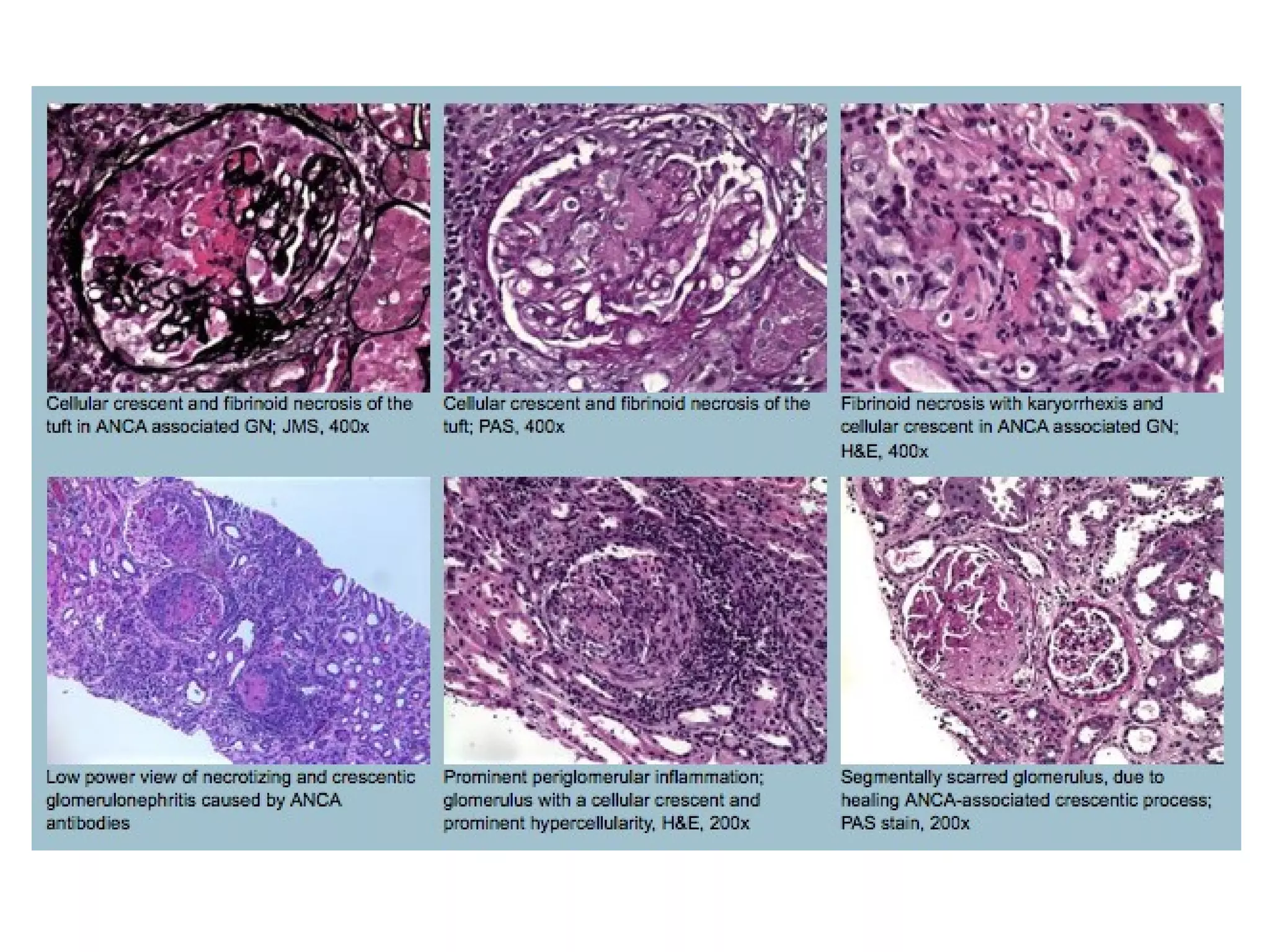
