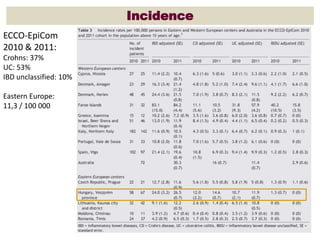
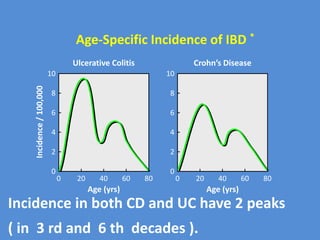
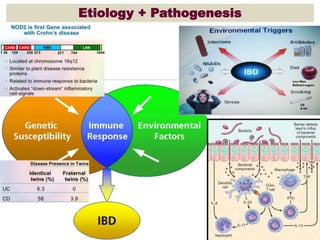
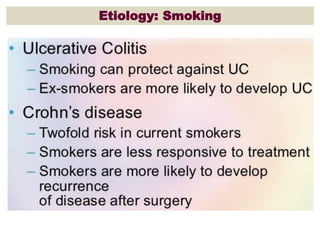
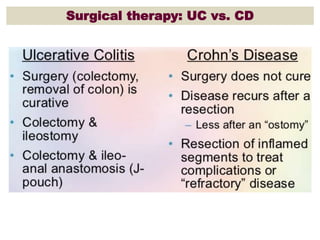
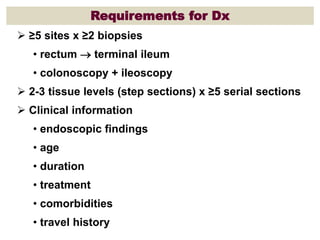
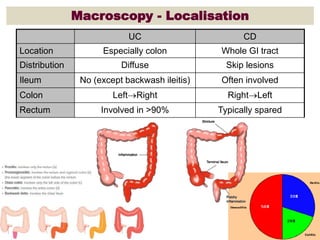
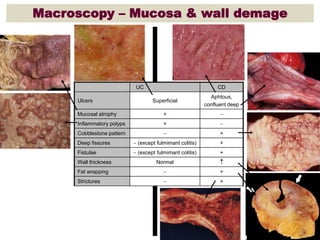
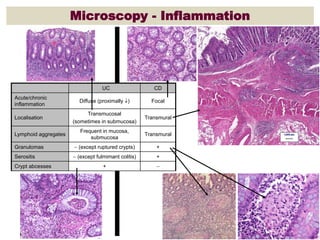
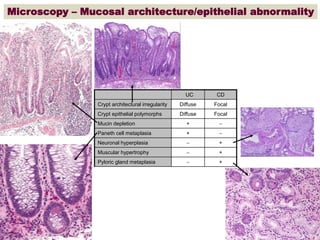
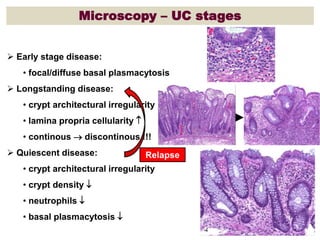
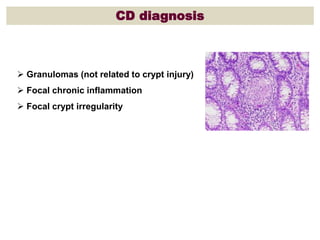
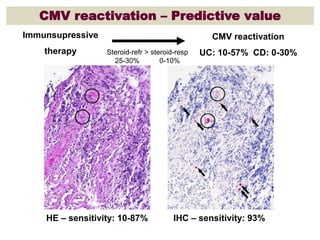
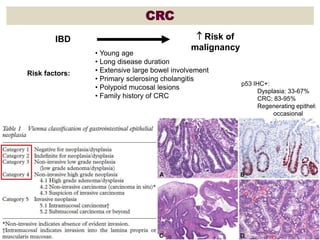
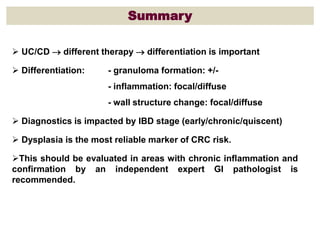
The document provides a comprehensive overview of inflammatory bowel disease (IBD) histopathology, detailing incidence rates, diagnostic requirements, and key histological findings for both Crohn's disease (CD) and ulcerative colitis (UC). It emphasizes the differences in therapy for UC and CD, the importance of differentiation in diagnosis, and identifies dysplasia as a critical marker for colorectal cancer risk associated with IBD. The document also discusses the influence of disease stage on diagnostics and highlights specific microscopic features relevant to each type of IBD.