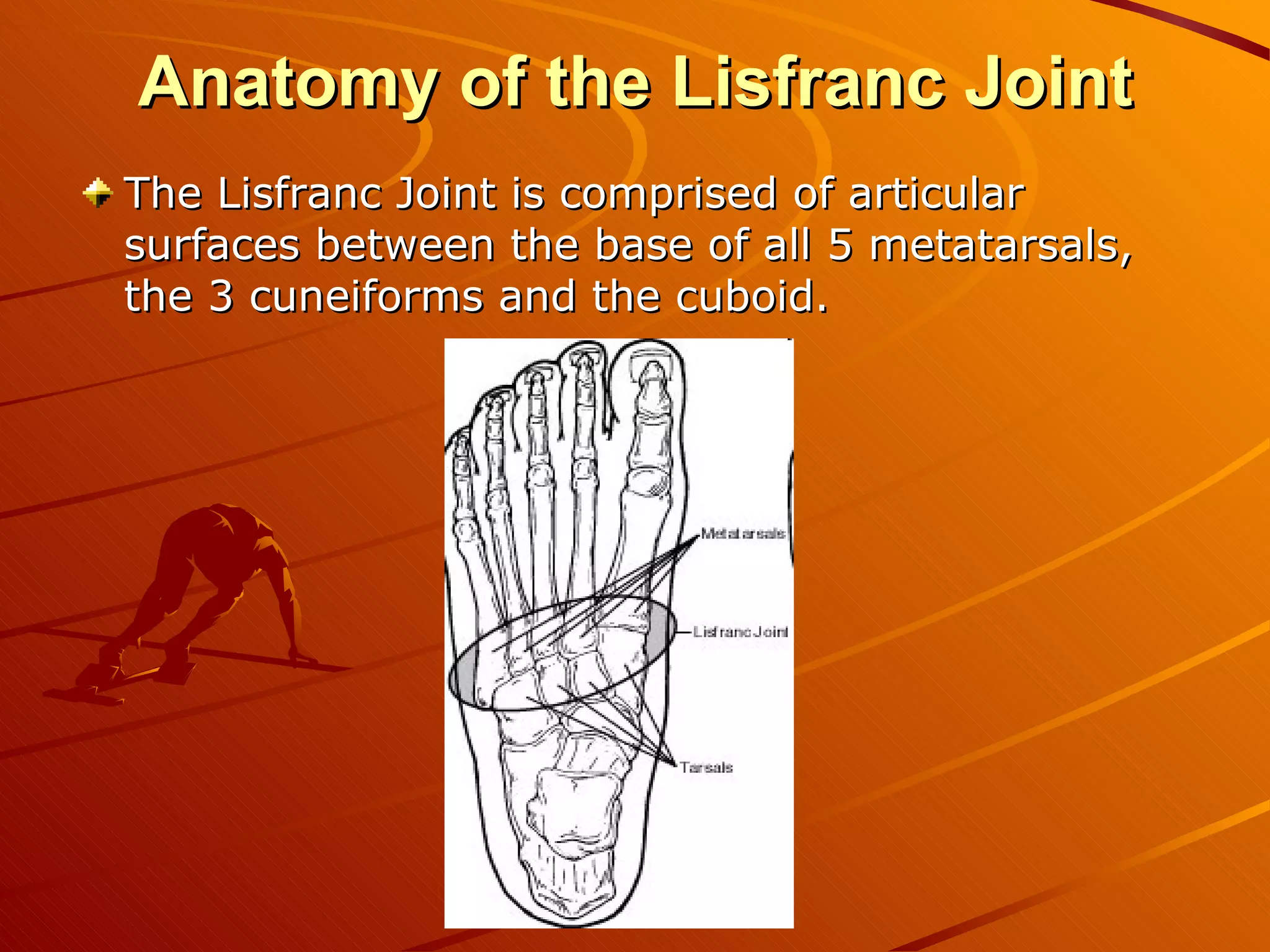
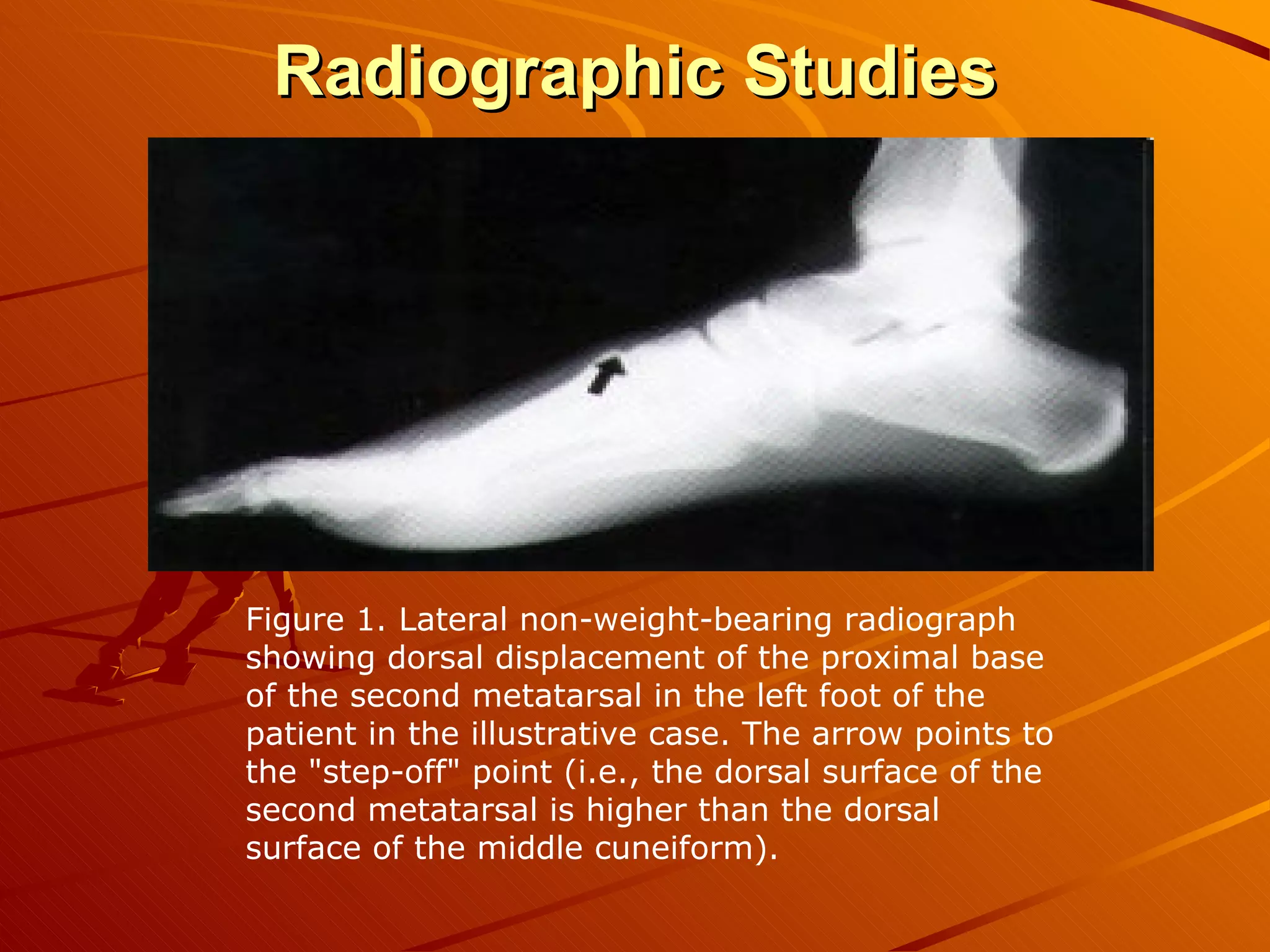
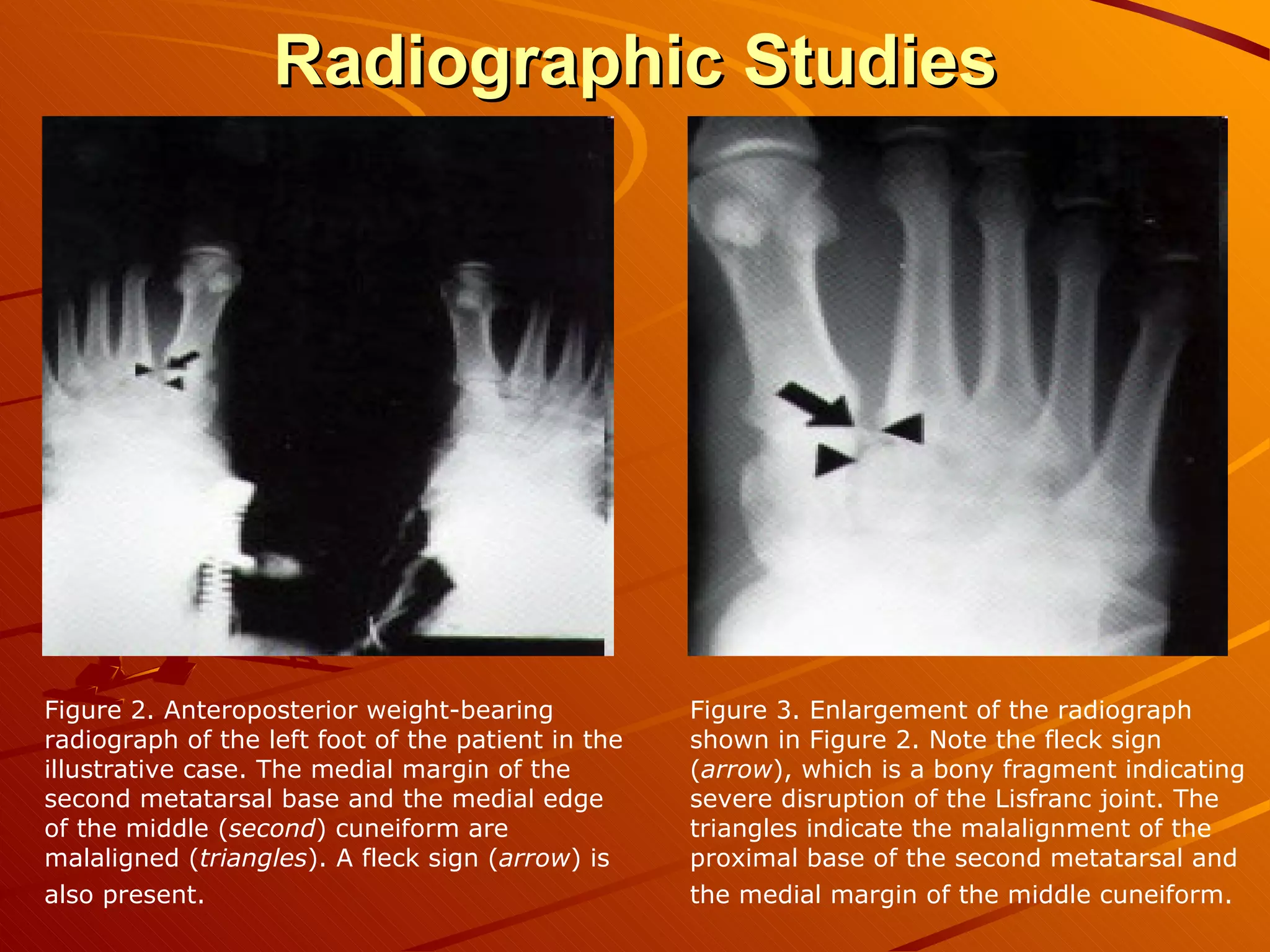
The Lisfranc joint was named after a field surgeon who described an amputation through the joint due to gangrene from an injury sustained after a soldier fell from a horse. Lisfranc injuries account for less than 1% of fractures and can result from high-energy trauma or less stressful twisting injuries. Diagnosis can be difficult as swelling and pain in the midfoot region are often the only findings. Treatment involves immobilization for mild sprains but surgery within 1-2 days for fractures or dislocations to ensure proper healing and prevent long-term disability. Surgical techniques include open reduction and internal fixation to anatomically realign the bones which allows for better functional outcomes compared to fusion or casting.