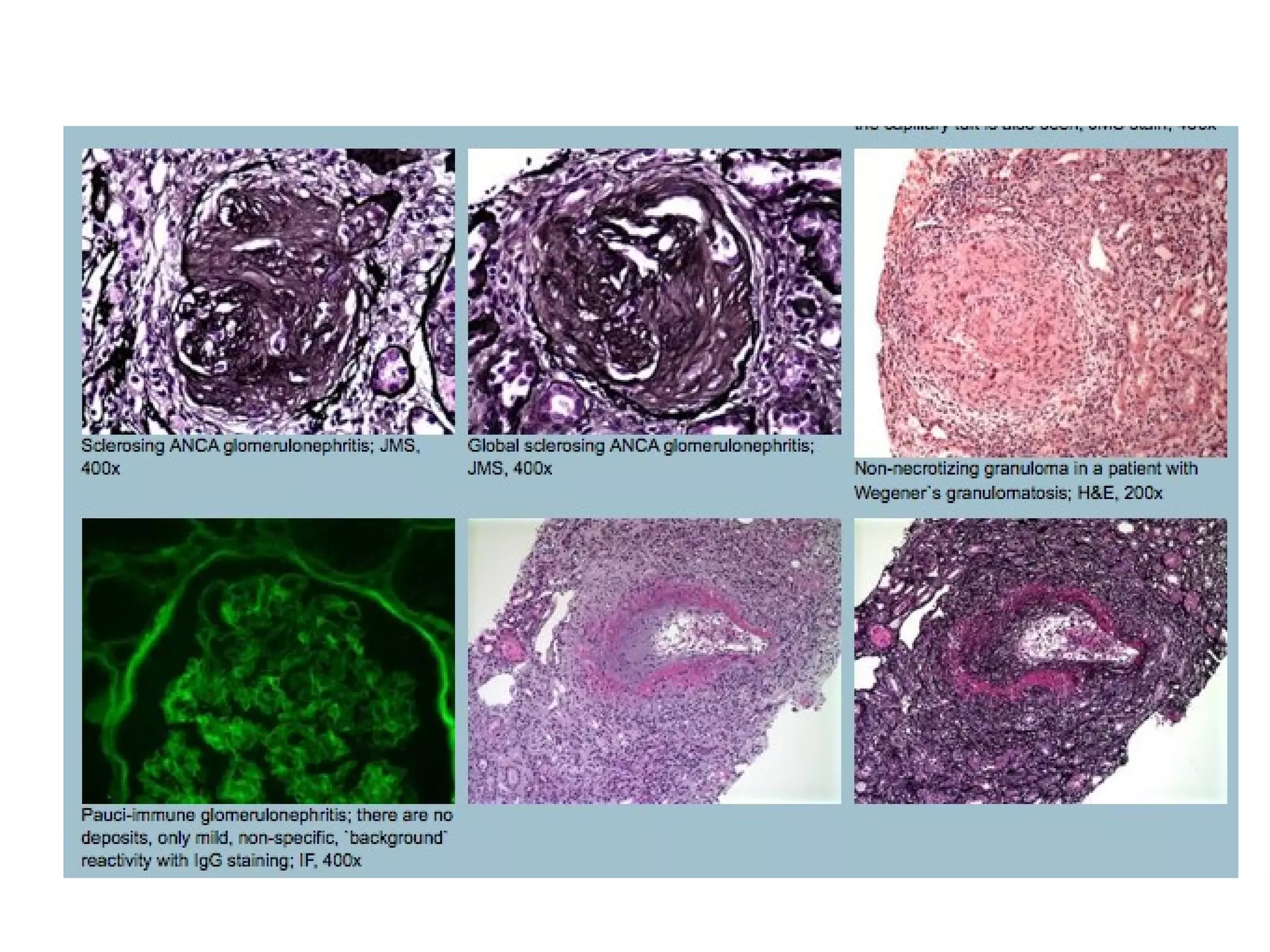
