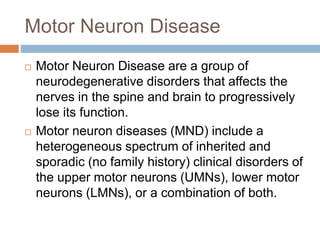
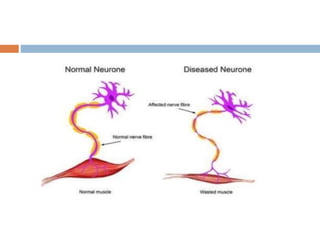
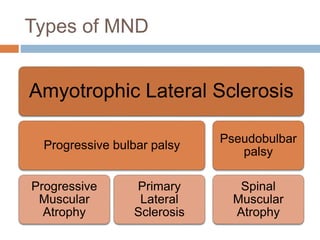
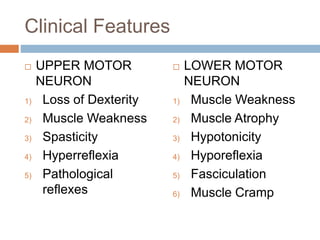
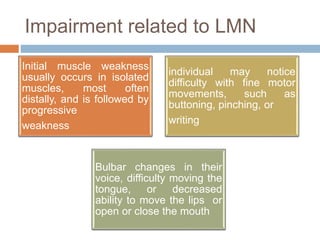
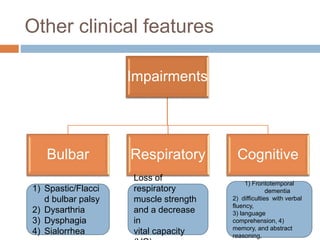
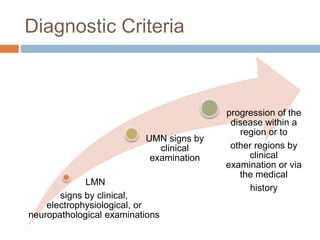
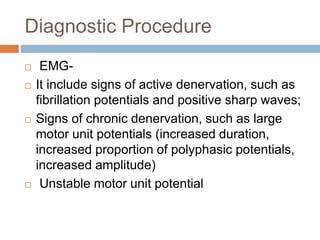
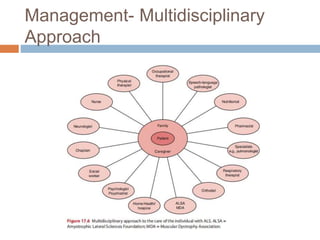
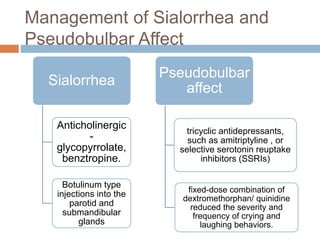
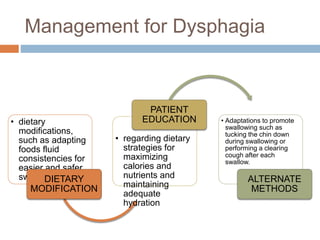
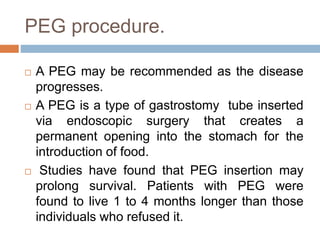
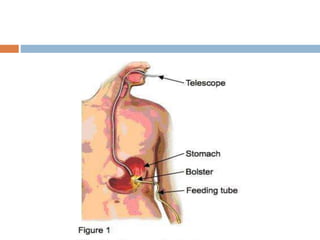
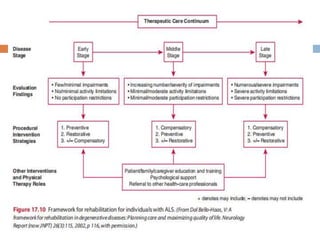
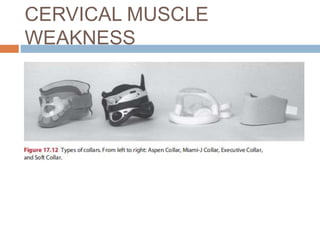
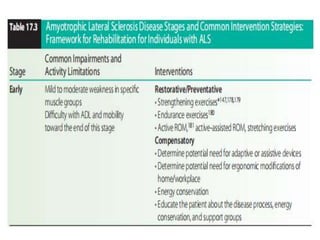
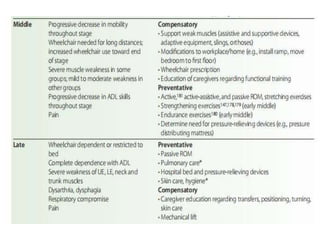
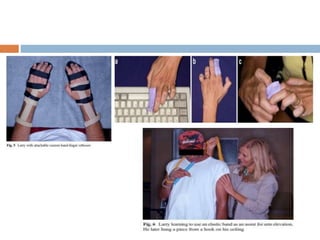
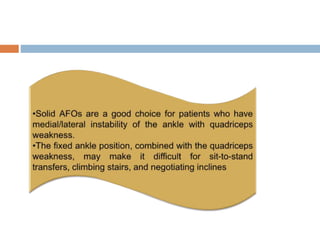
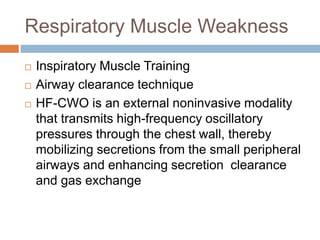
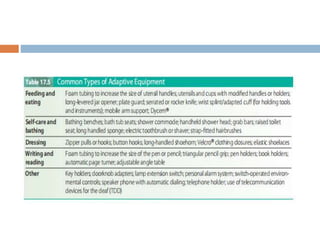
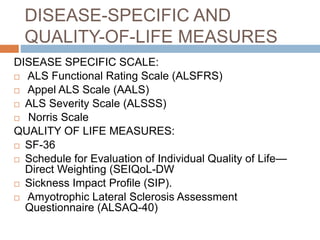
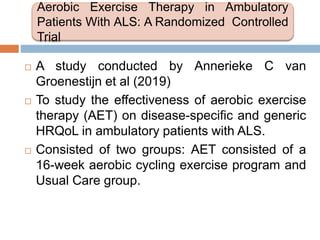
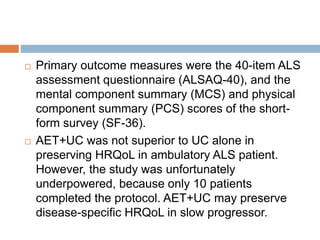
The document discusses motor neuron diseases (MND), including types such as amyotrophic lateral sclerosis (ALS), their clinical features, diagnostic procedures, and management strategies, emphasizing a multidisciplinary approach including physiotherapy. Key management goals involve pain reduction, joint mobility maintenance, and interventions for dysphagia and respiratory issues. It highlights ongoing research regarding aerobic exercise therapy's effectiveness on quality of life in patients with ALS.