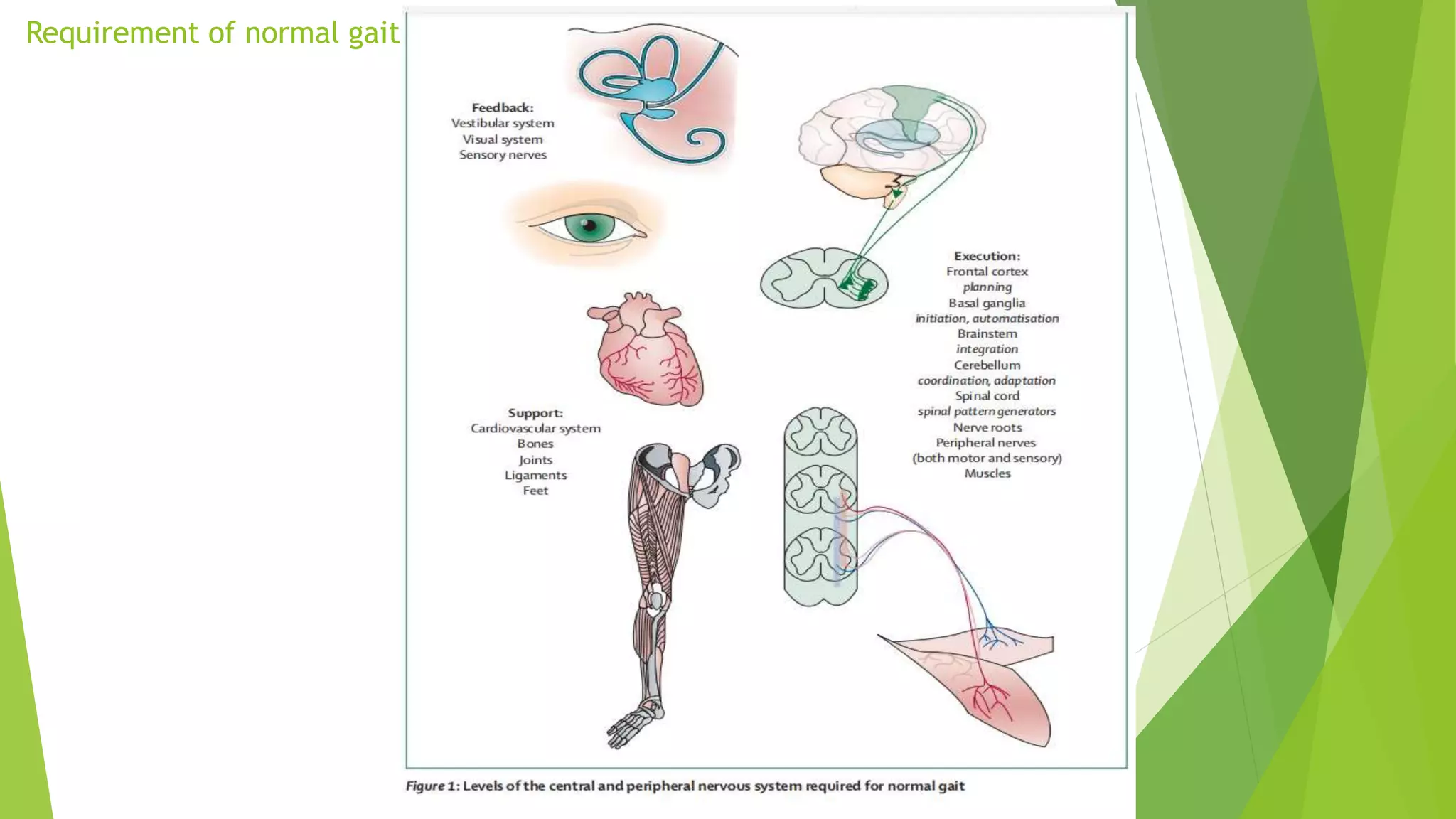
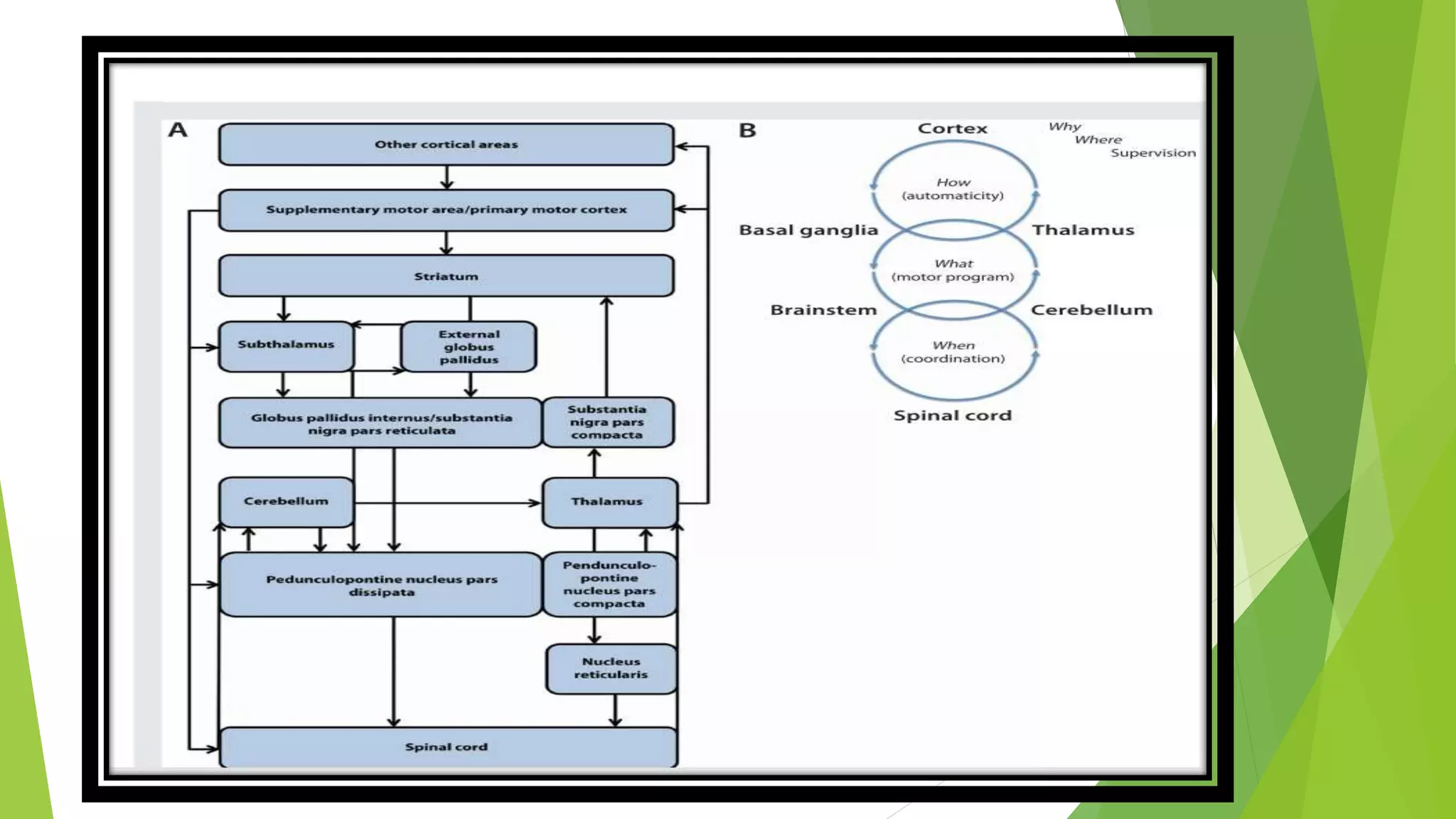
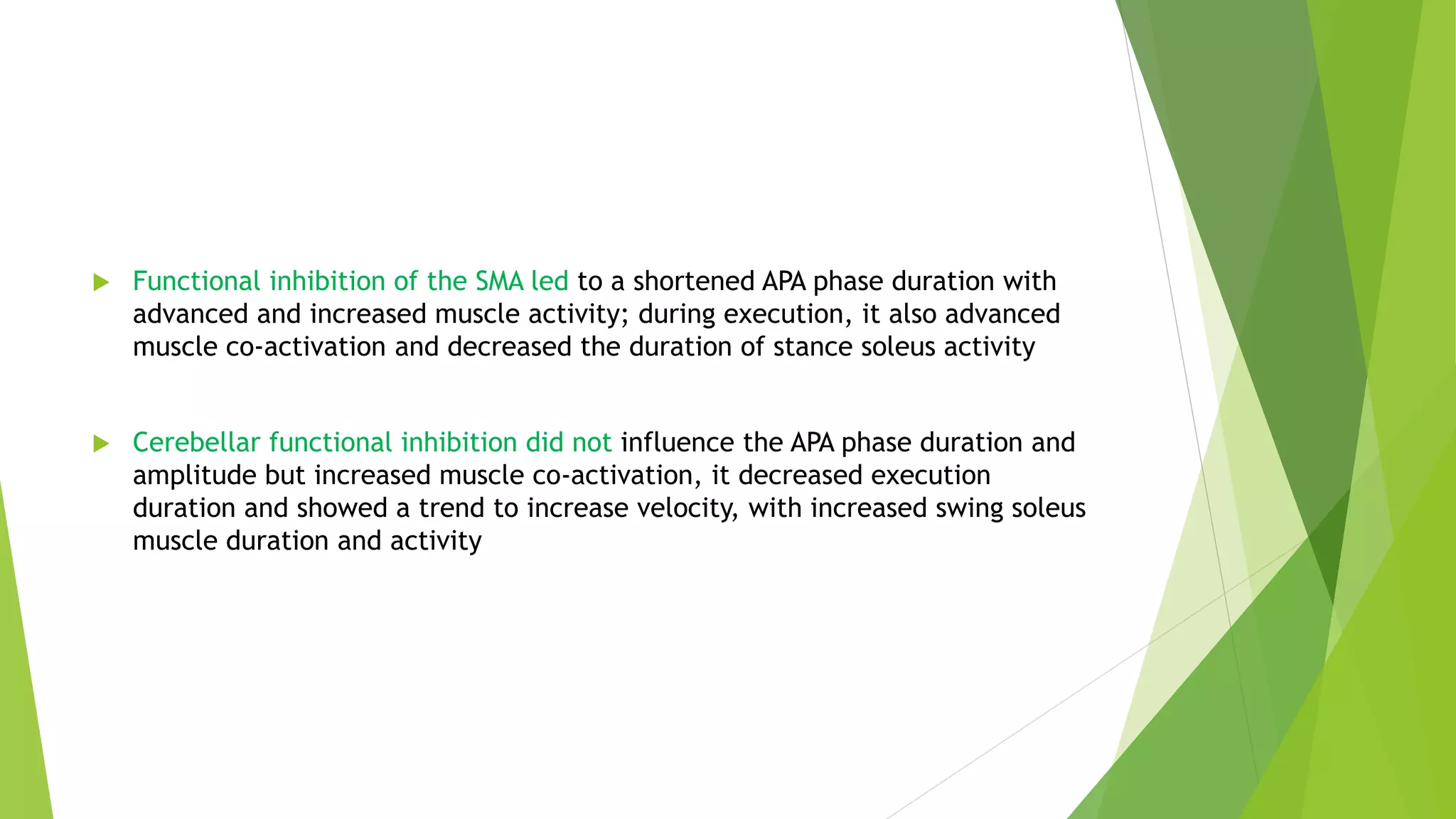
