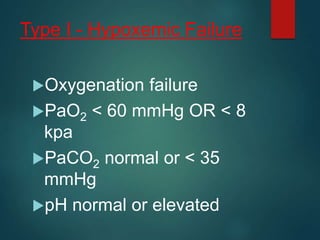
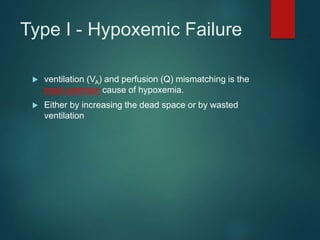
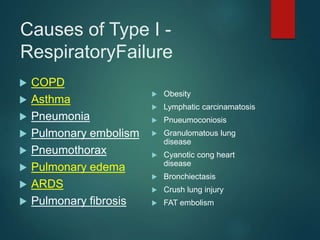
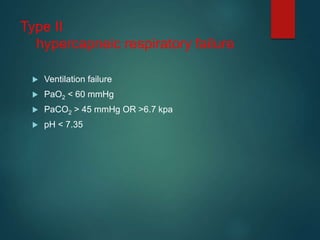
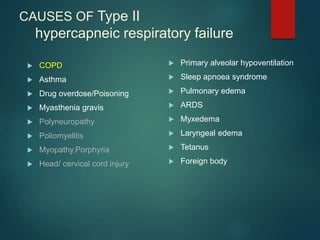
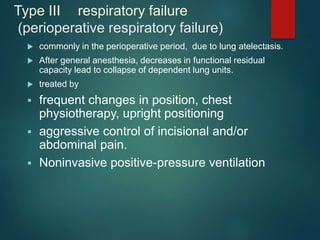
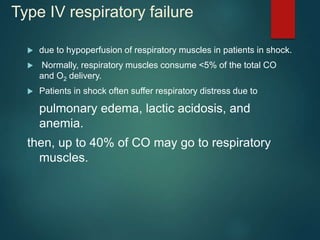
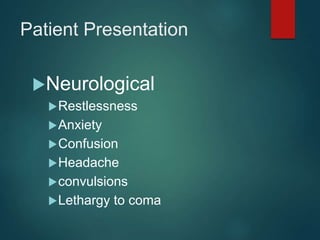
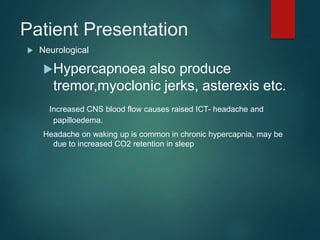
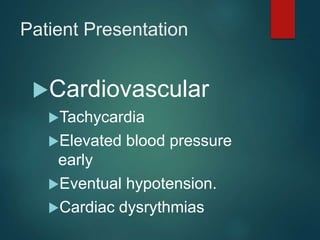
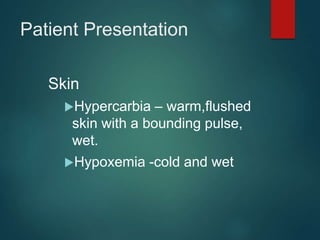
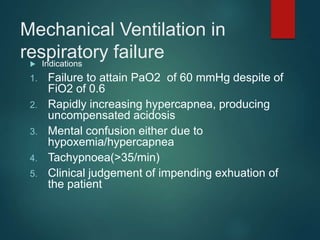
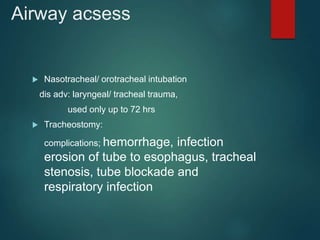
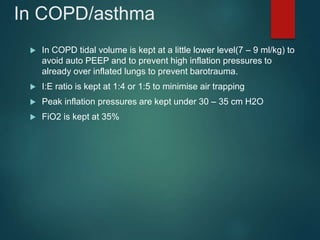
This document provides an overview of respiratory failure, including its definition, types, causes, patient presentation, investigations, management, and complications. There are four types of respiratory failure: type I involves hypoxemic failure due to issues with oxygenation; type II involves hypercapneic failure due to ventilation issues; type III occurs perioperatively due to lung collapse; and type IV is due to respiratory muscle hypoperfusion in shock. The management of respiratory failure involves treating the underlying cause, providing oxygen support, and potentially mechanical ventilation. Outcomes depend on the severity of acidosis and underlying illnesses.