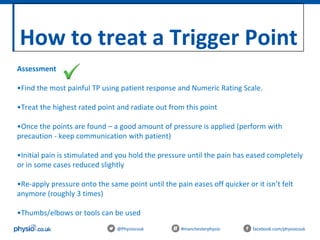
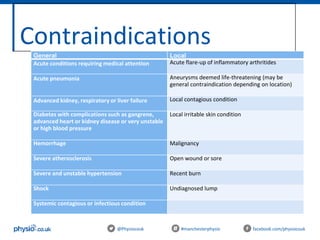
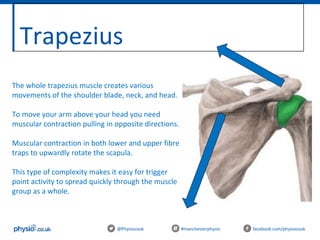
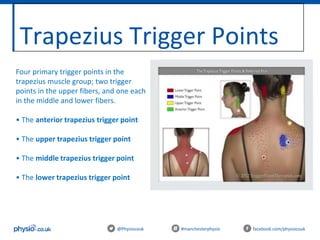
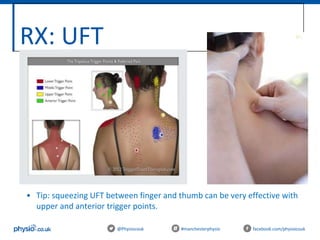
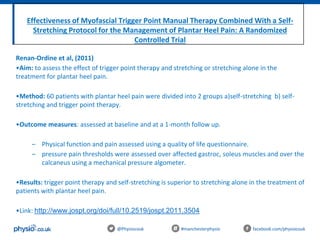
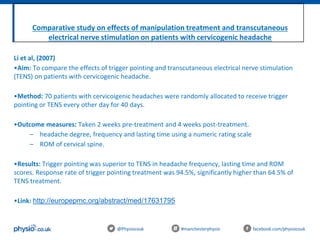
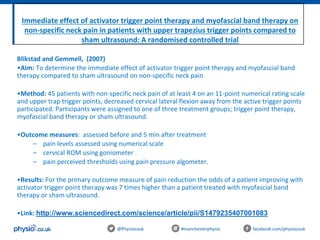
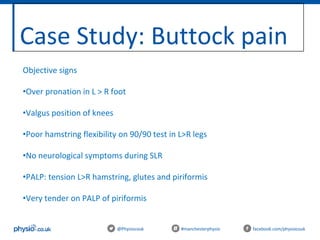
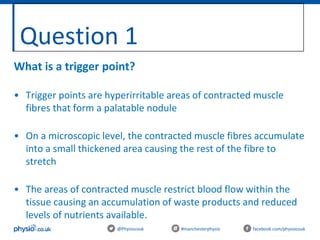
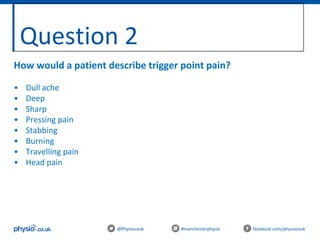
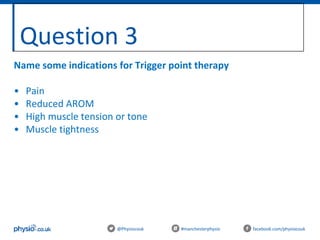
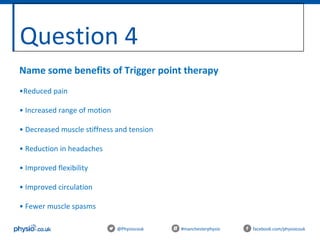
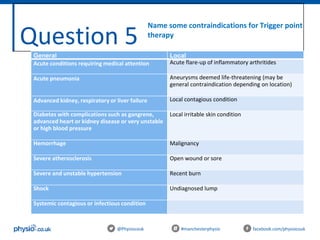
The document provides an overview of trigger point therapy, including its theory, techniques, and practical applications for sports and massage therapists. It details the different types of trigger points, their symptoms, and the history of trigger point therapy, as well as outcome measures for assessing treatment effectiveness. The document outlines the aims, itinerary, and various precautions and contraindications associated with the therapy.