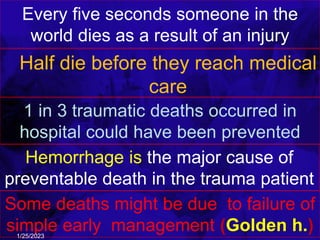
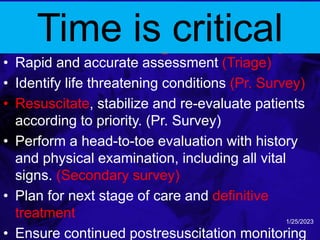
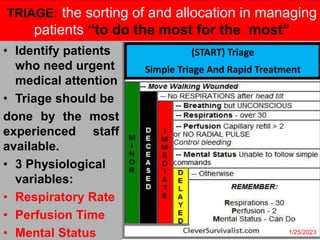
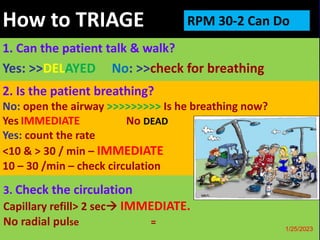
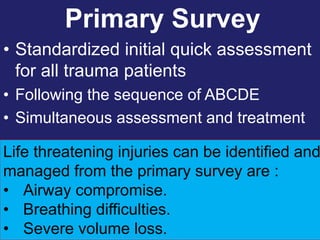
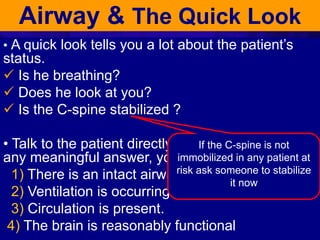
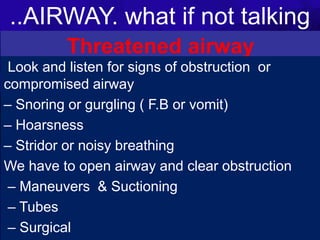
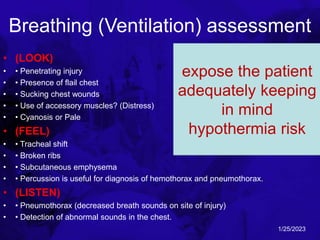
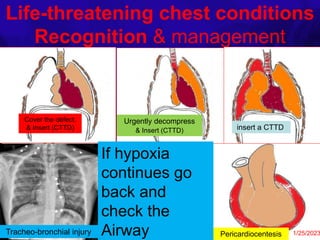
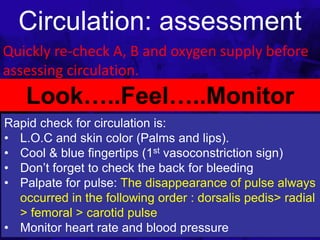
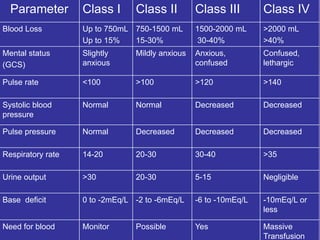
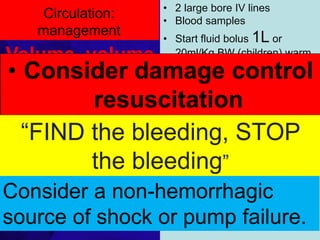
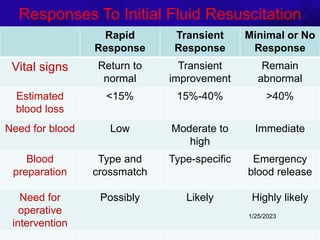
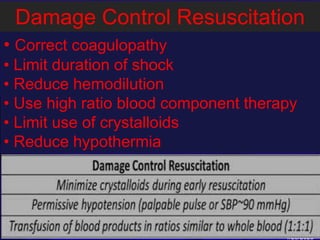
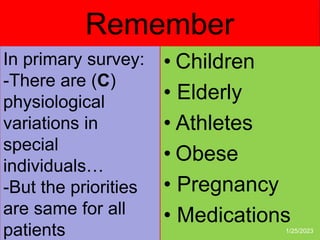
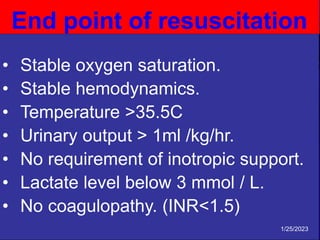
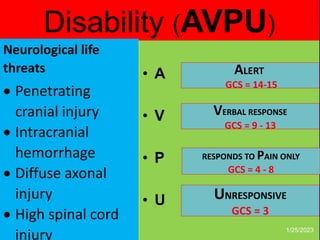
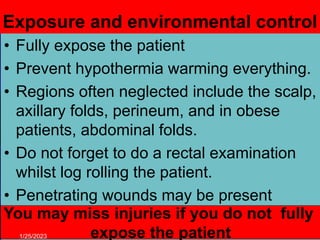
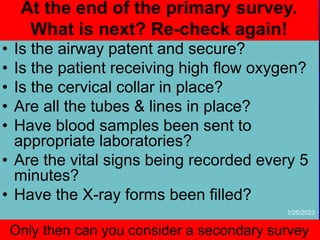
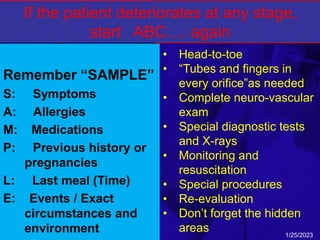
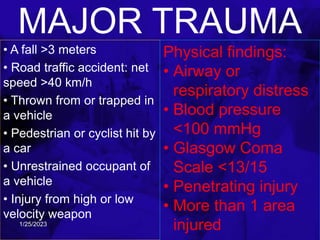
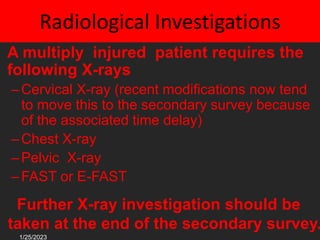
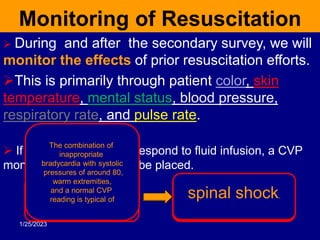
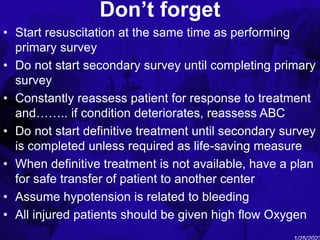
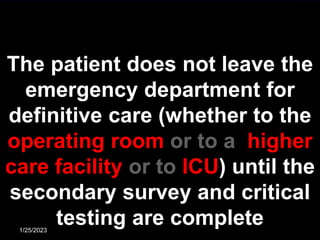
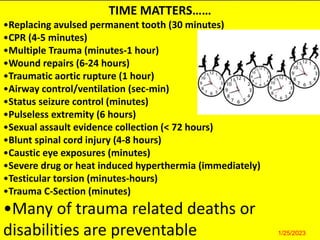
The document outlines the critical elements of trauma assessment and management, emphasizing the importance of rapid and accurate initial evaluations to prevent preventable deaths due to trauma. Key principles include prioritizing life-threatening conditions, effective resuscitation, and thorough patient assessment through a systematic primary and secondary survey approach. The urgency of immediate intervention and coordinated team efforts are necessary to improve patient outcomes and reduce mortality in traumatic situations.