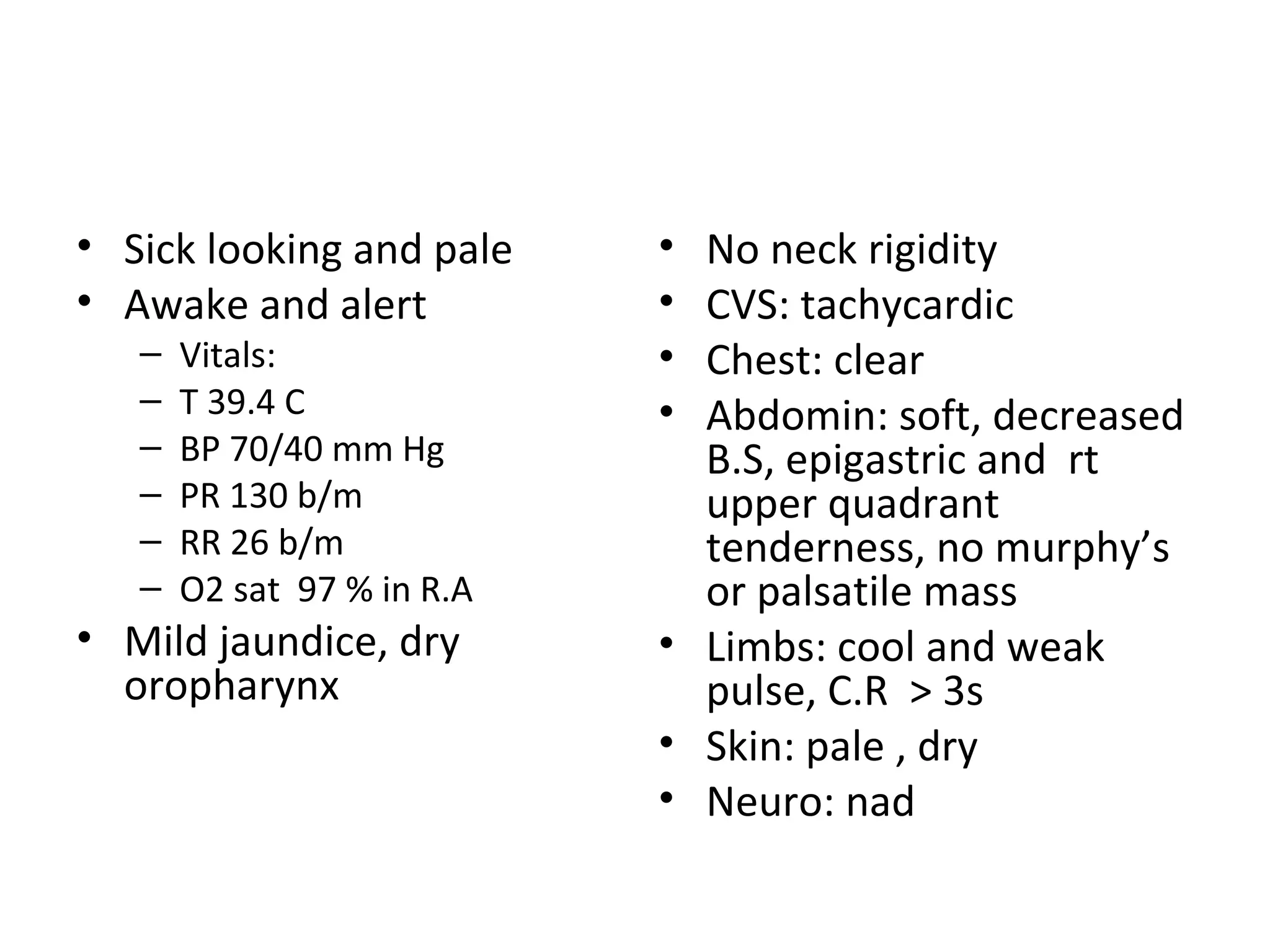
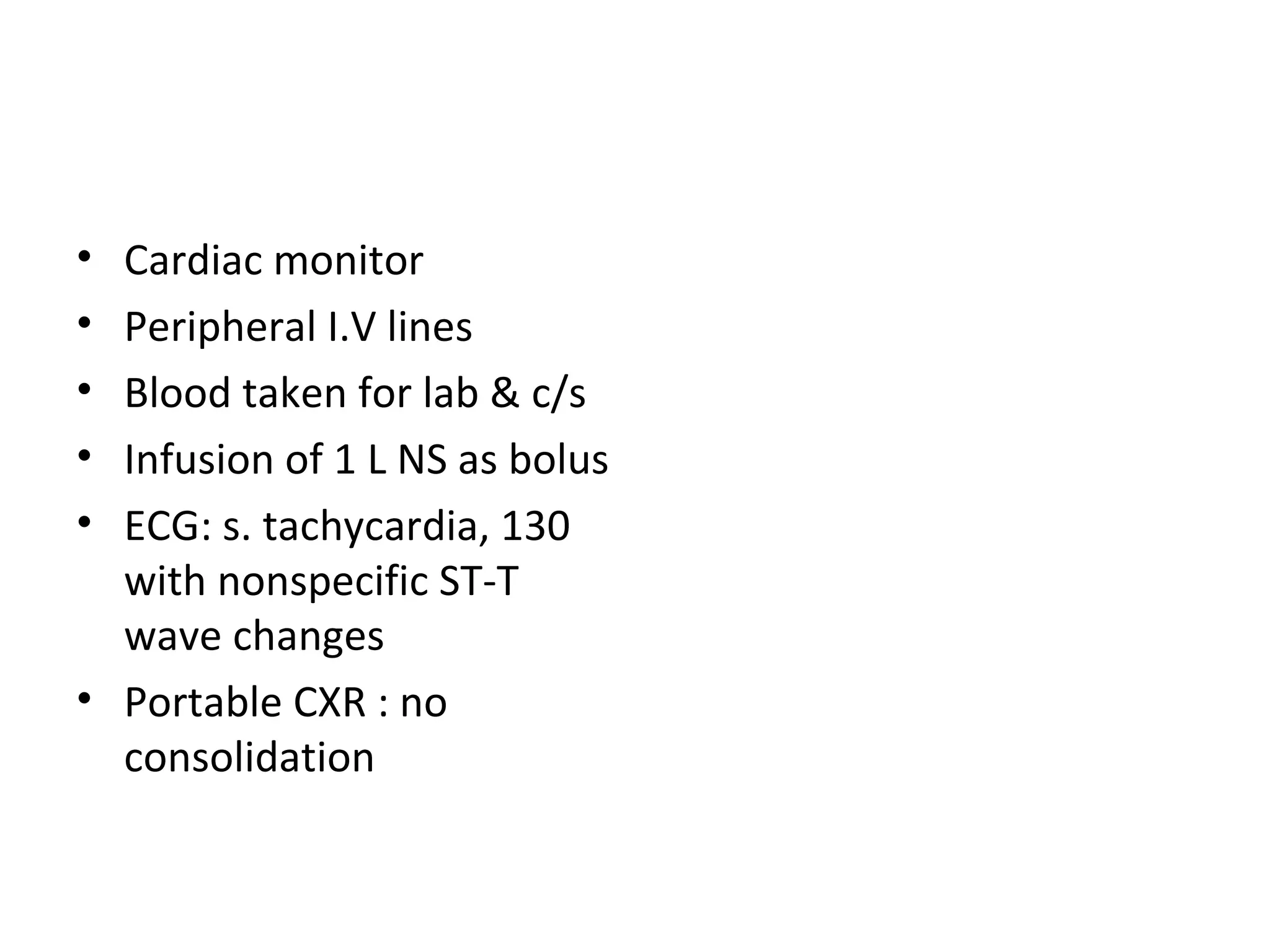
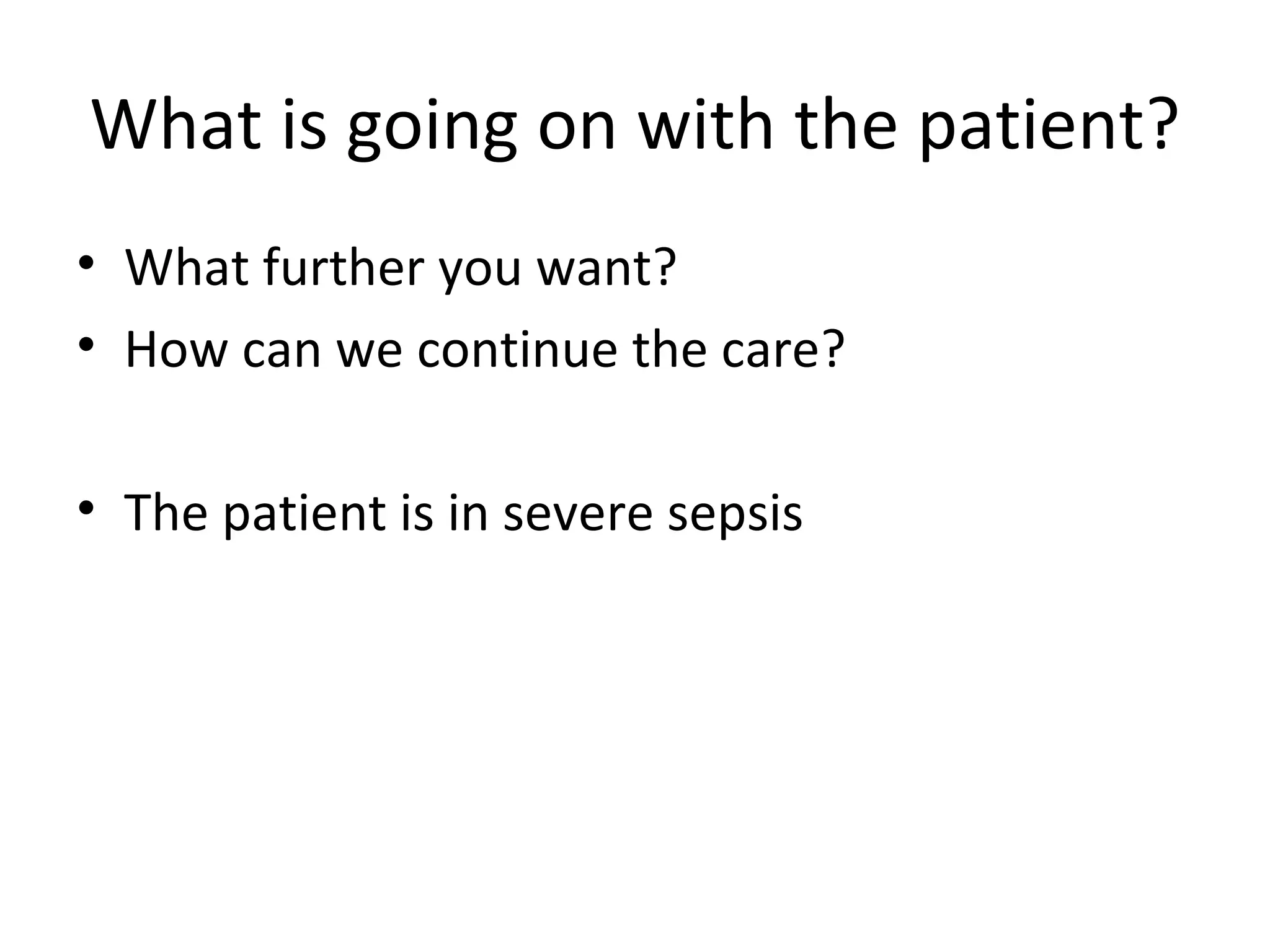
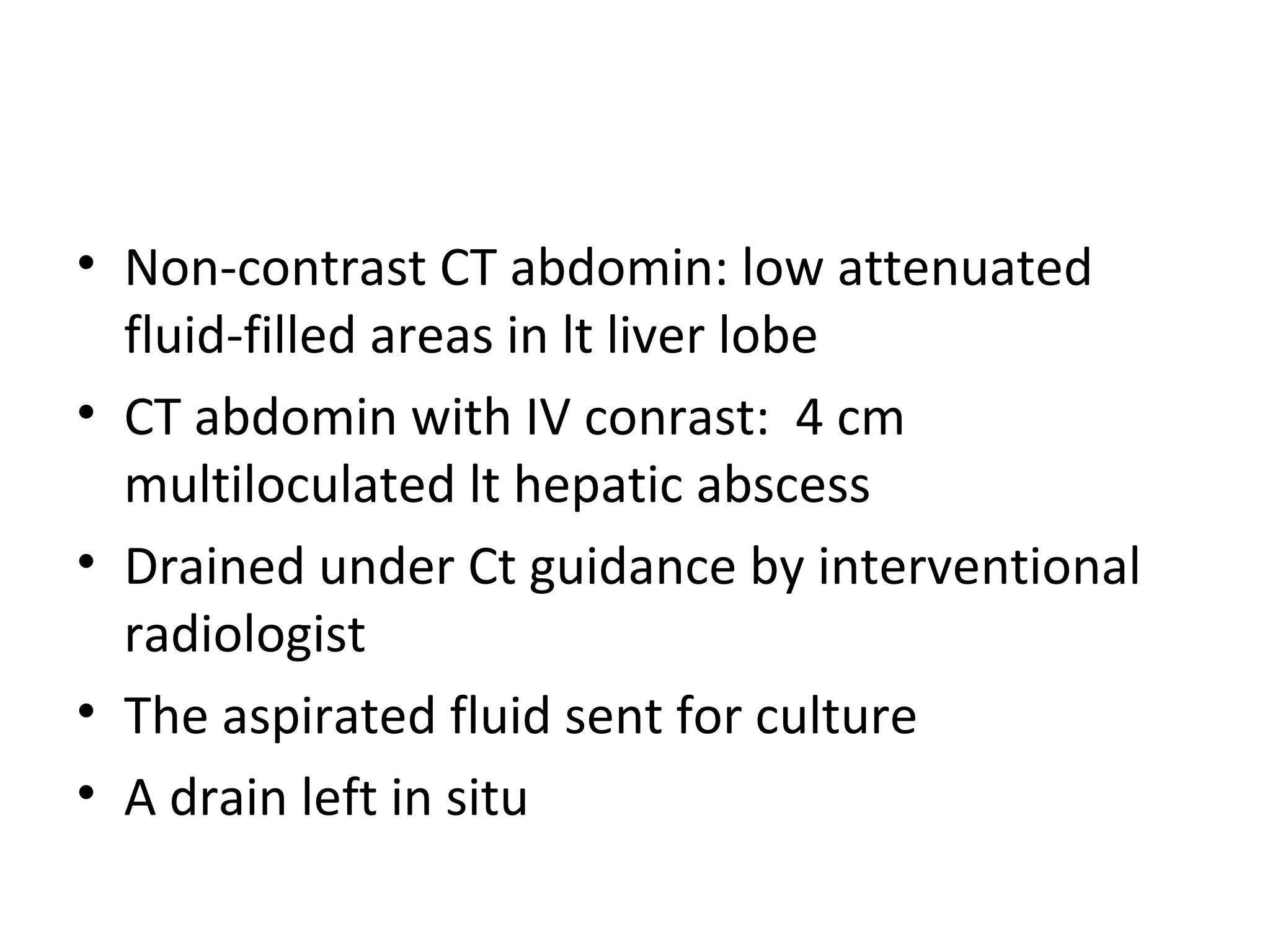
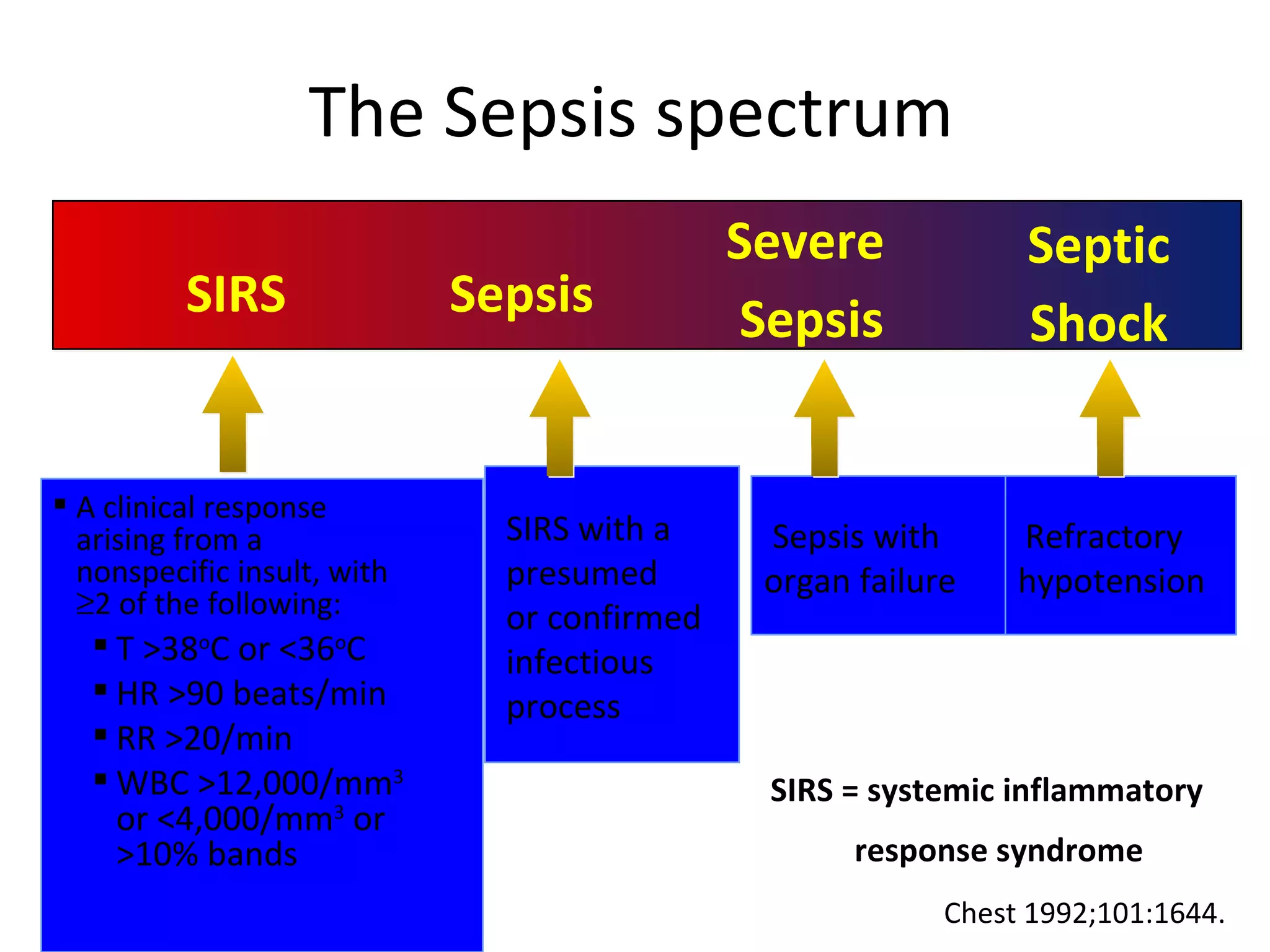
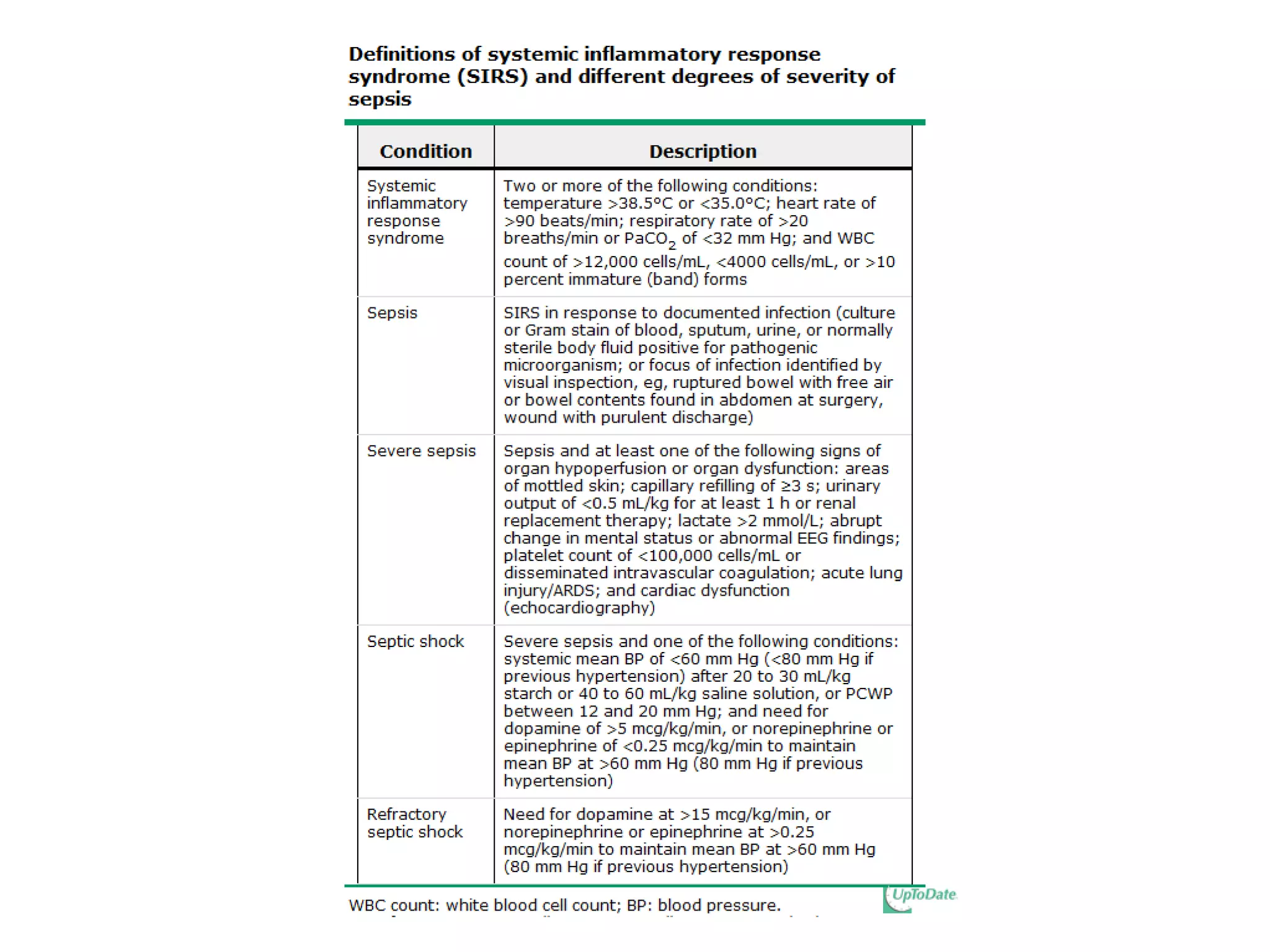
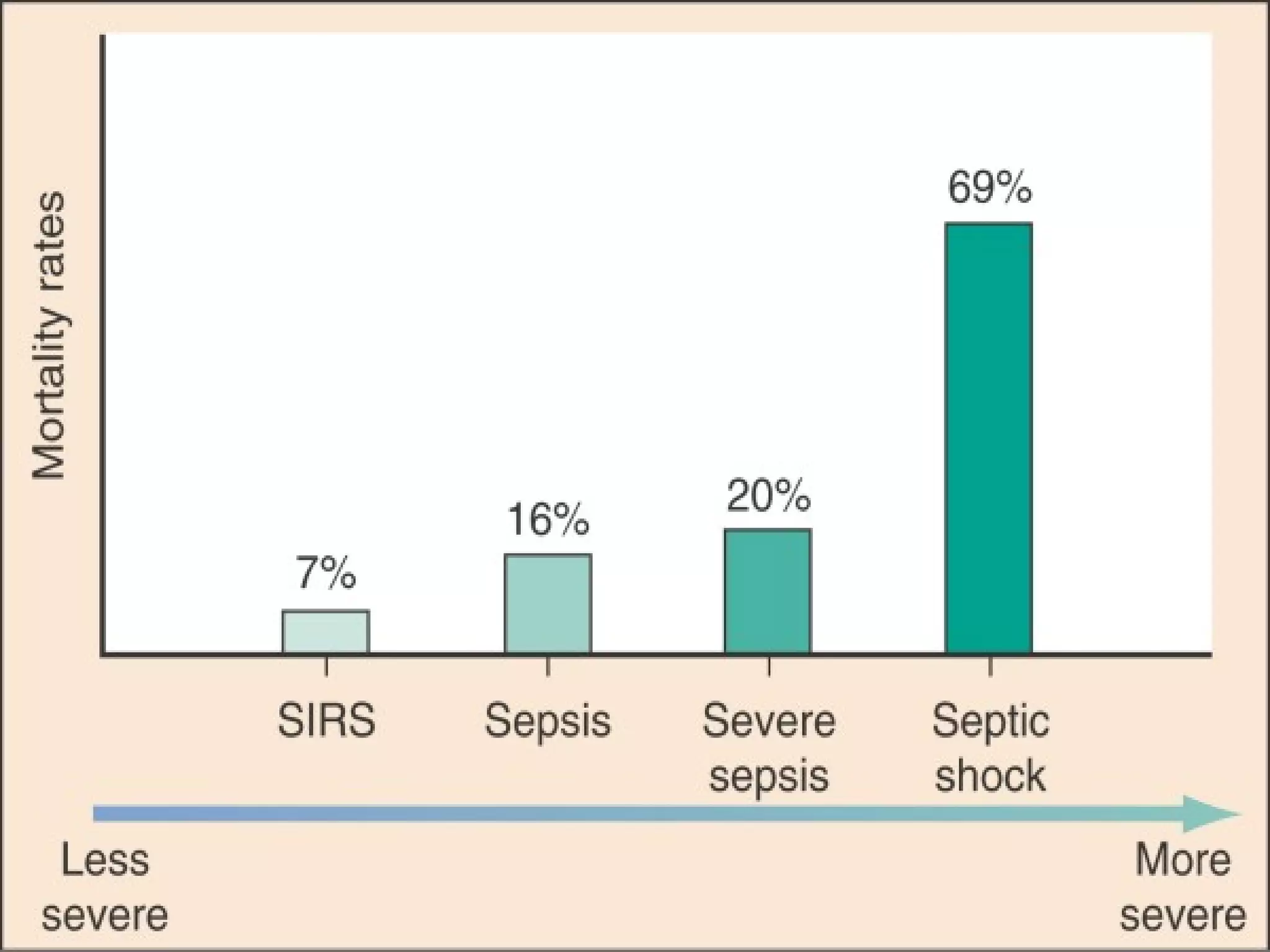
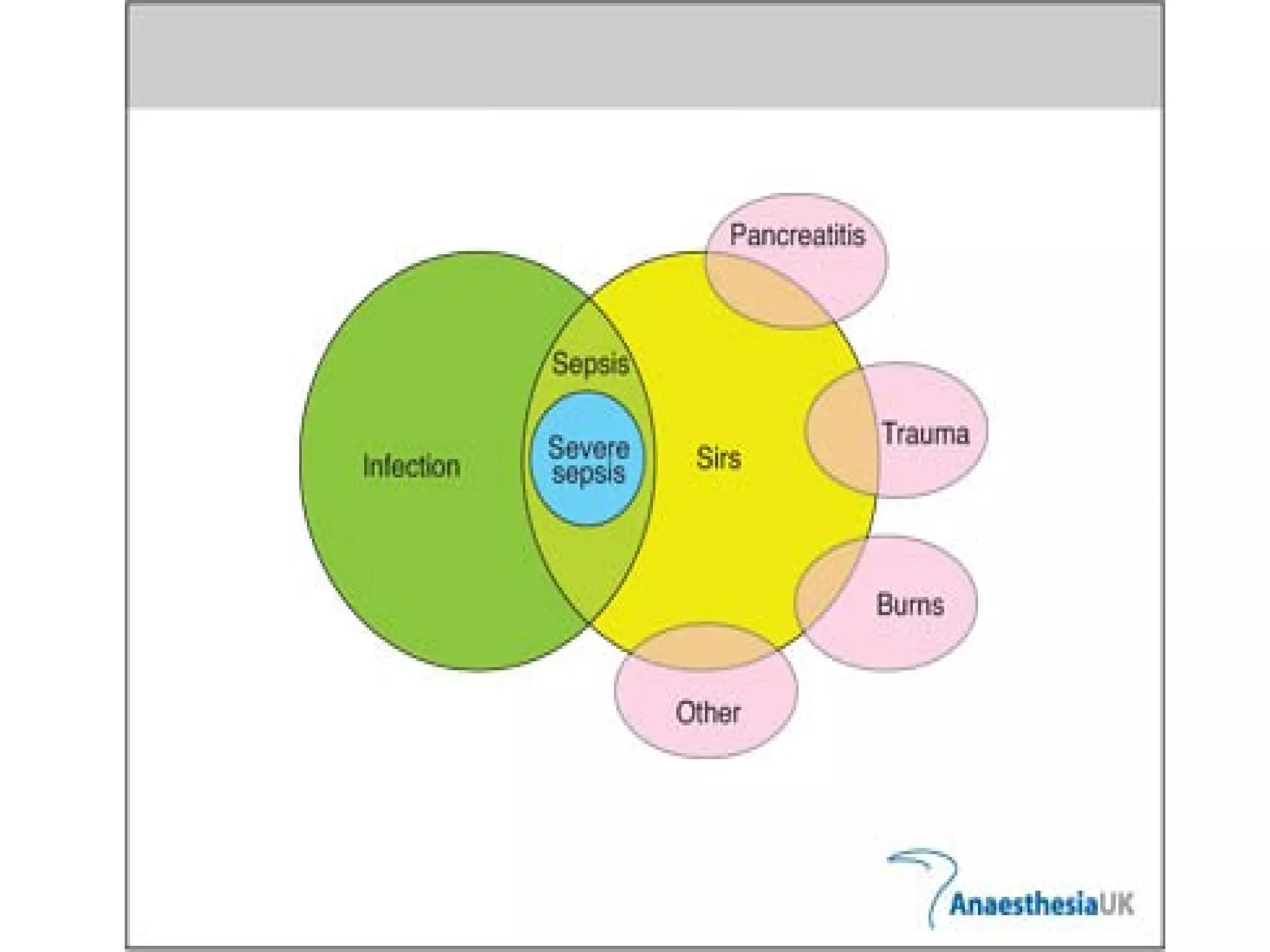
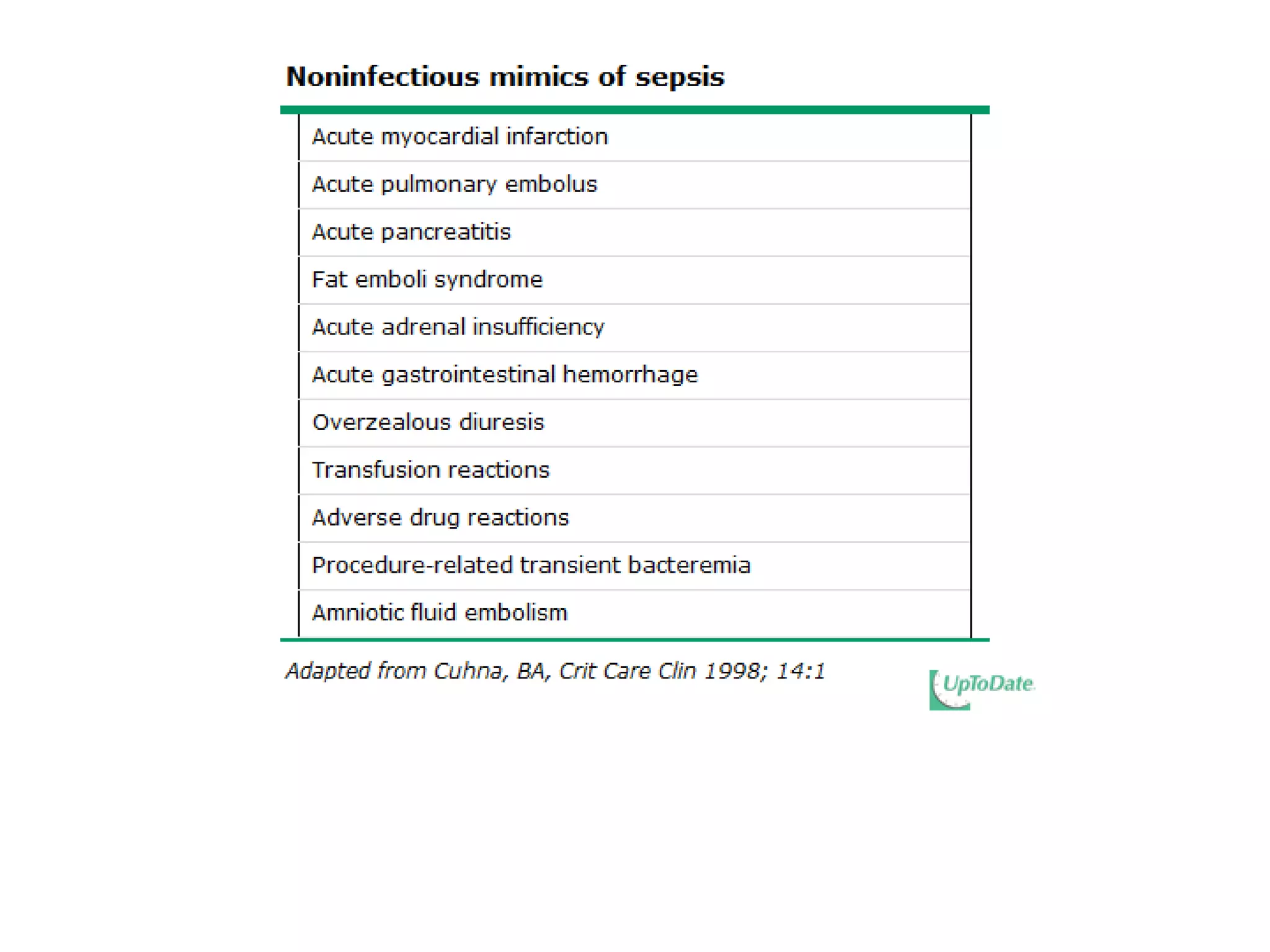
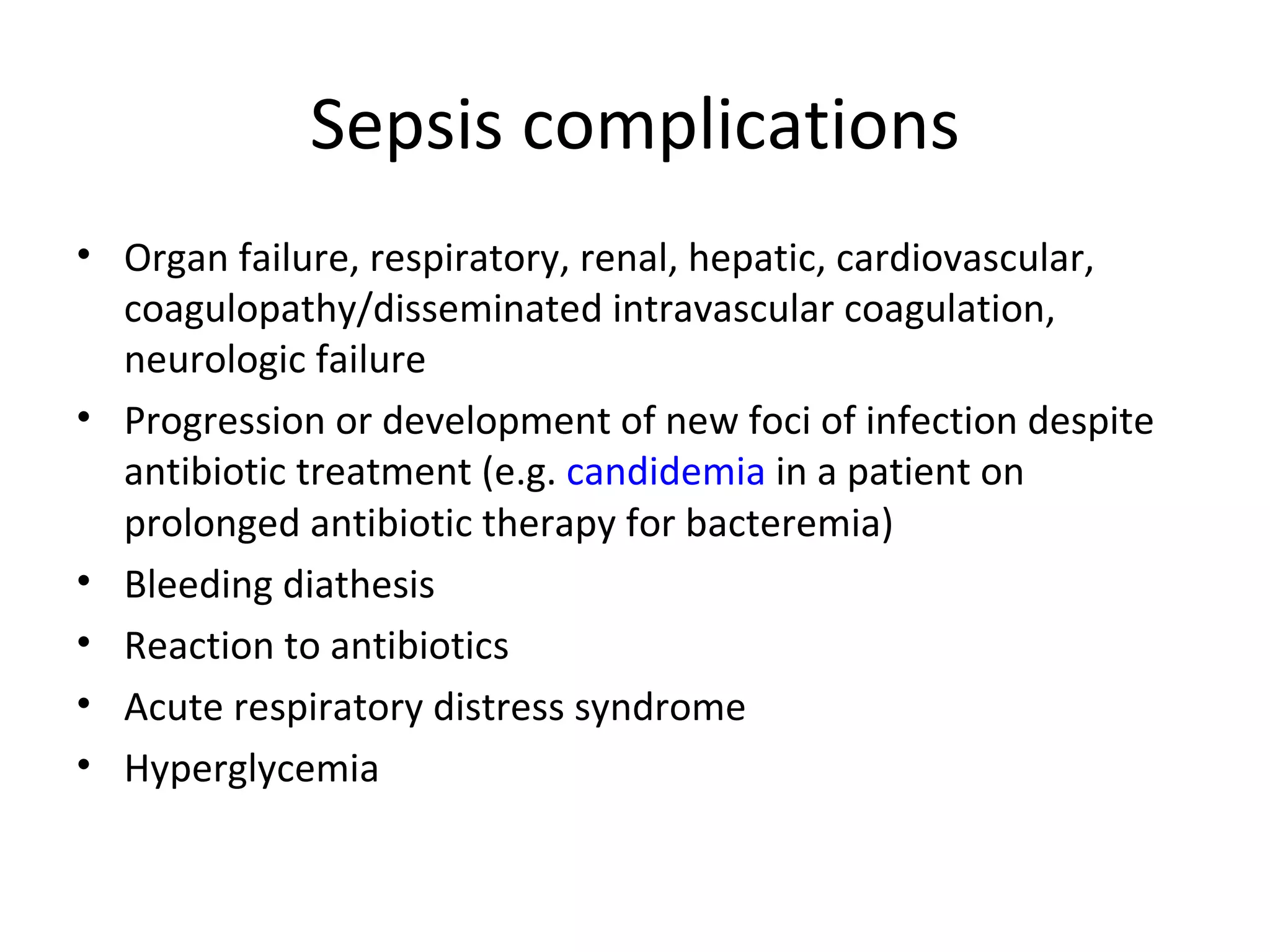
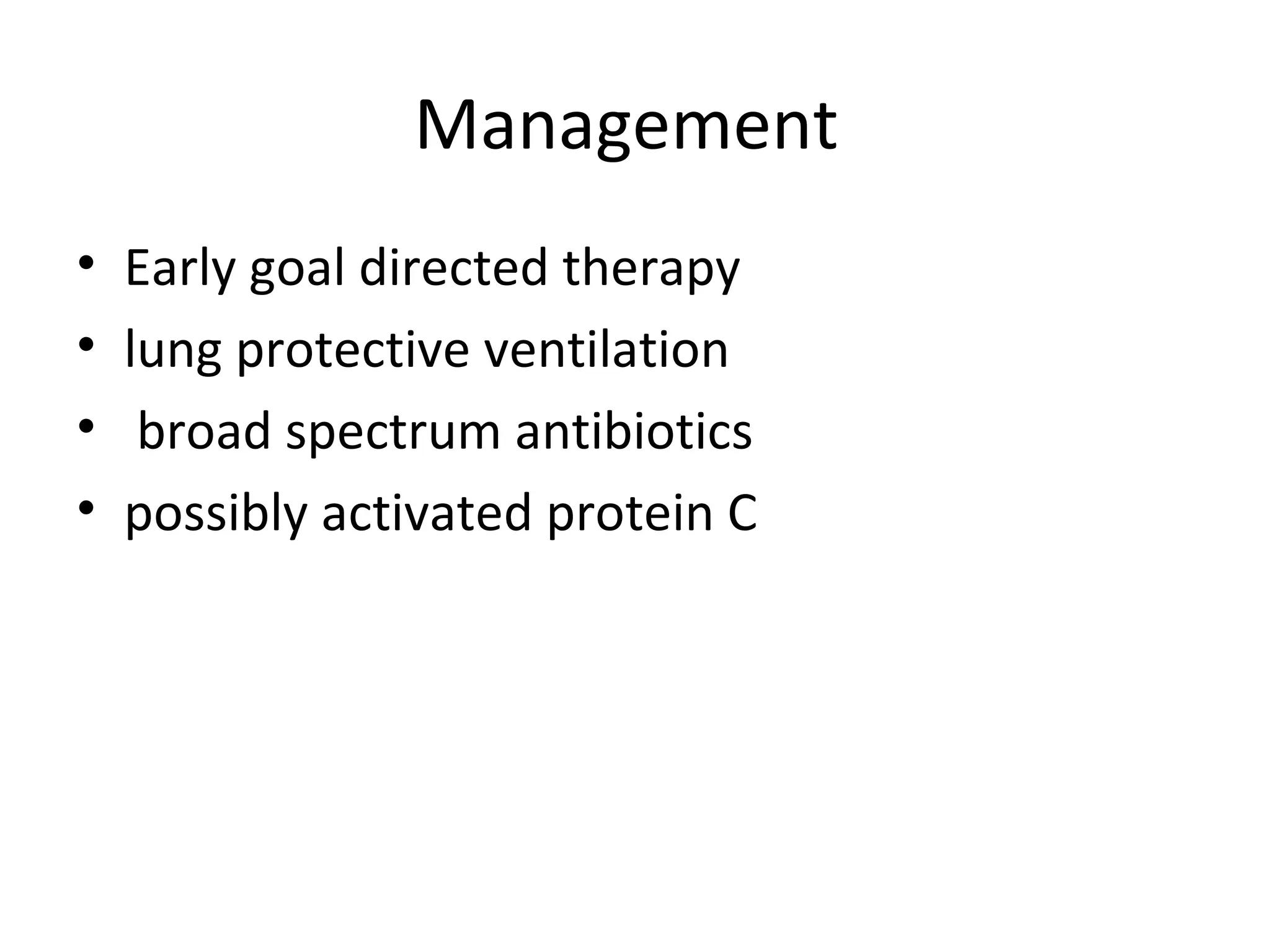
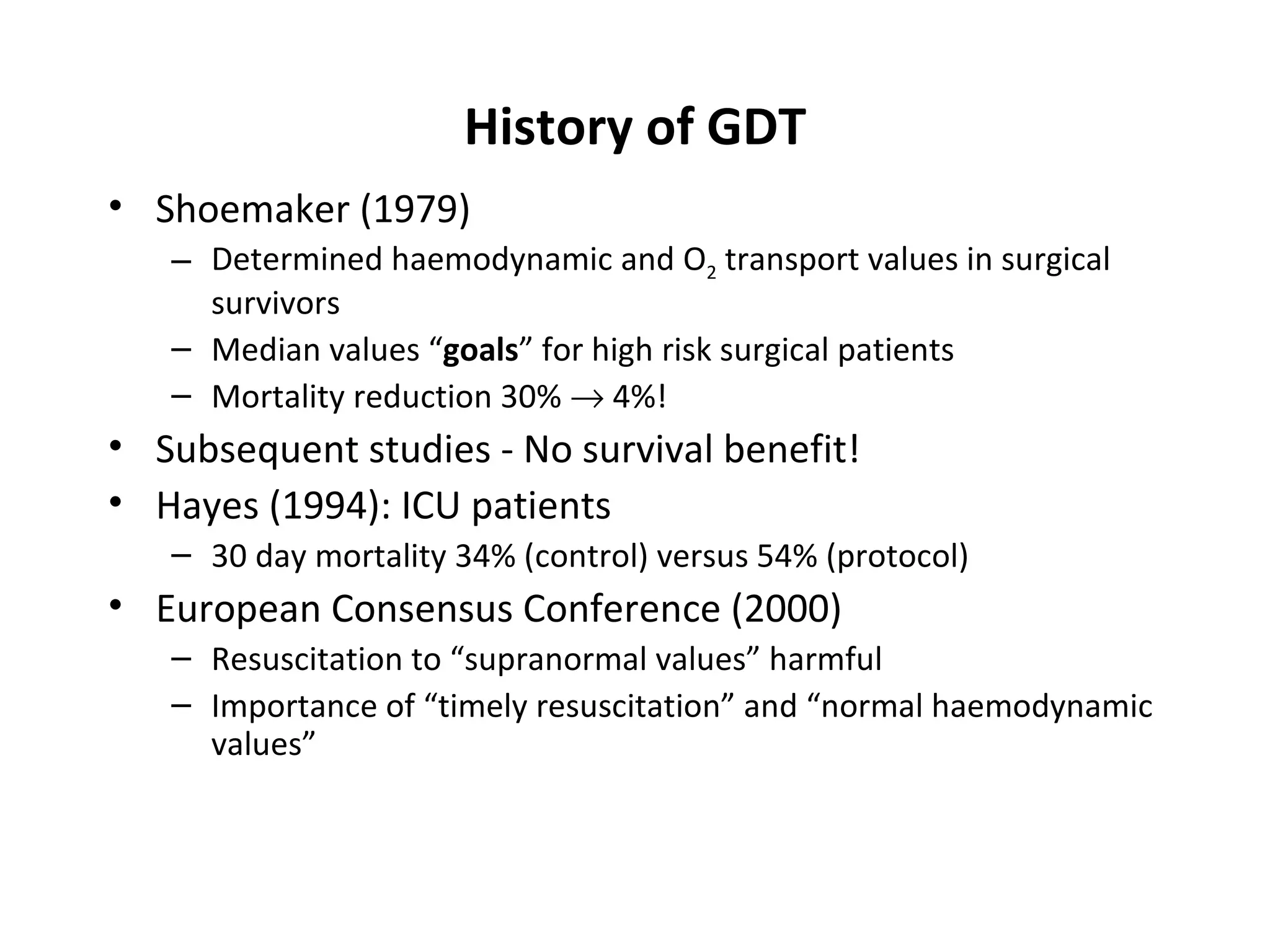
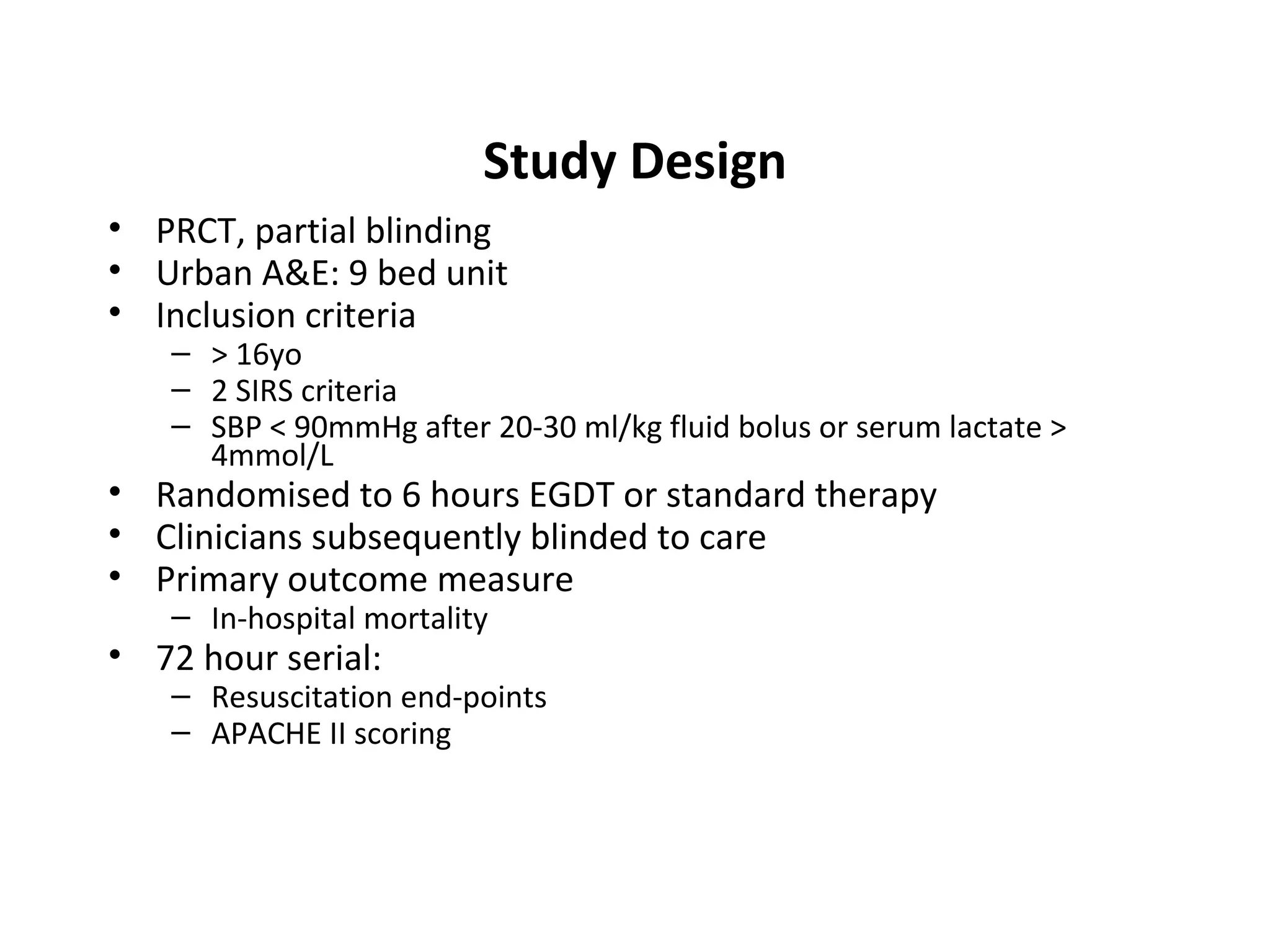
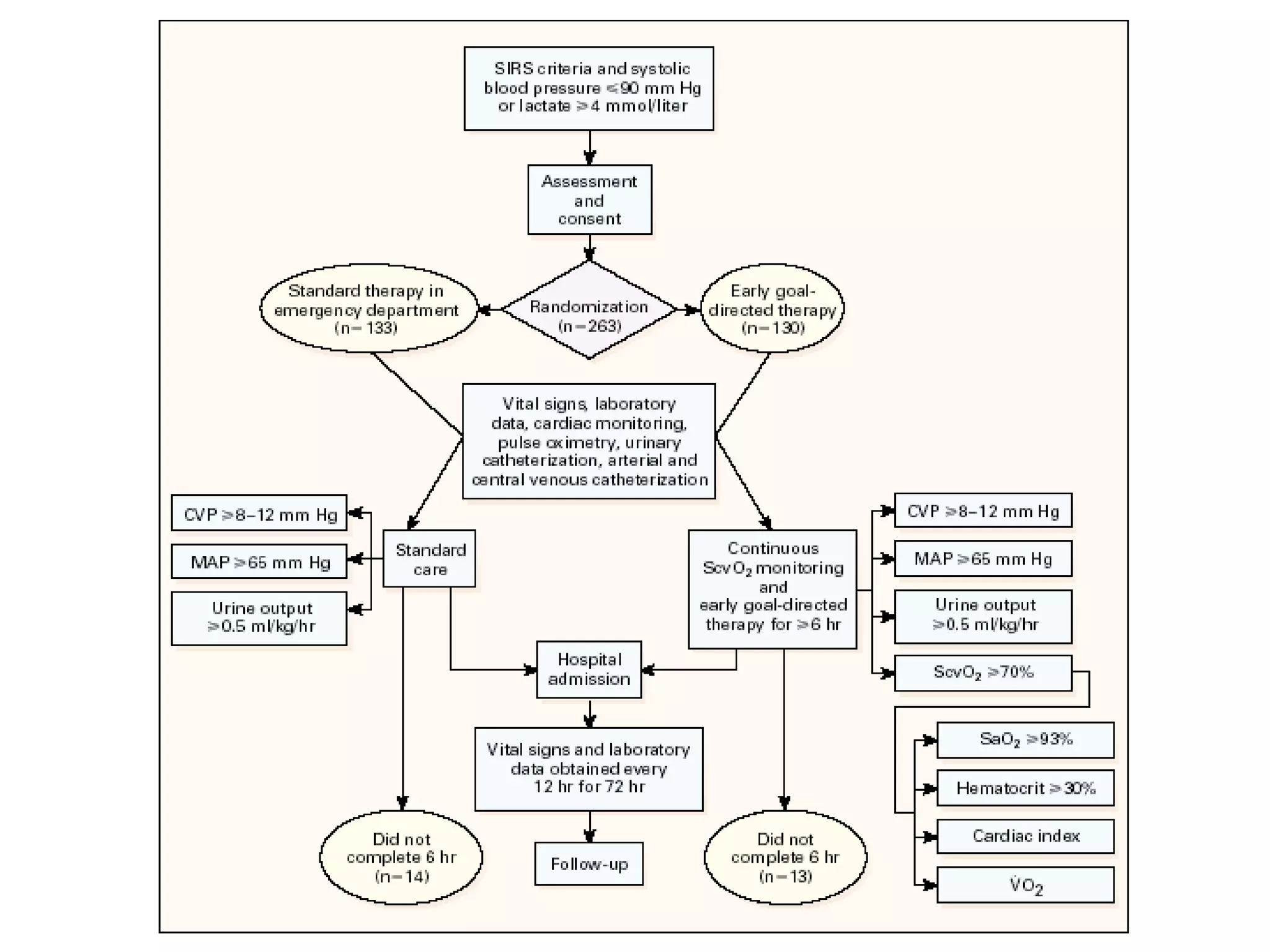
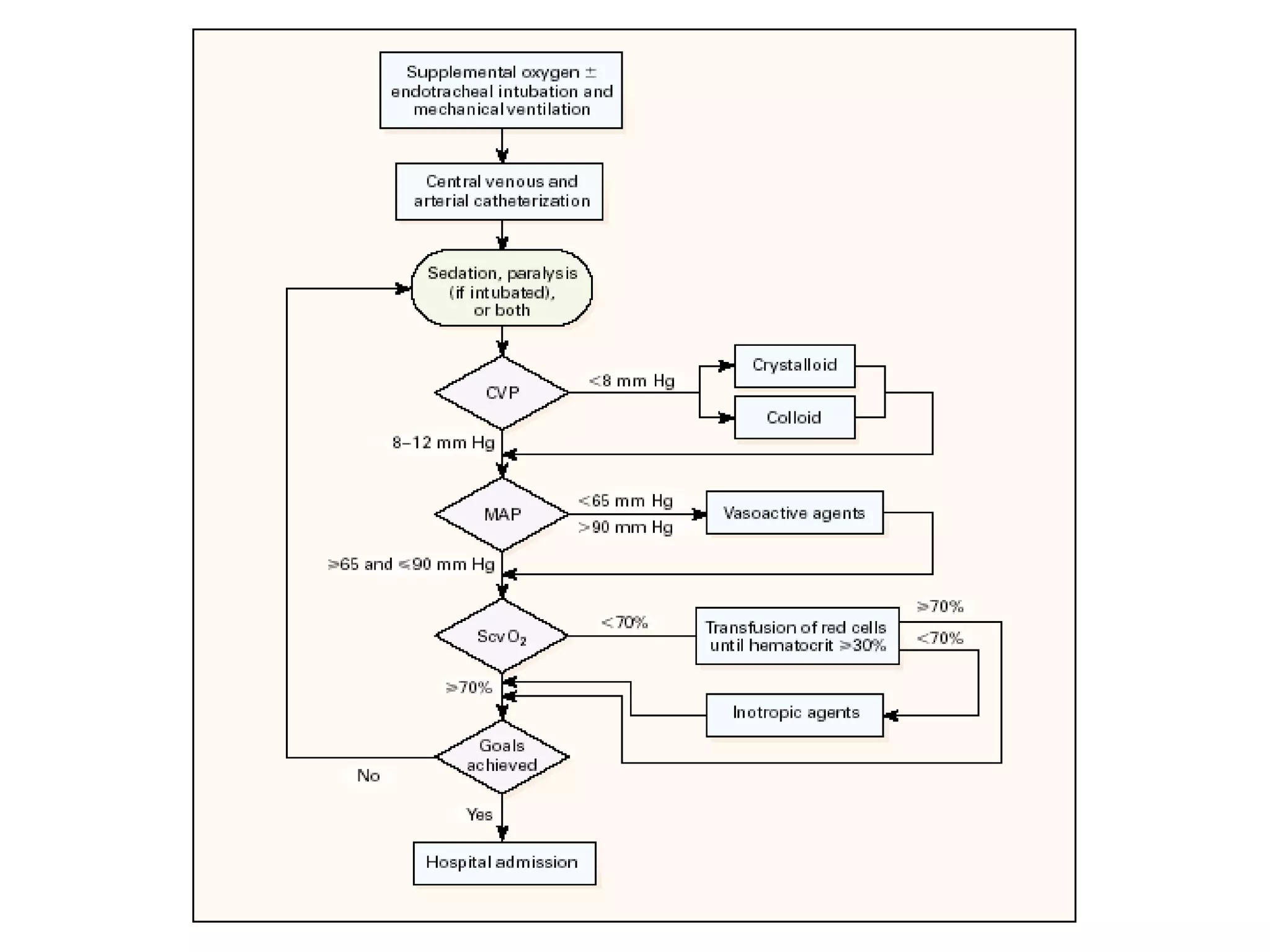
