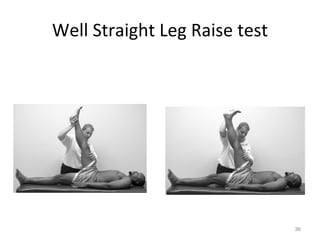
The document provides an overview of evaluating the thoracic and lumbar spine for lower extremity injuries. It discusses obtaining a history including location of pain, onset, mechanism of injury, consistency, and aggravating/alleviating factors. Physical examination includes inspection of posture, gait, and skin markings as well as palpation of spinal landmarks. Range of motion, ligamentous, and neurological testing are outlined to assess for nerve root impingement.