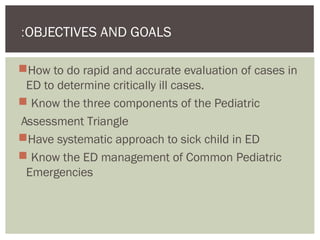
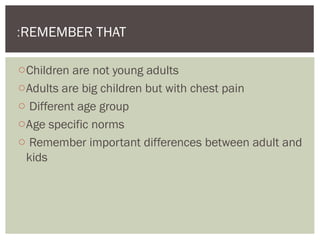
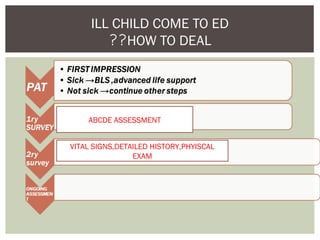
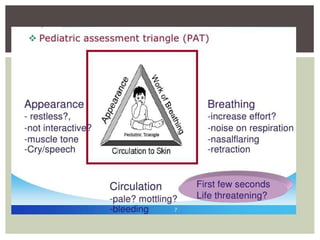
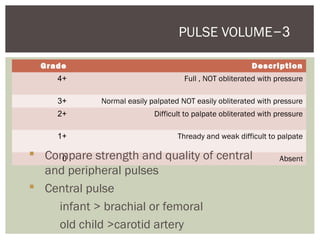
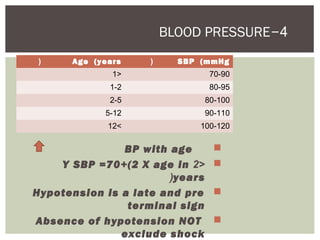
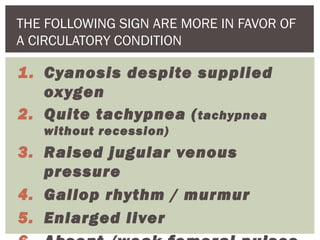
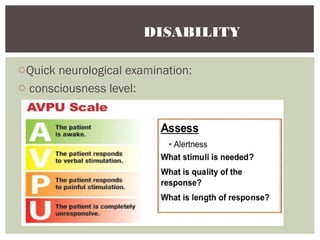
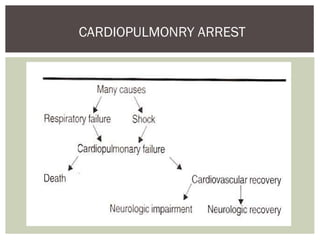
This document provides guidance on assessing and managing critically ill children presenting to the emergency department. It outlines the Pediatric Assessment Triangle (PAT) as a rapid and effective initial evaluation tool focusing on appearance, work of breathing, and circulation. The PAT evaluates tone, interaction, consolability, gaze and cry to assess appearance while circulation is determined by heart rate, capillary refill time, pulses, skin color and temperature. It emphasizes treating the child rather than the diagnosis and remembering key physiological differences between adults and children.