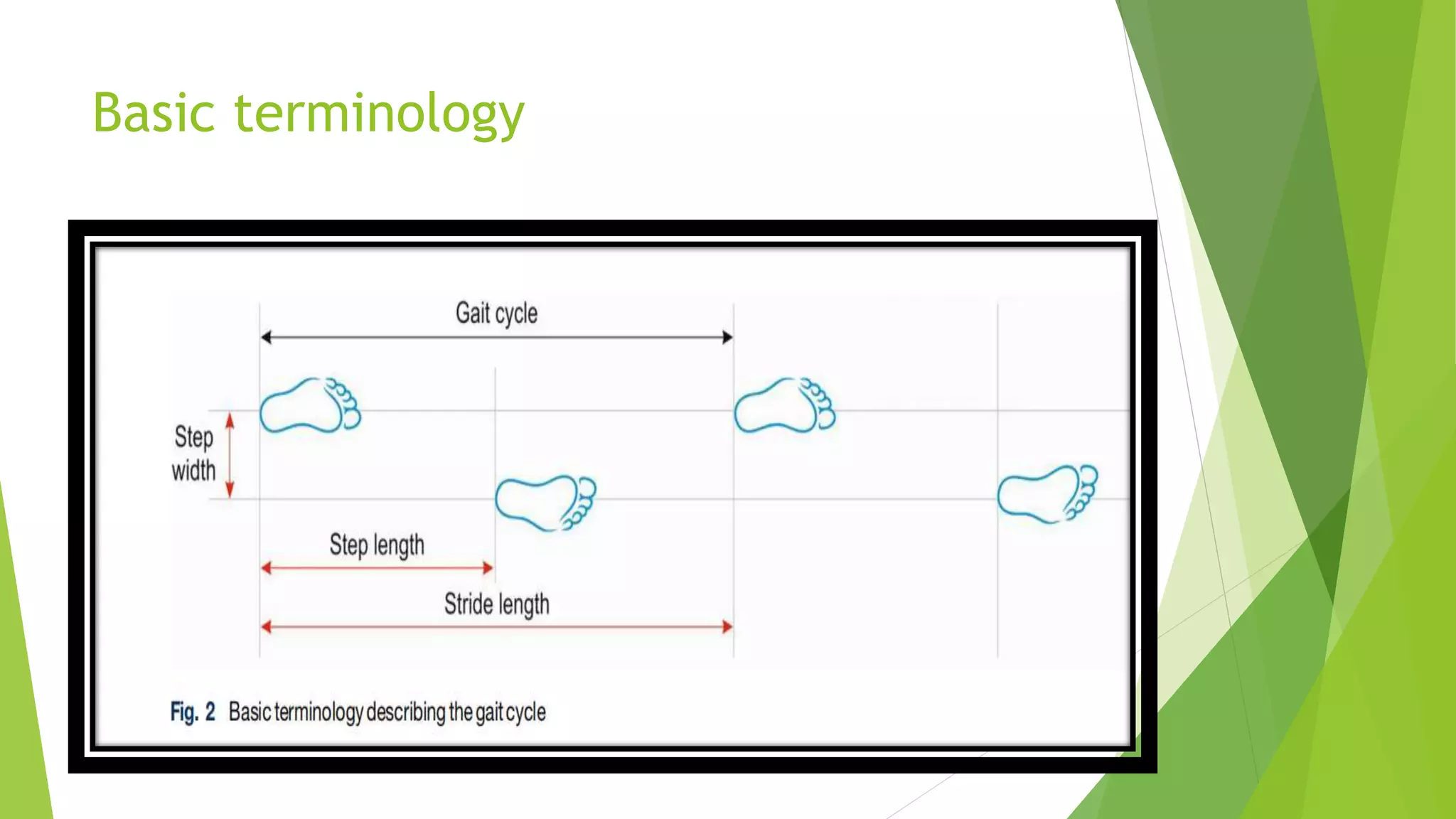
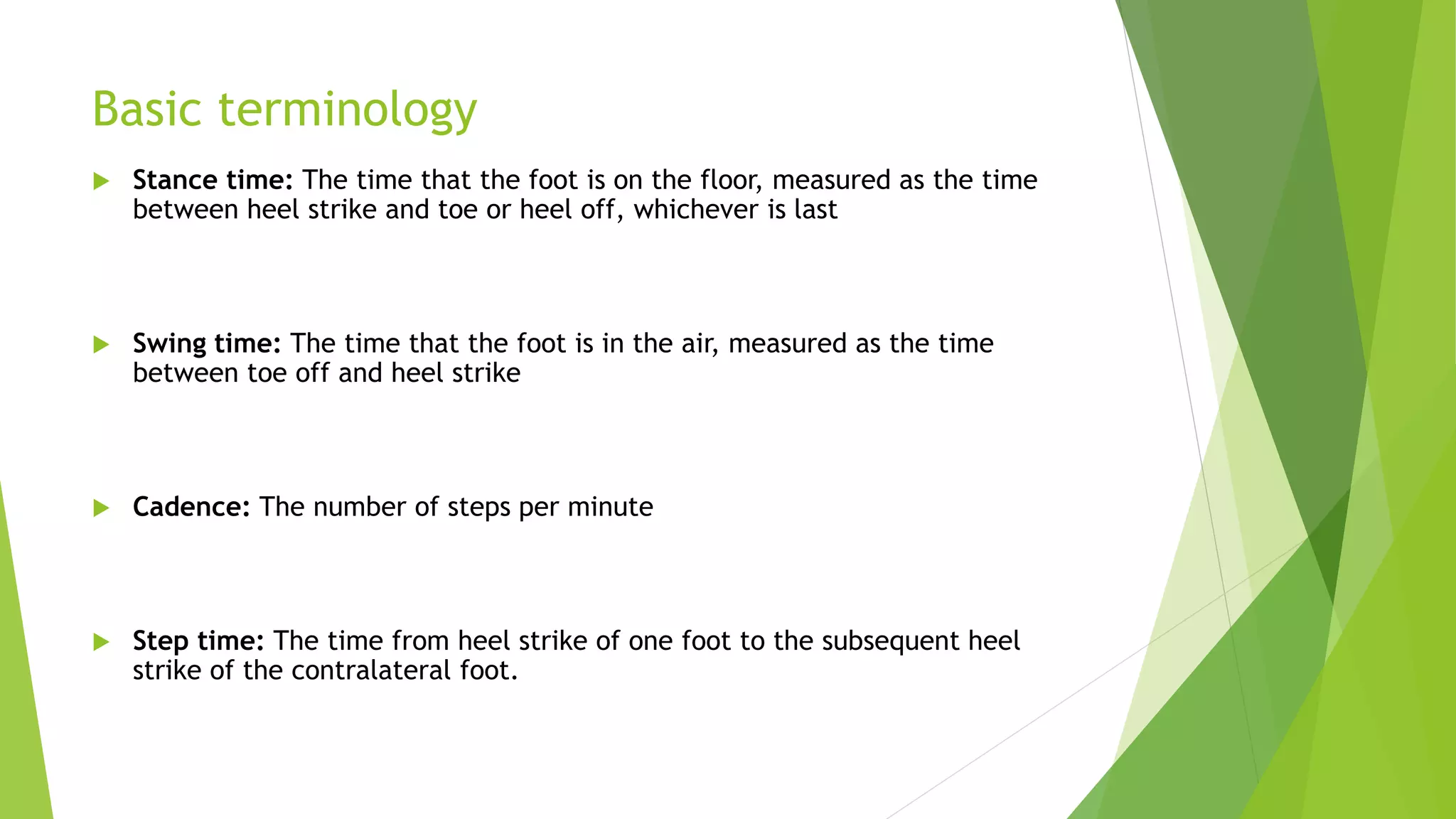
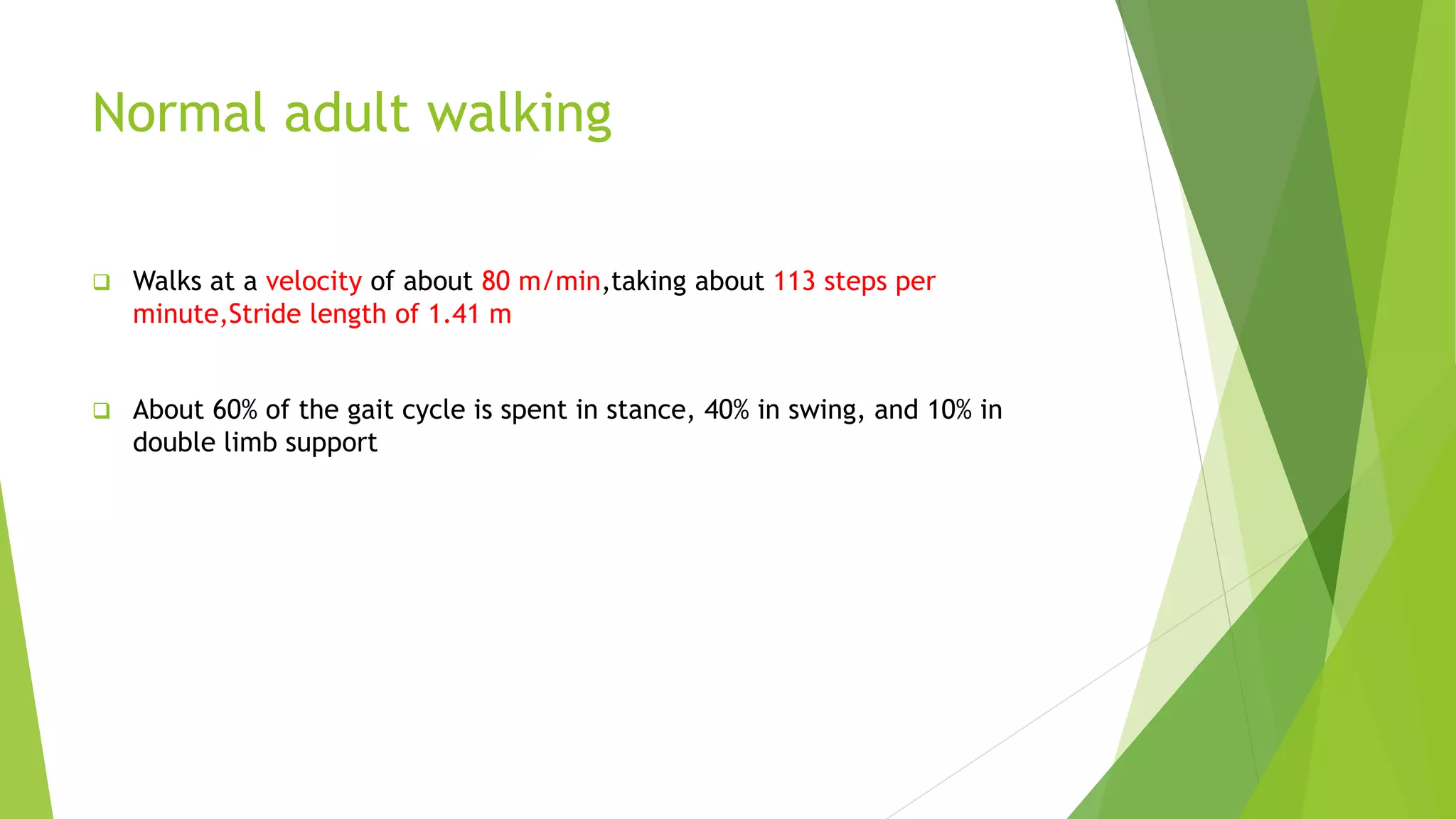
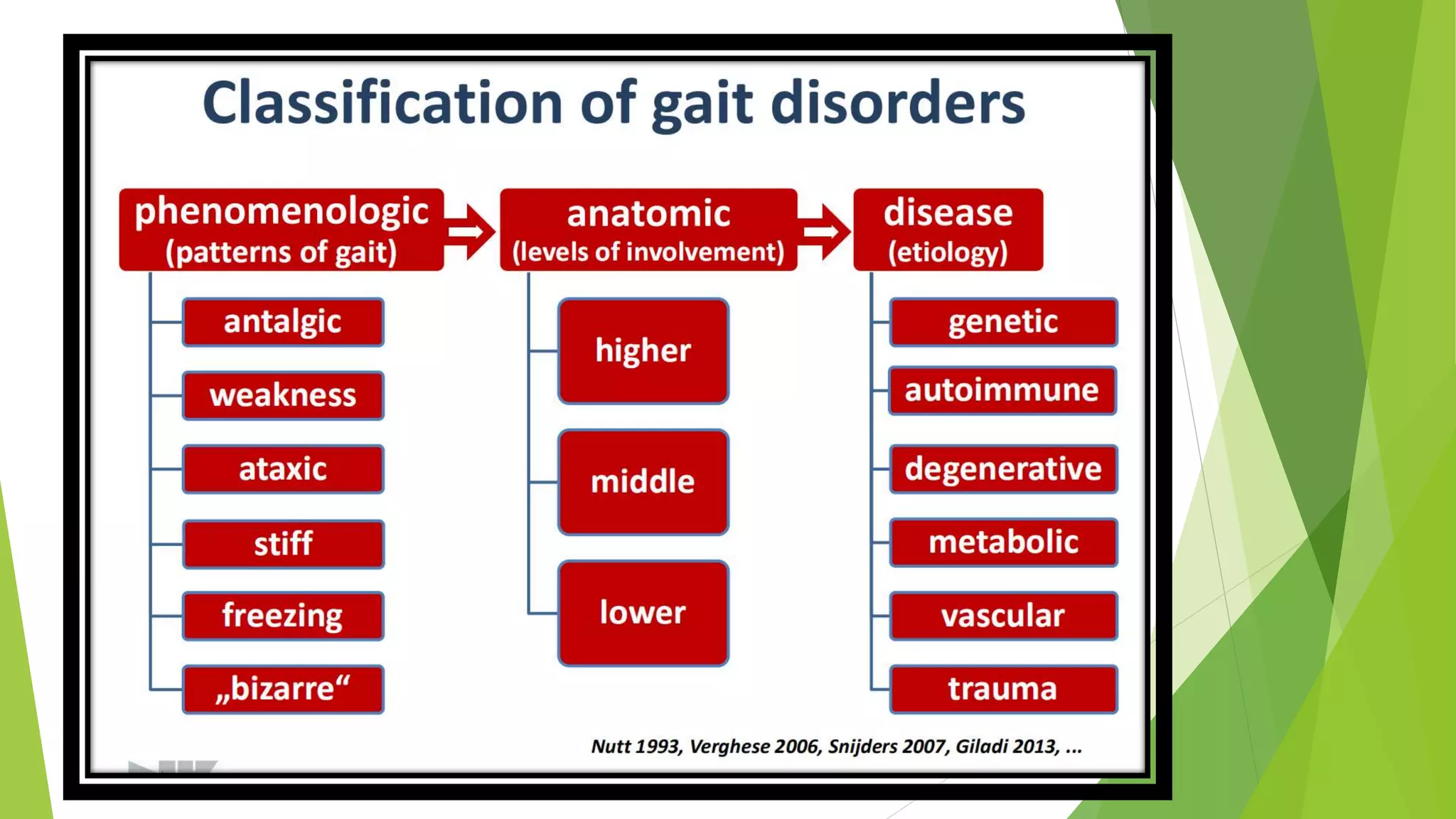