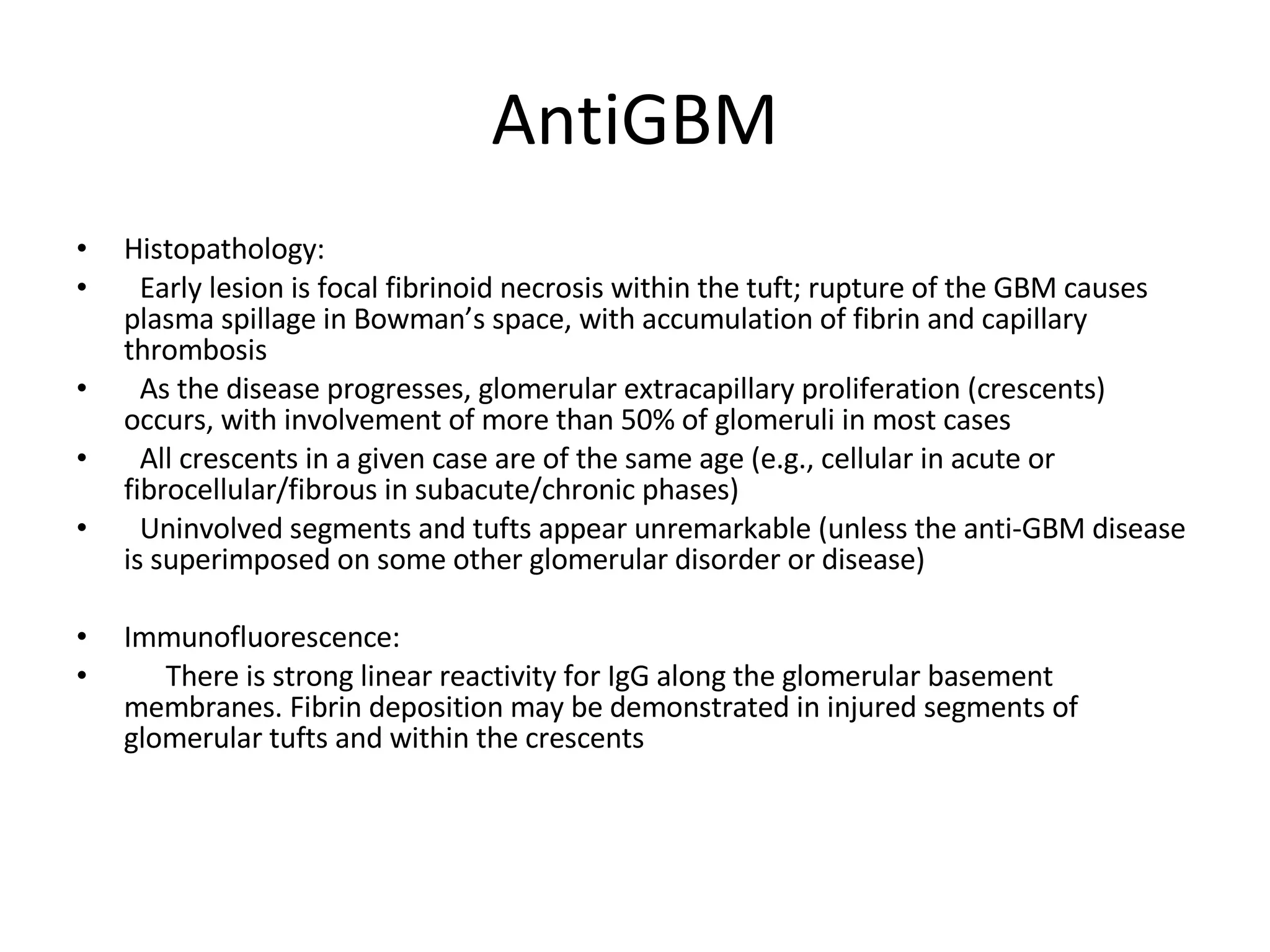