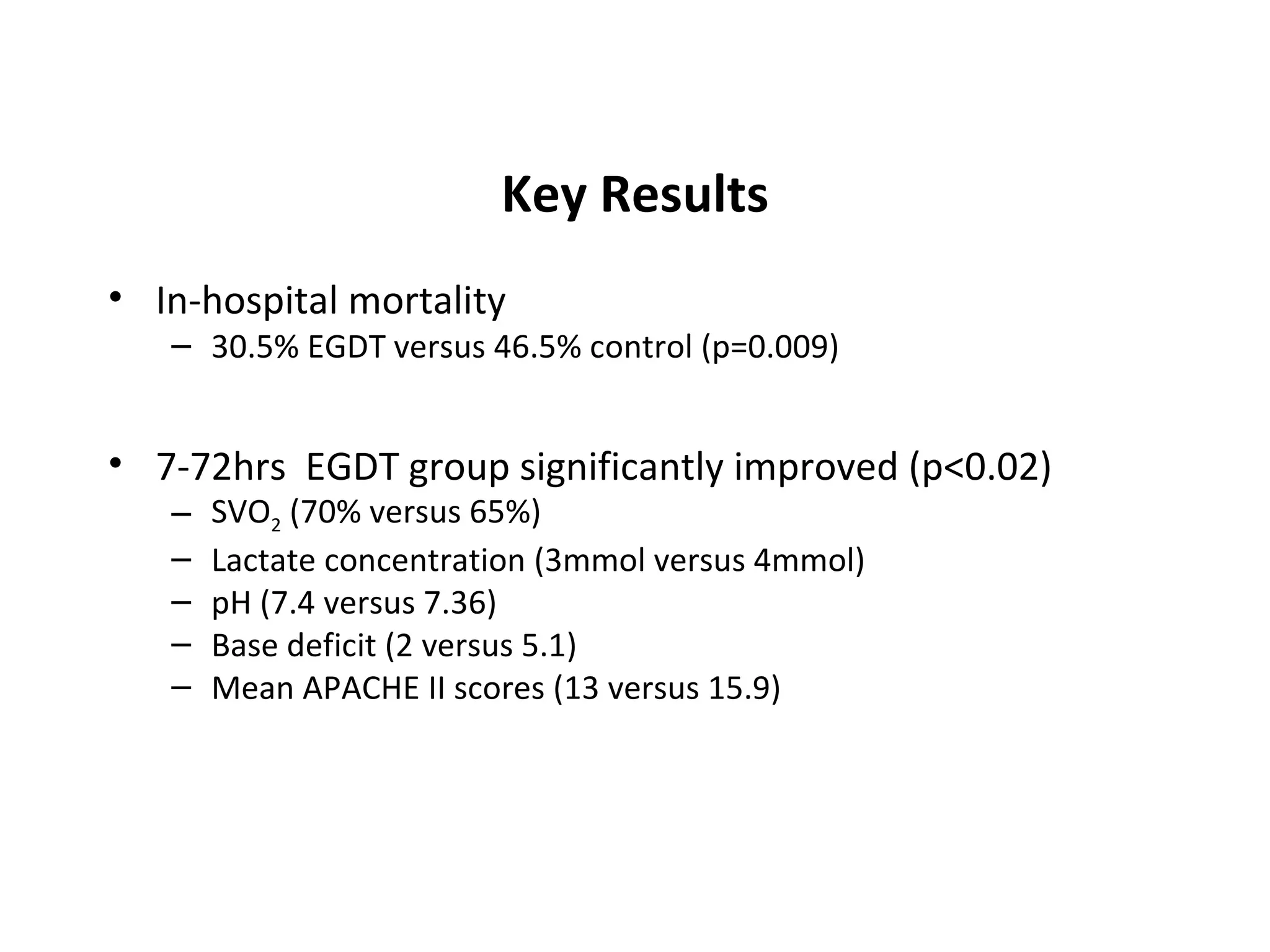
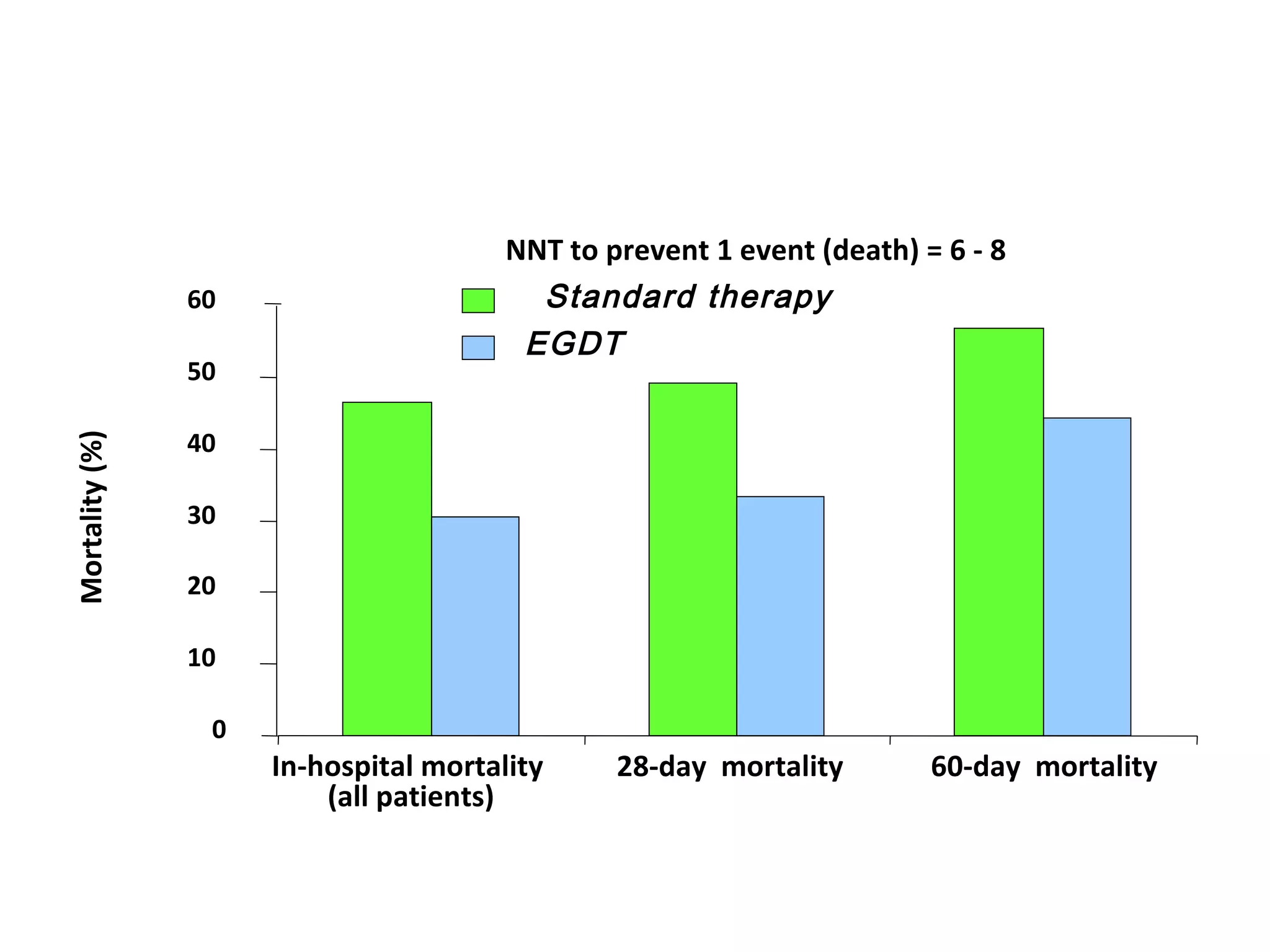
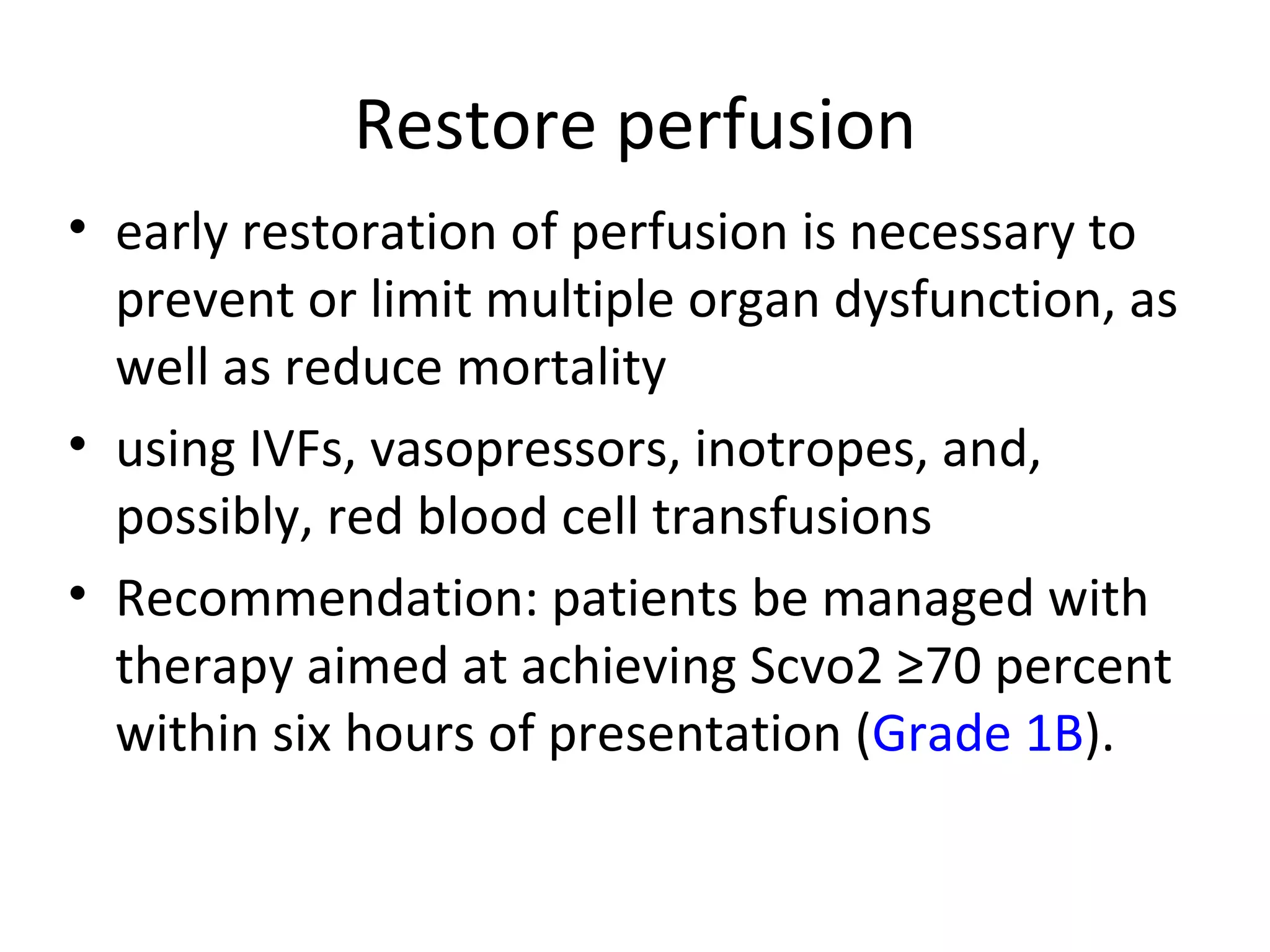
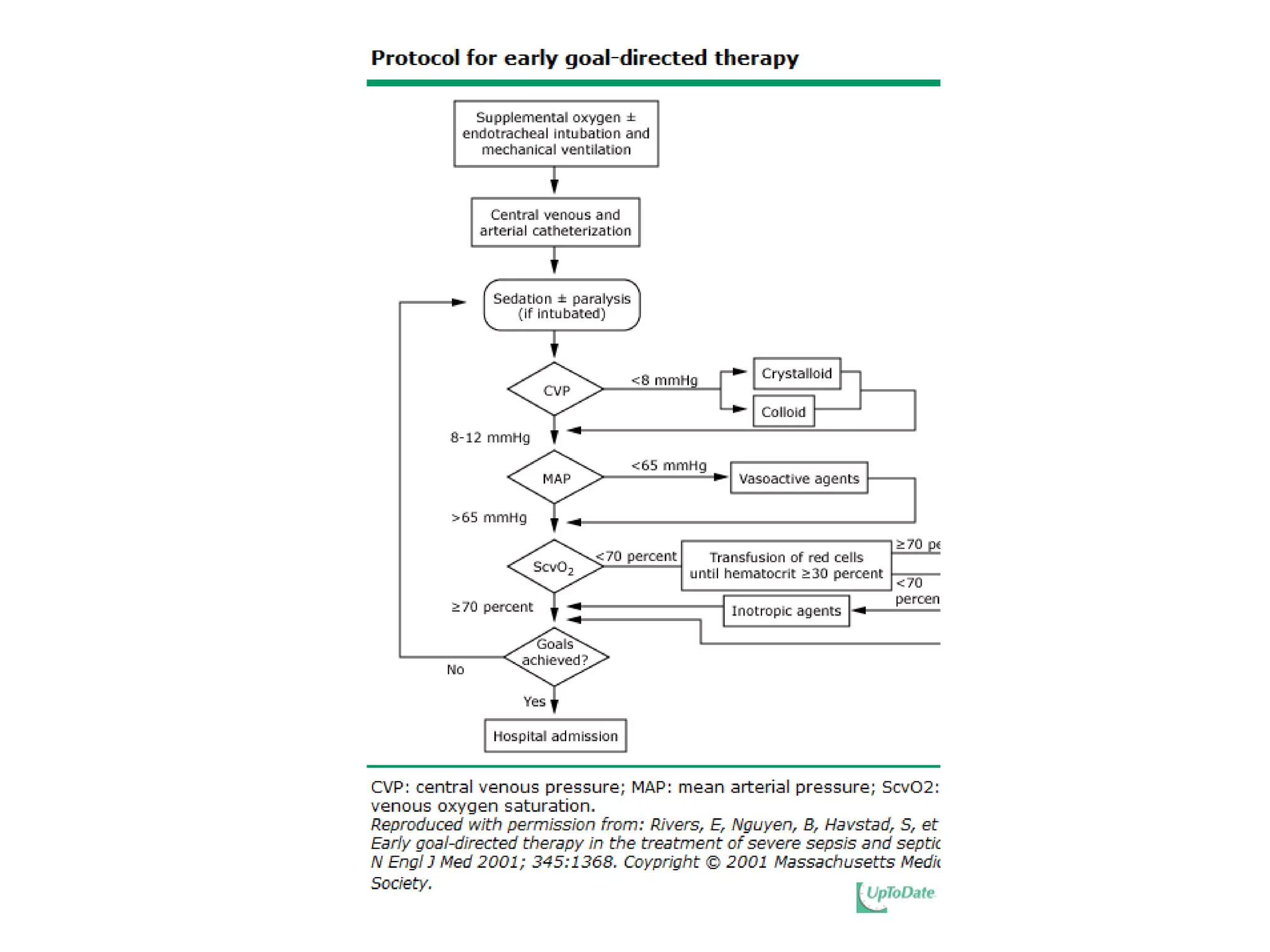
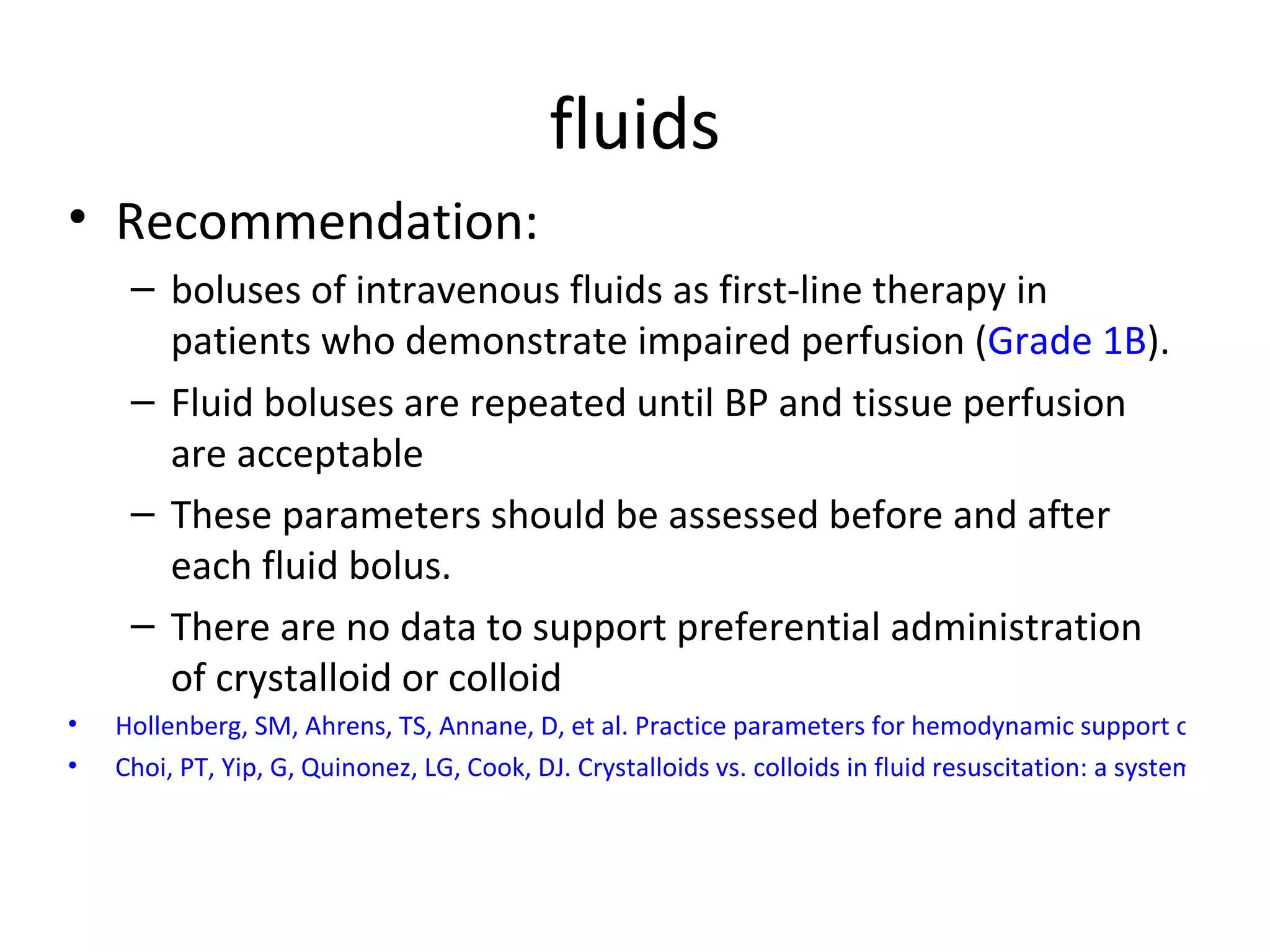
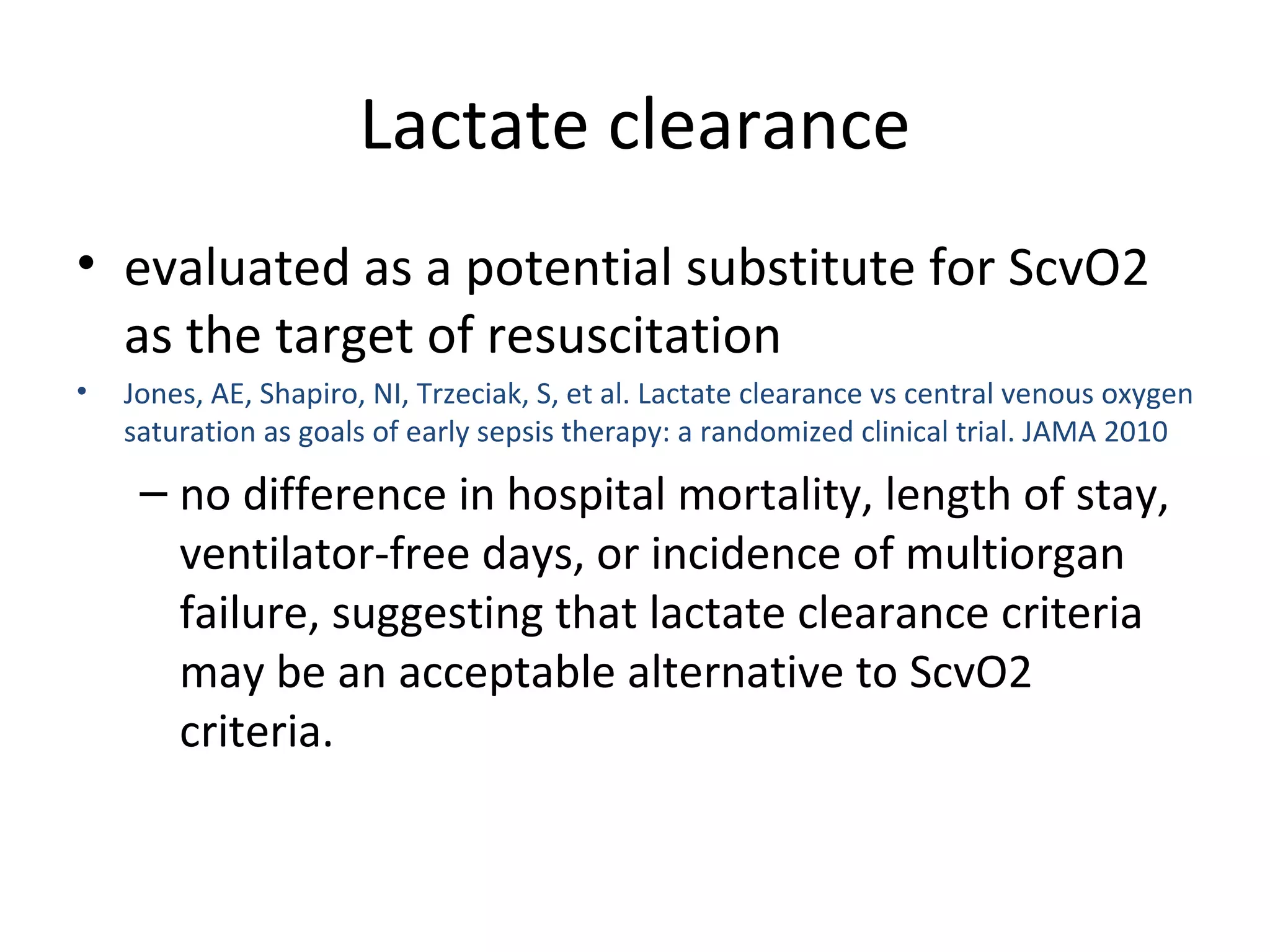
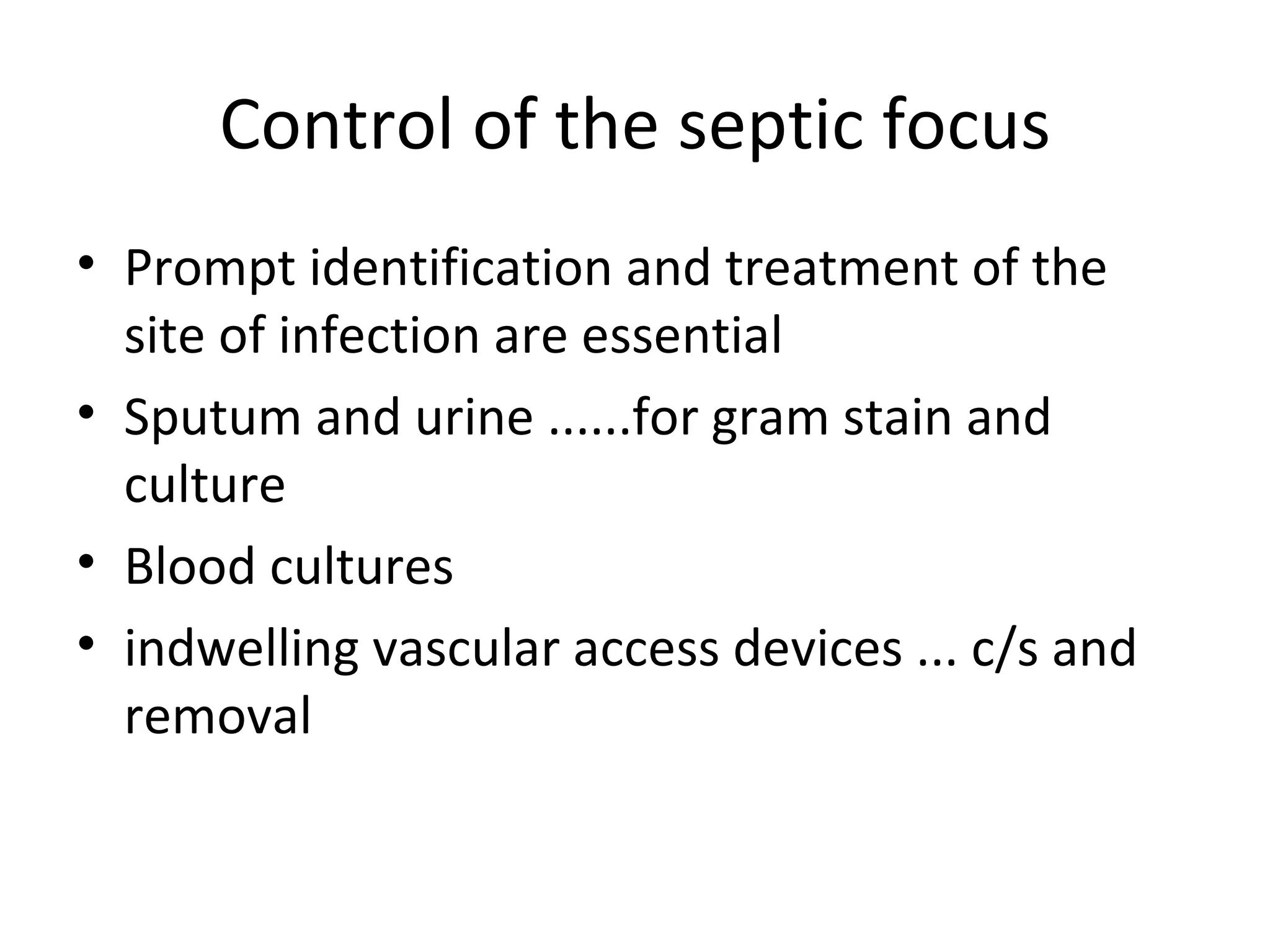
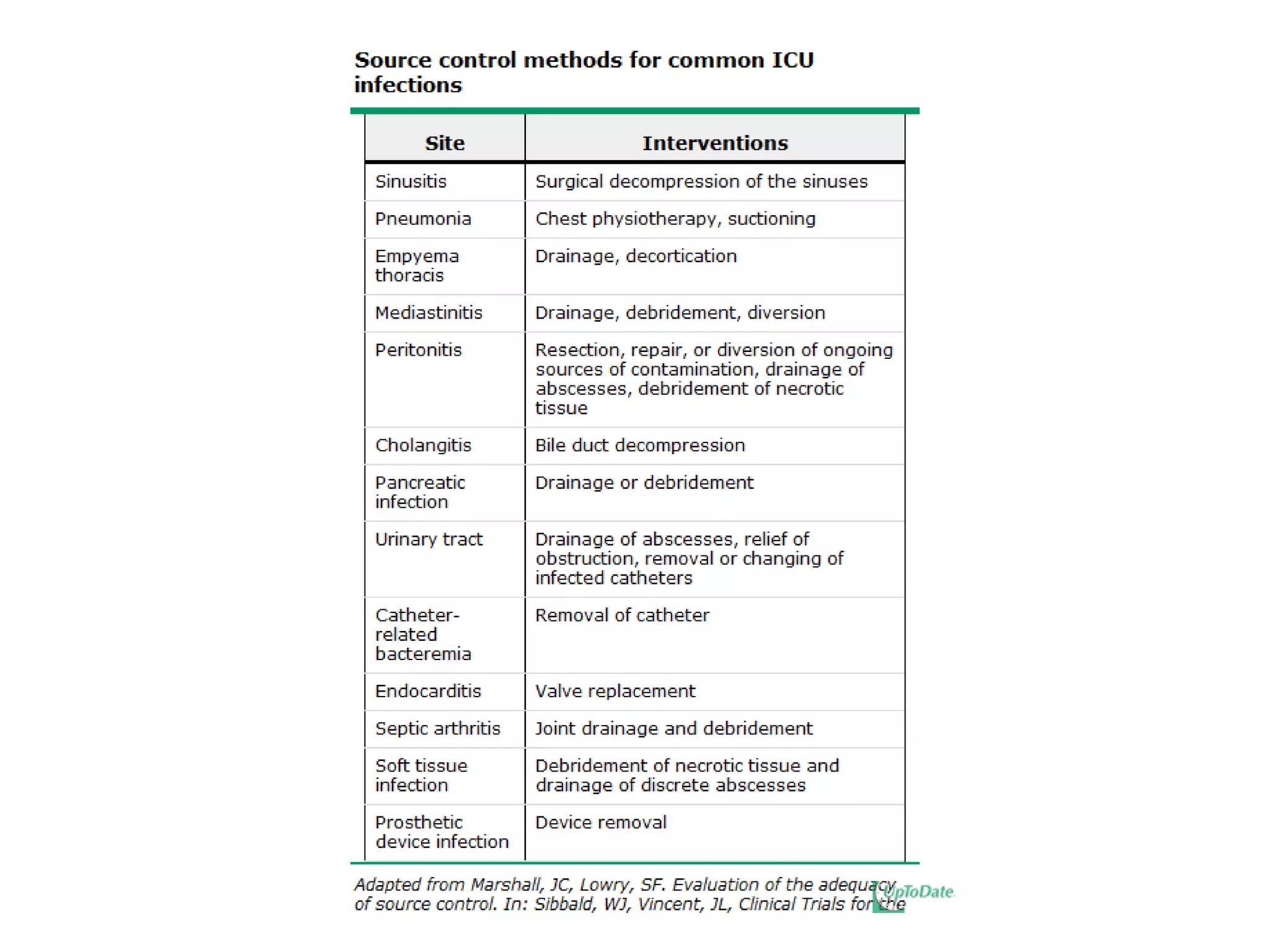
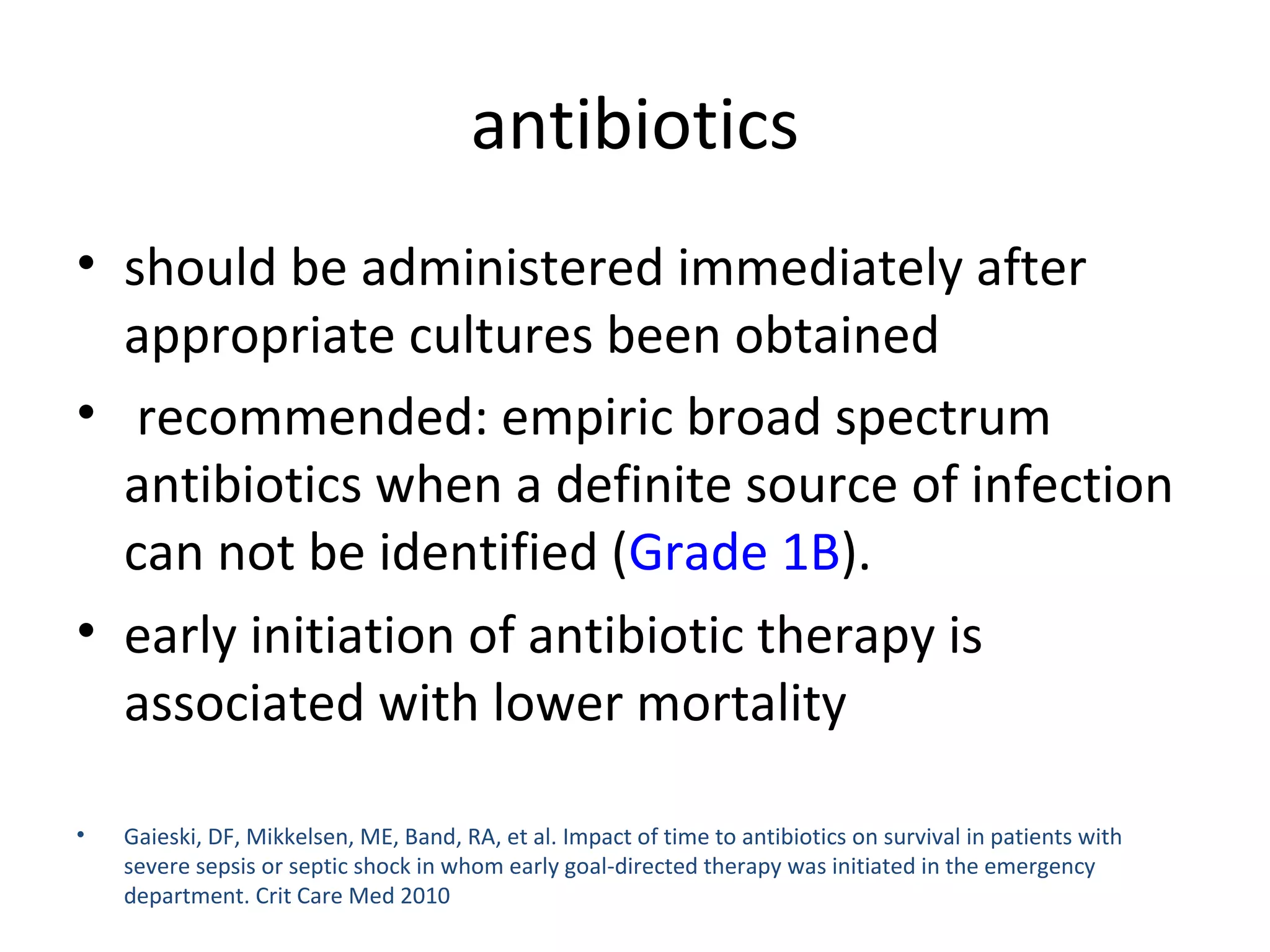
The document discusses the case of a 51-year-old man presenting with severe sepsis and septic shock. It outlines his initial treatment including IV fluids, antibiotics, and vasopressors. Further workup revealed a hepatic abscess