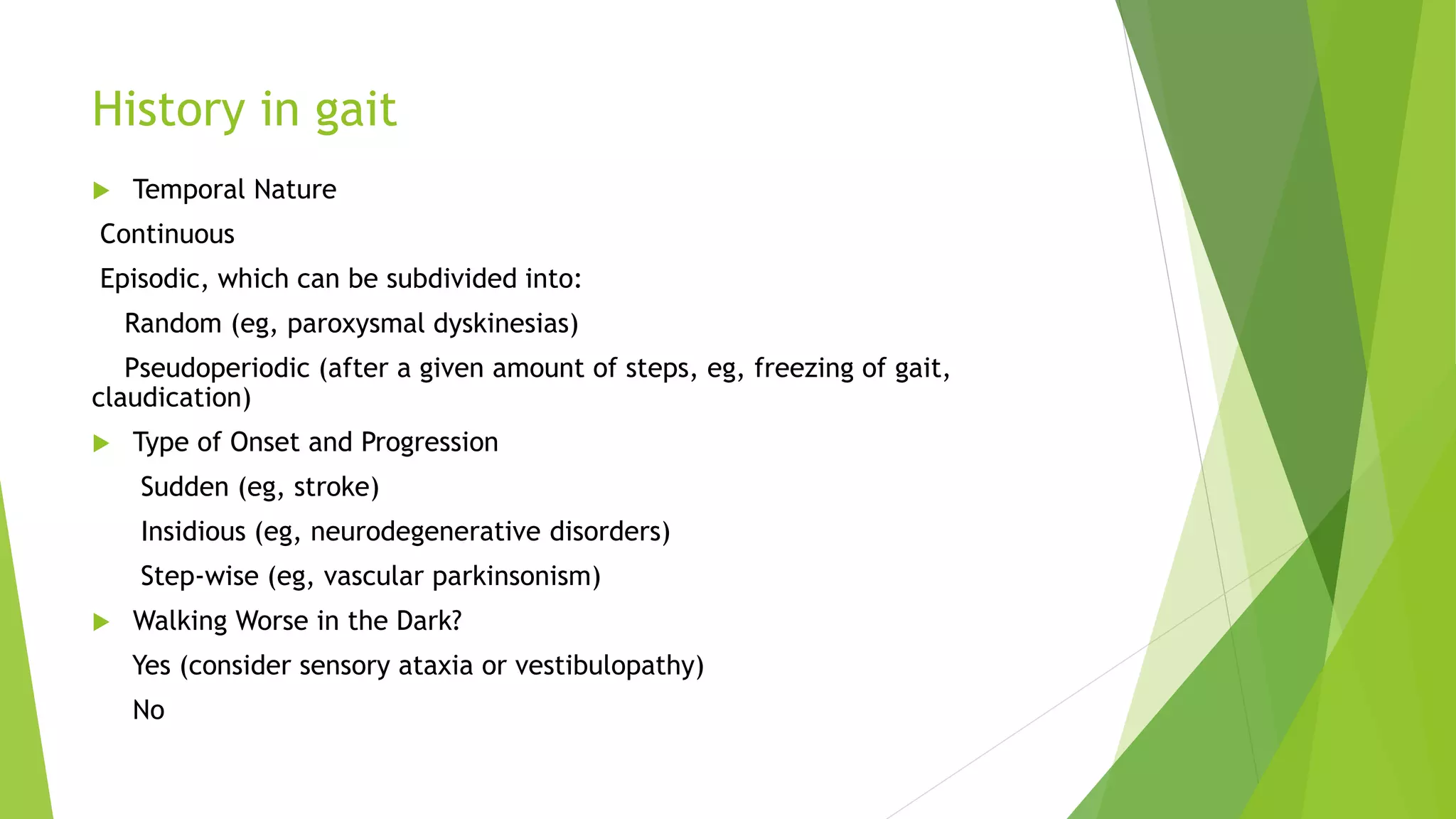
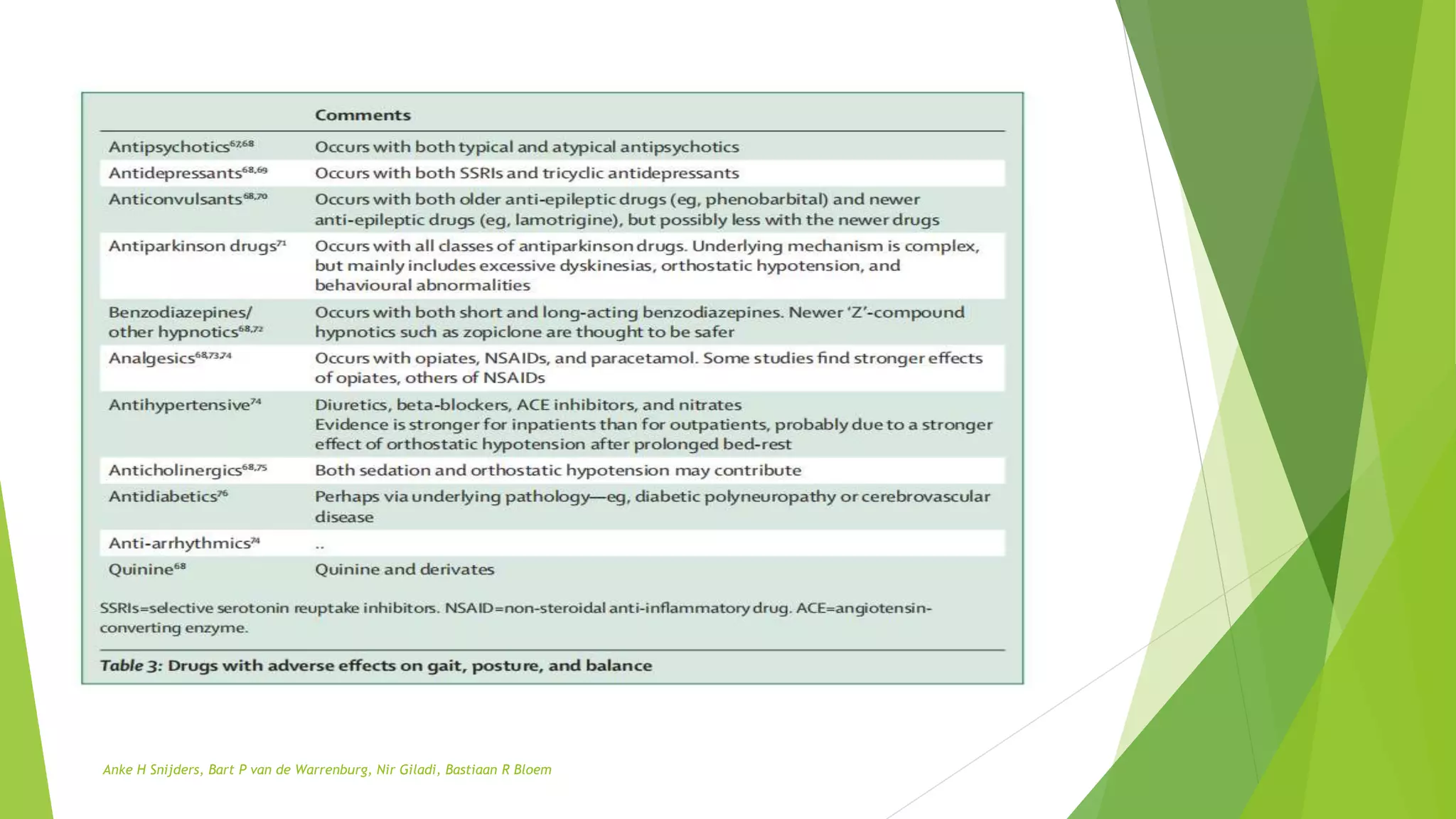
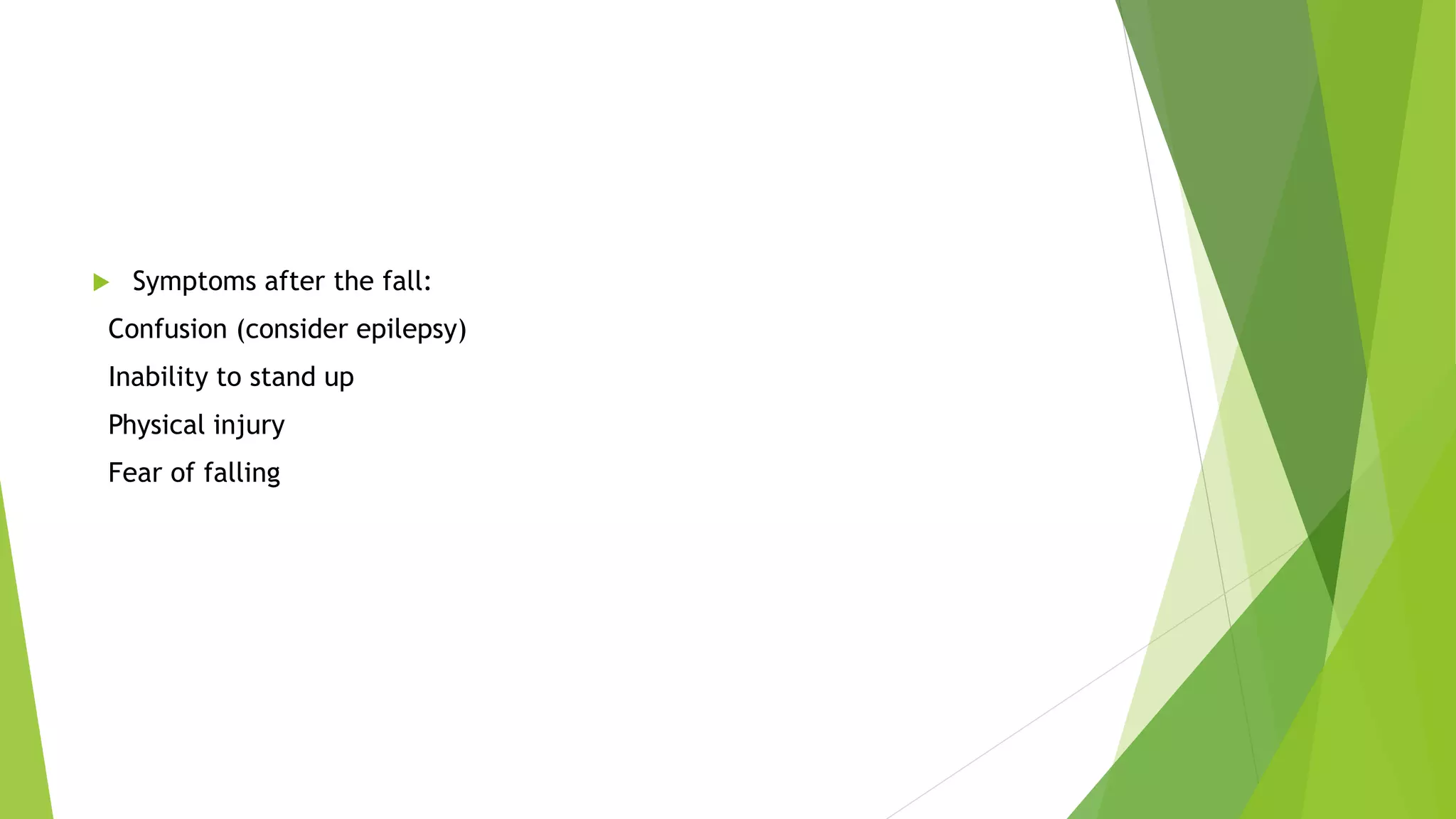