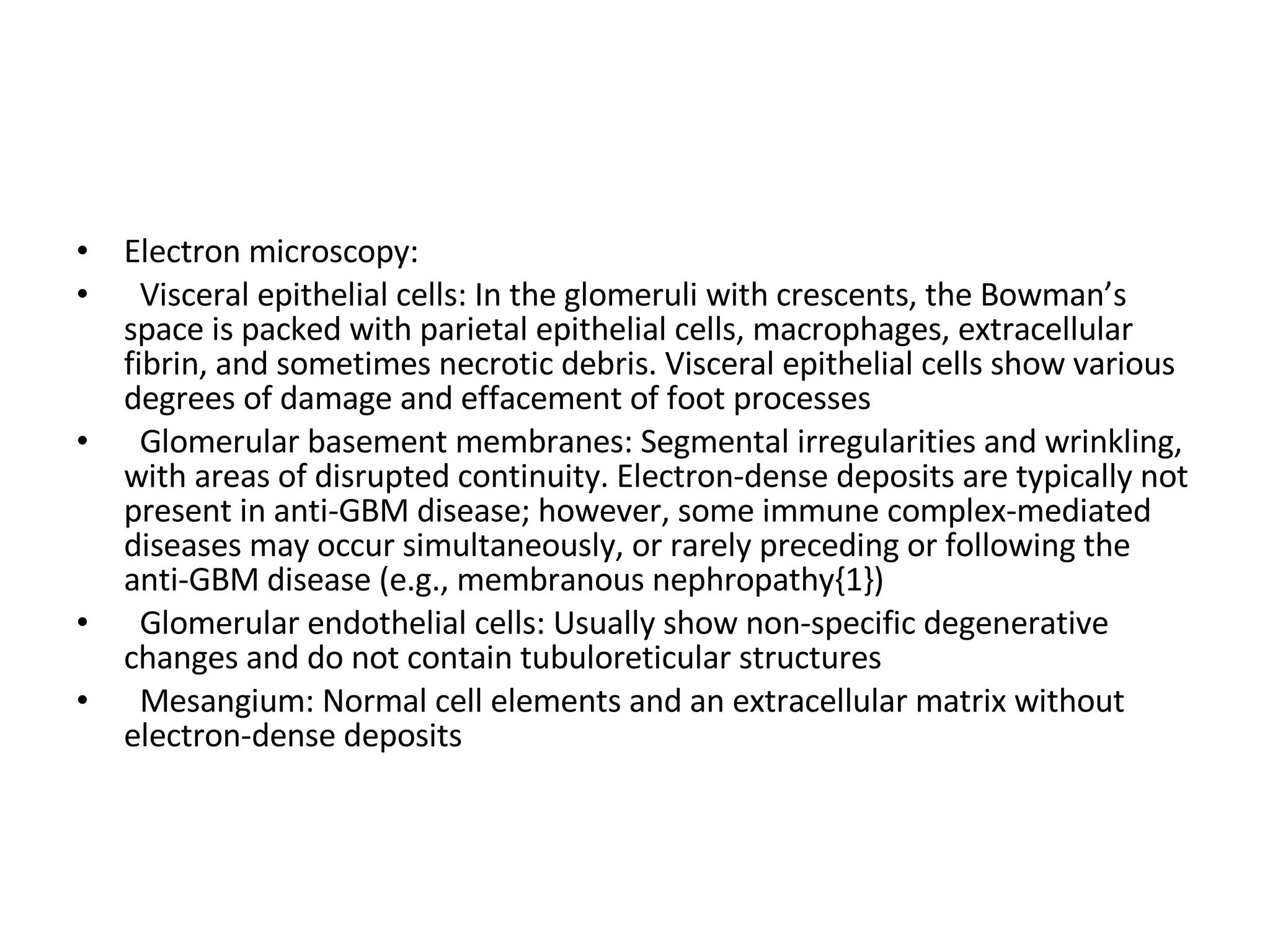