which was drained surgically. The patient eventually recovered after 10 days of targeted antibiotic therapy guided by cultures. The document also reviews key literature on defining sepsis, early management principles like early goal-directed therapy, and optimization of oxygen delivery through fluid resuscitation, vasopressors, inotropes, and blood transfusions.
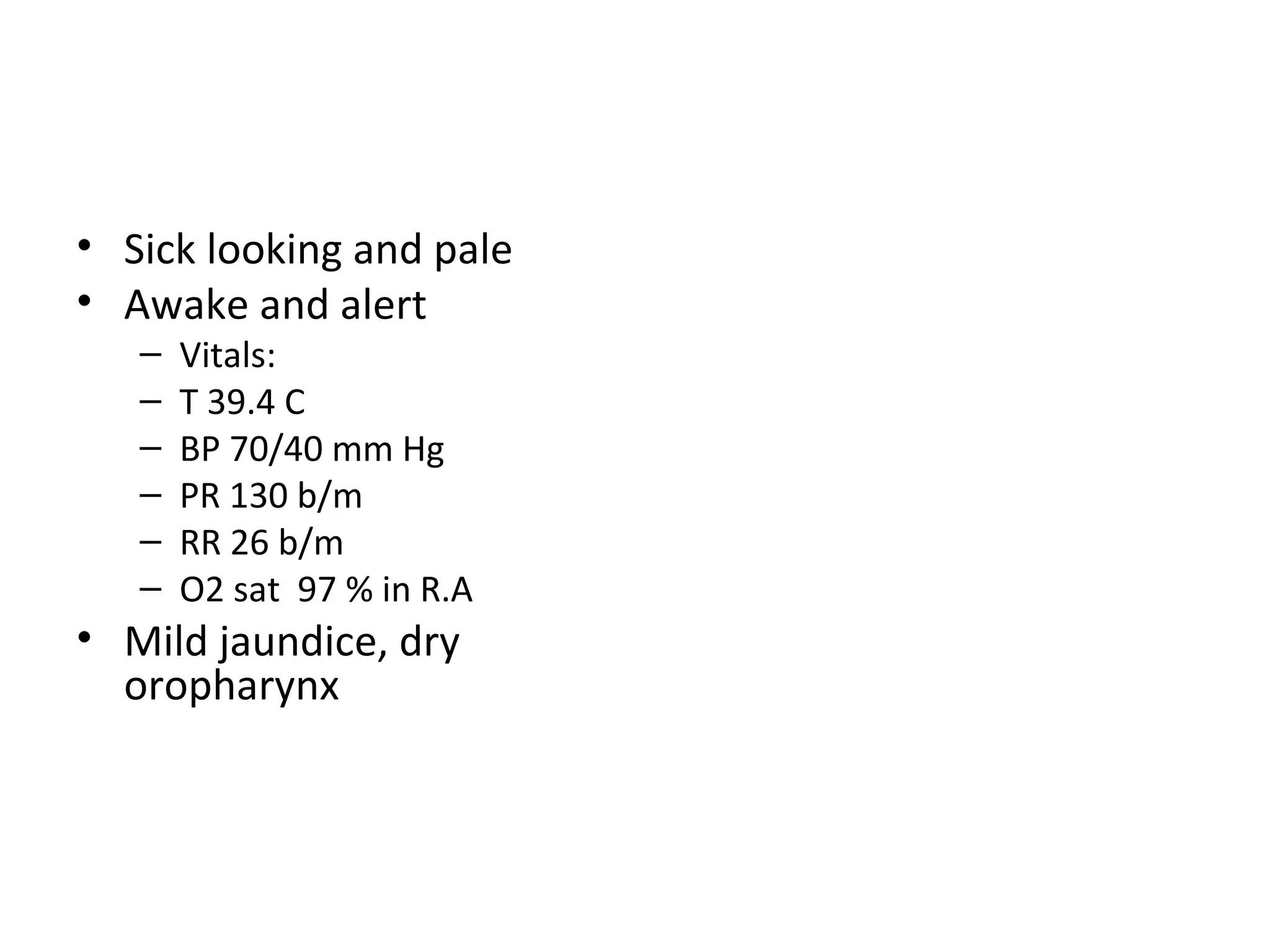
![Cardiac monitor Peripheral I.V lines Blood taken for lab & c/s Infusion of 1 L NS as bolus ECG: s. tachycardia, 130 with nonspecific ST-T wave changes Portable CXR : no consolidation WBC : 2 Hematocrit : 29% PLT: 81 Cr: 1.6 mg/dl[0.8-1.5] T.bili : 2.9 [0.2-1.3] AST: 84 [17-59] ALT: 93 [11-66] ALP: 205 [38-126] Trop: 0.18 [0.00-0.09]](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-8-2048.jpg)
![Additional work-up Lactate 4.6 INR 1.3 Fibrinogen 516[189-434] ABG: ph 7.46, pco2 22, po2 79, hco3 18 base excess -8.1](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-10-2048.jpg)
![Additional work-up Lactate 4.6 INR 1.3 Fibrinogen 516[189-434] ABG: ph 7.46, pco2 22, po2 79, hco3 18 base excess -8.1 He received 5 L NS, no much improvement Norepi. Drip started CVC and ScvO2 monitor were placed Emperic broad spectrum antibiotics given Pt admitted to ICU](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-11-2048.jpg)
![Blood & fluid c/s : strep constellatus [viridans] Antibotics changed according to sensitivity Patient was d/c after 10 days](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-13-2048.jpg)

![EGDT Rivers & colleagues [ rivers E,Nguyen B,havstad S,et al. early goal-directed therapyin the treatment of severe sepsis and septic shock. N Engl J Med 2001 ] RCT Pts with severe sepsis and septic shock Pt enrolled to either EGDT during the first 6 hrs or the standard therapy](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-24-2048.jpg)