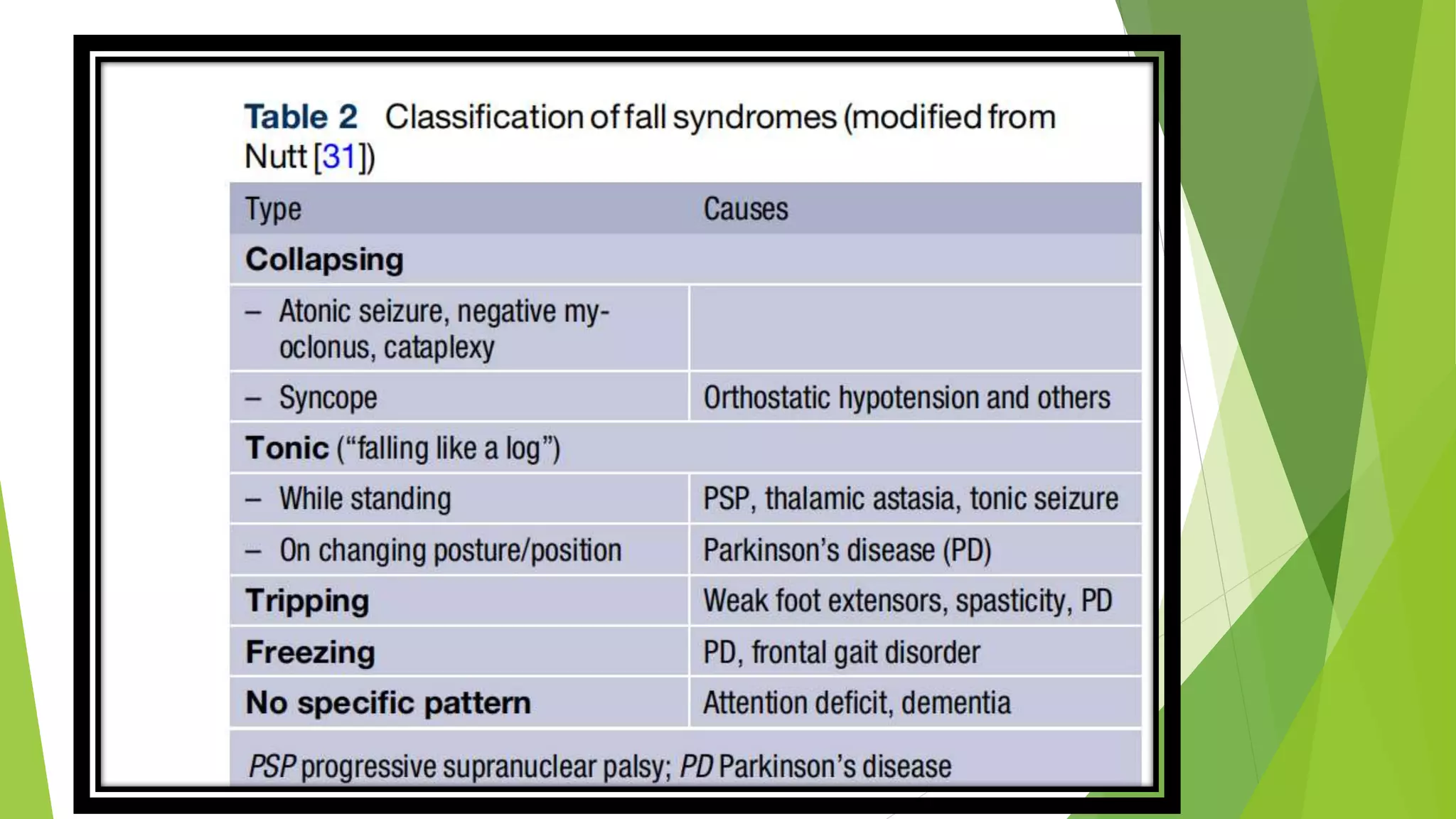
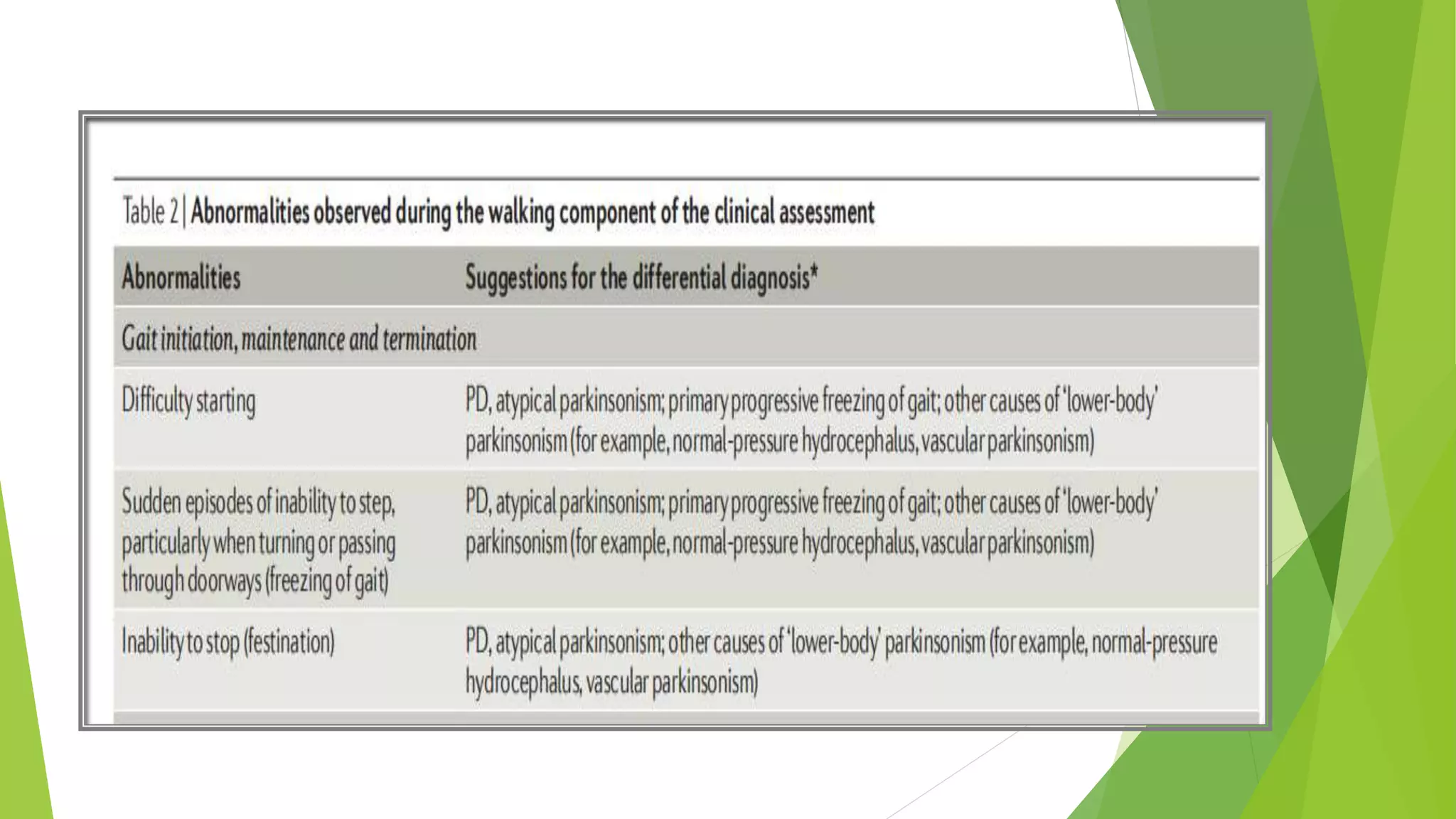
This document discusses normal and abnormal human gait. It begins with definitions of gait, stance, and balance. It then covers the three components and three systems required for normal gait. The document discusses the physiology and neural control of gait, including central pattern generators and higher brain centers. It provides a classification system for gait disorders and describes approaches to clinical assessment. Specific gait abnormalities are defined, including those related to upper and lower motor neuron dysfunction. Treatment approaches for gait disorders are also mentioned.