![References Gaines RJ, Wright G, Stewart J. Injury to the tarsometatarsal joint complex during fixation of Lisfranc fracture dislocations: an anatomic study. J Trauma . Apr 2009;66(4):1125-8. [Medline] . Cook KD, Jeffries LC, O'Connor JP, Svach D. Determining the strongest orientation for "Lisfranc's screw" in transverse plane tarsometatarsal injuries: a cadaveric study. J Foot Ankle Surg . Jul-Aug 2009;48(4):427-31. [Medline] . Kaar S, Femino J, Morag Y. Lisfranc joint displacement following sequential ligament sectioning. J Bone Joint Surg Am . Oct 2007;89(10):2225-32. [Medline] . Hardcastle PH, Reschauer R, Kutscha-Lissberg E, et al. Injuries to the tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg Br . 1982;64(3):349-56. [Medline] . [Full Text] . Desmond EA, Chou LB. Current concepts review: Lisfranc injuries. Foot Ankle Int . Aug 2006;27(8):653-60. [Medline] . Lattermann C, Goldstein JL, Wukich DK, et al. Practical management of Lisfranc injuries in athletes. Clin J Sport Med . Jul 2007;17(4):311-5. [Medline] . Curtis MJ, Myerson M, Szura B. Tarsometatarsal joint injuries in the athlete. Am J Sports Med . Jul-Aug 1993;21(4):497-502. [Medline] . Patillo D, Rudzki JR, Johnson JE, et al. Lisfranc injury in a national hockey league player: a case report. Int J Sports Med . Nov 2007;28(11):980-4. [Medline] . Chilvers M, Donahue M, Nassar L, et al. Foot and ankle injuries in elite female gymnasts. Foot Ankle Int . Feb 2007;28(2):214-8. [Medline] .](https://image.slidesharecdn.com/lisfrancinjury-100921223507-phpapp02/75/Lis-Franc-Injury-18-2048.jpg)