![Crystalloids given to keep CVP at 8-12mmHg Vasopressors added if MAP < 65 mmHg PRBCs transfusion if ScvO2 [ central venous oxygen saturation] < 70% to maintain hematocrit > 30% Conclusion : decreased mortality at 28 and 60 days & decreased duration of hospitalization](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-26-2048.jpg)

![Activated protein C 24 mic/kg/hr for 96 hrs Reported to decrease mortality and to ameliorate organ dysfunction in Pts with severe sepsis [ APACHE2 score > 25 or dysfunction 2 or more organs ]… decrease mortality by 13 % Not beneficial in low risk Pts Ely EW, Laterre PF,Angus DC, et al. Drotrecogin alfa (activated) administration across clinically important subgroup of Pts with severe sepsis. Crit Care Med 2003](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-51-2048.jpg)


![29 % of infected Ptswith elevated lactate were normotensive- yet if lactate not cleared within 6 hrs, their mortality ----- 55 % Normal BP doesnot equate to effective end-organ perfusion When lactate is elevated, the Pt is in critical but potentially reversible situation [ O2 delivery is not meeting demand ] Nguyen HB,rivers EP,knoblichBP, et al.Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med 2004](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-59-2048.jpg)
![Lung protective mechanical ventilation Use tidal volume 6cc/kg [ not 12cc/kg ]shown to decrease mortality rate from 40% to 31 %, to reduce organ dysfunction, to lower level of cytokines Ranieri VM, Suter PM,Tortorella C, et al. Effect of mechanical ventilation on inflammatry mediators in pts with ARDS : RCT. JAMA 1999](https://image.slidesharecdn.com/optimzingsepsismanagement-101221112719-phpapp02/75/Optimzing-sepsis-management-60-2048.jpg)