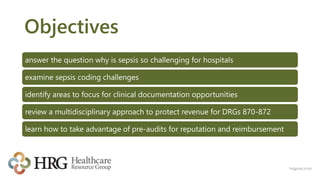
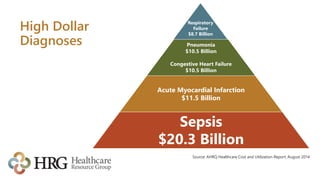
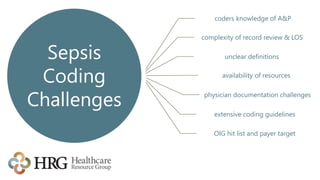
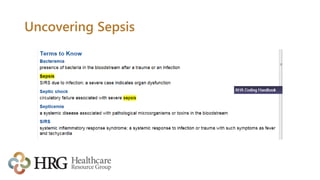
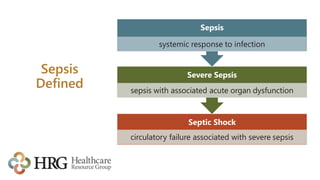
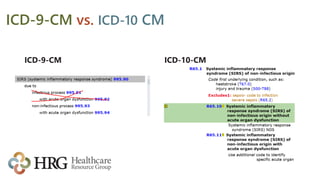
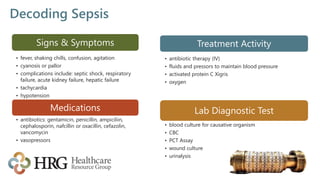
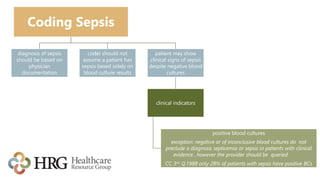
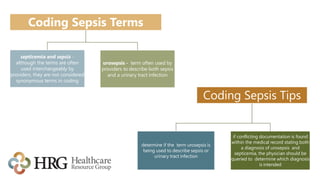
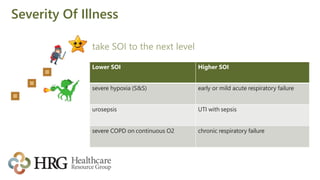
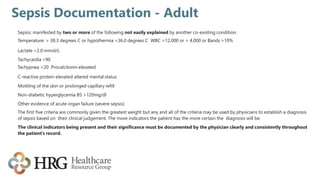
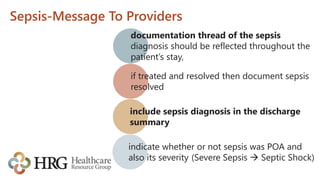
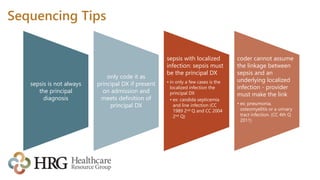
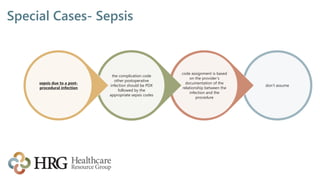
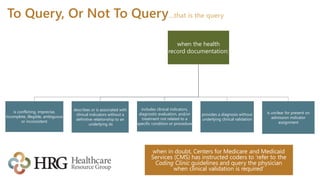
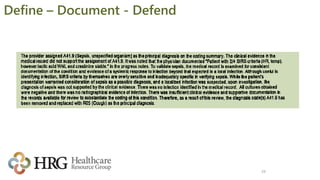
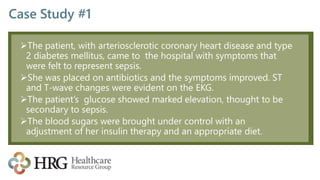
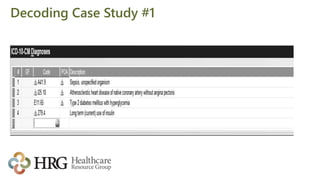
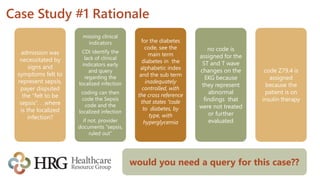
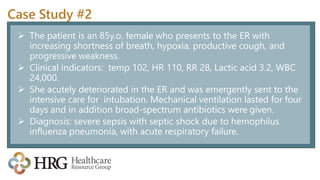
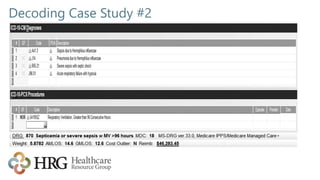
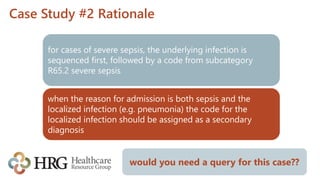
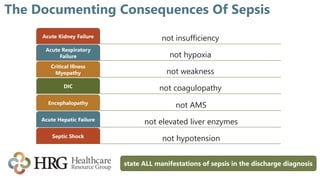
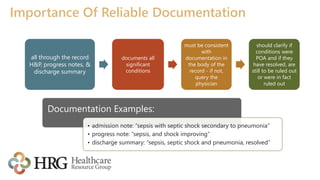
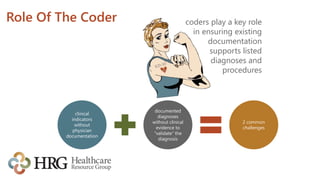
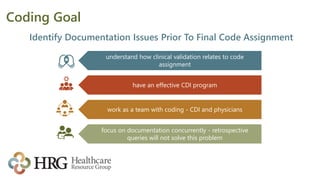
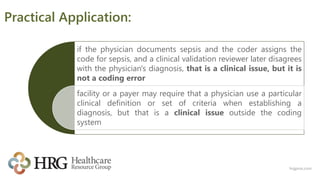
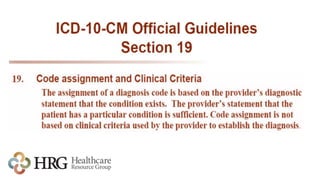
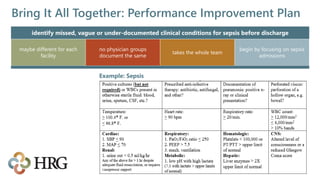
The presentation by Laura Legg focuses on the complexities of coding sepsis in hospitals, highlighting the significant costs associated with sepsis care, estimated at $20.3 billion annually in the U.S. It outlines specific challenges in sepsis documentation and coding, emphasizing the need for clear clinical indicators, physician queries, and effective documentation practices. The presentation advocates for multidisciplinary approaches to improve coding accuracy and protect hospital revenue related to Diagnosis Related Groups (DRGs) 870-872.