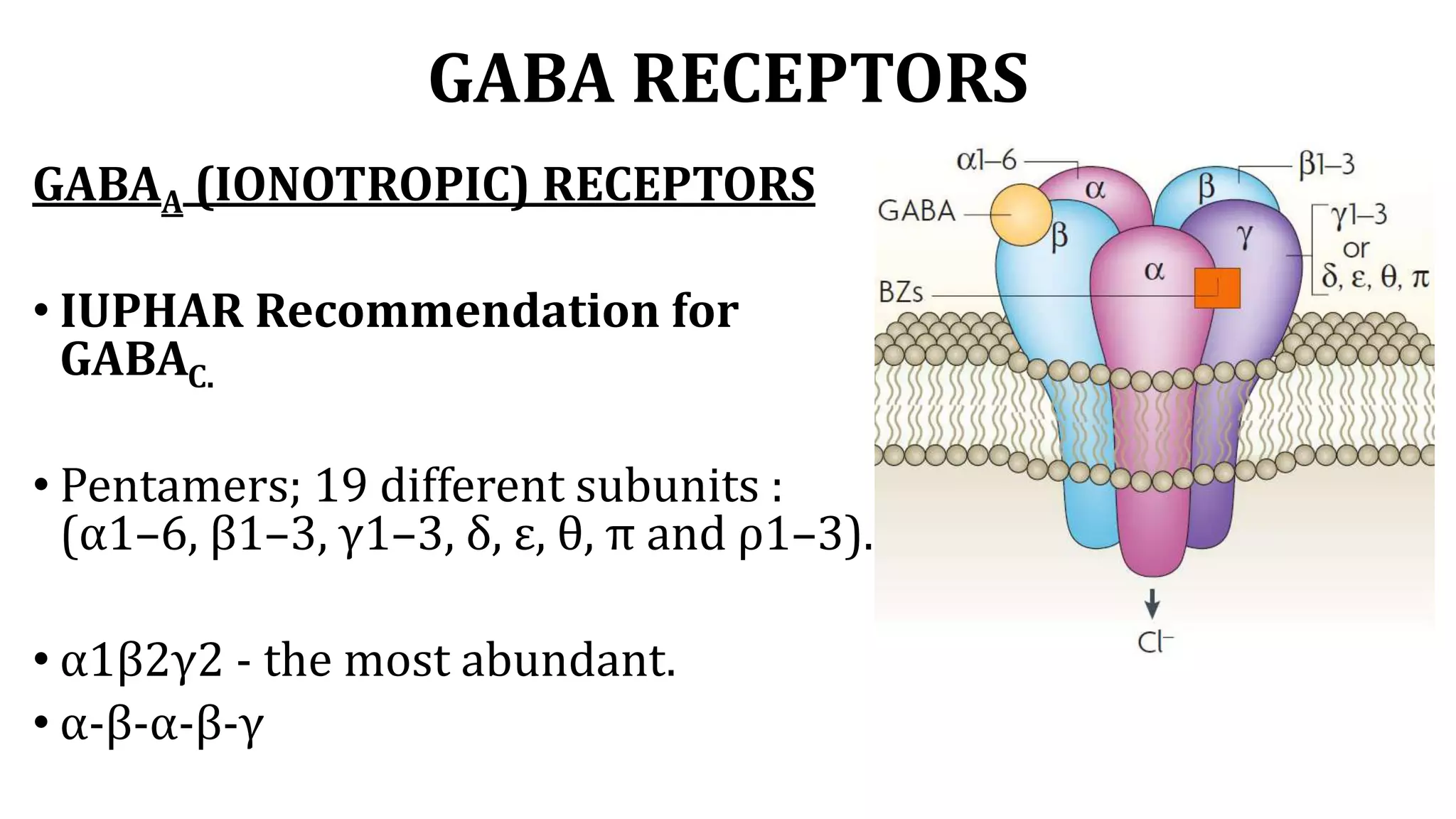
This document provides an overview of glutamate and GABA, their receptors and therapeutic applications. It discusses the synthesis, storage, release and termination of glutamate and GABA in the central nervous system. It describes the ionotropic and metabotropic glutamate receptors and GABAA and GABAB receptors. It also discusses conditions associated with glutamate like seizures, neurodegenerative diseases and stroke. Finally, it outlines current and upcoming therapeutic agents that target glutamate and GABA receptors and their uses, mechanisms and adverse effects.