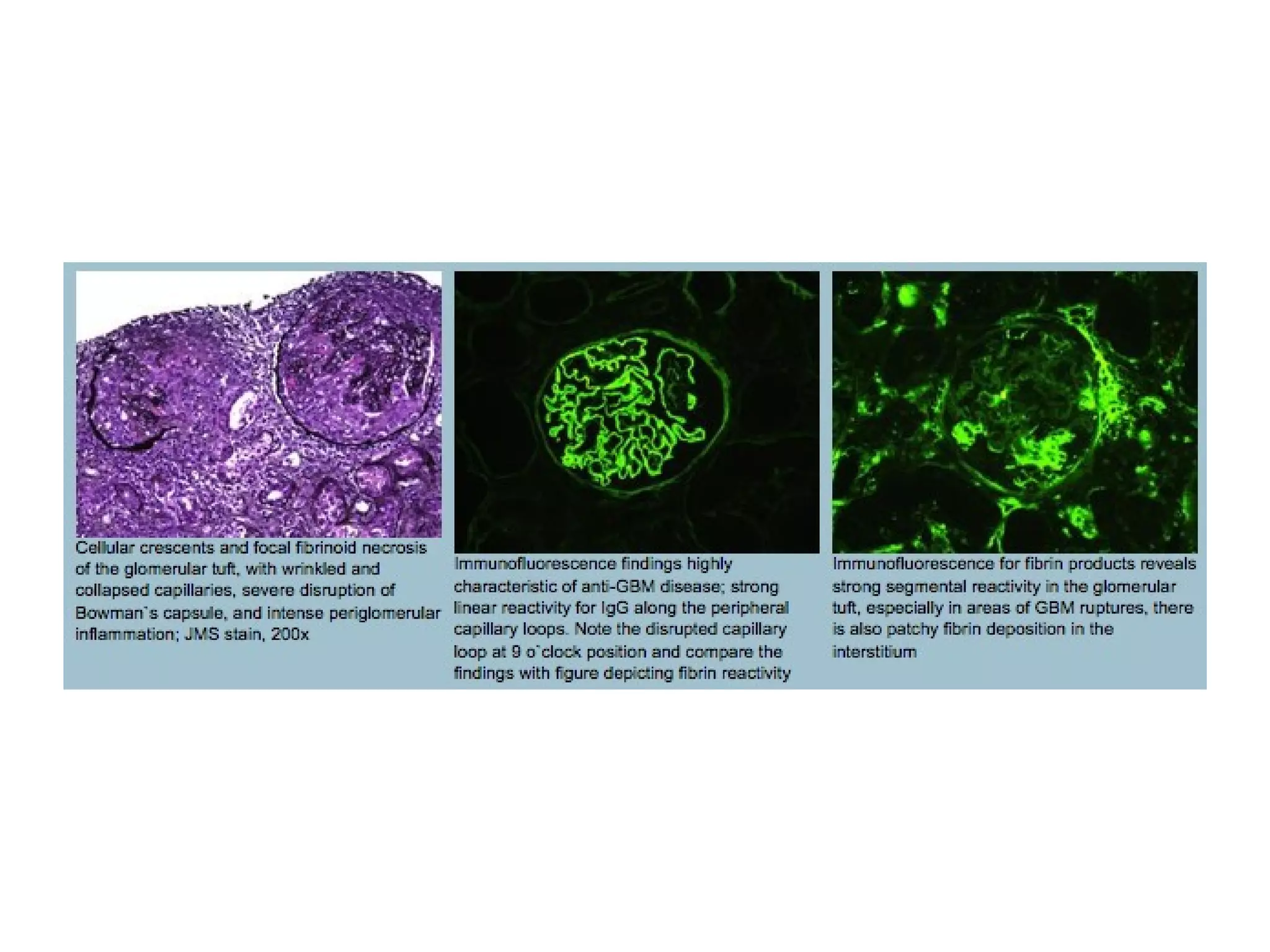
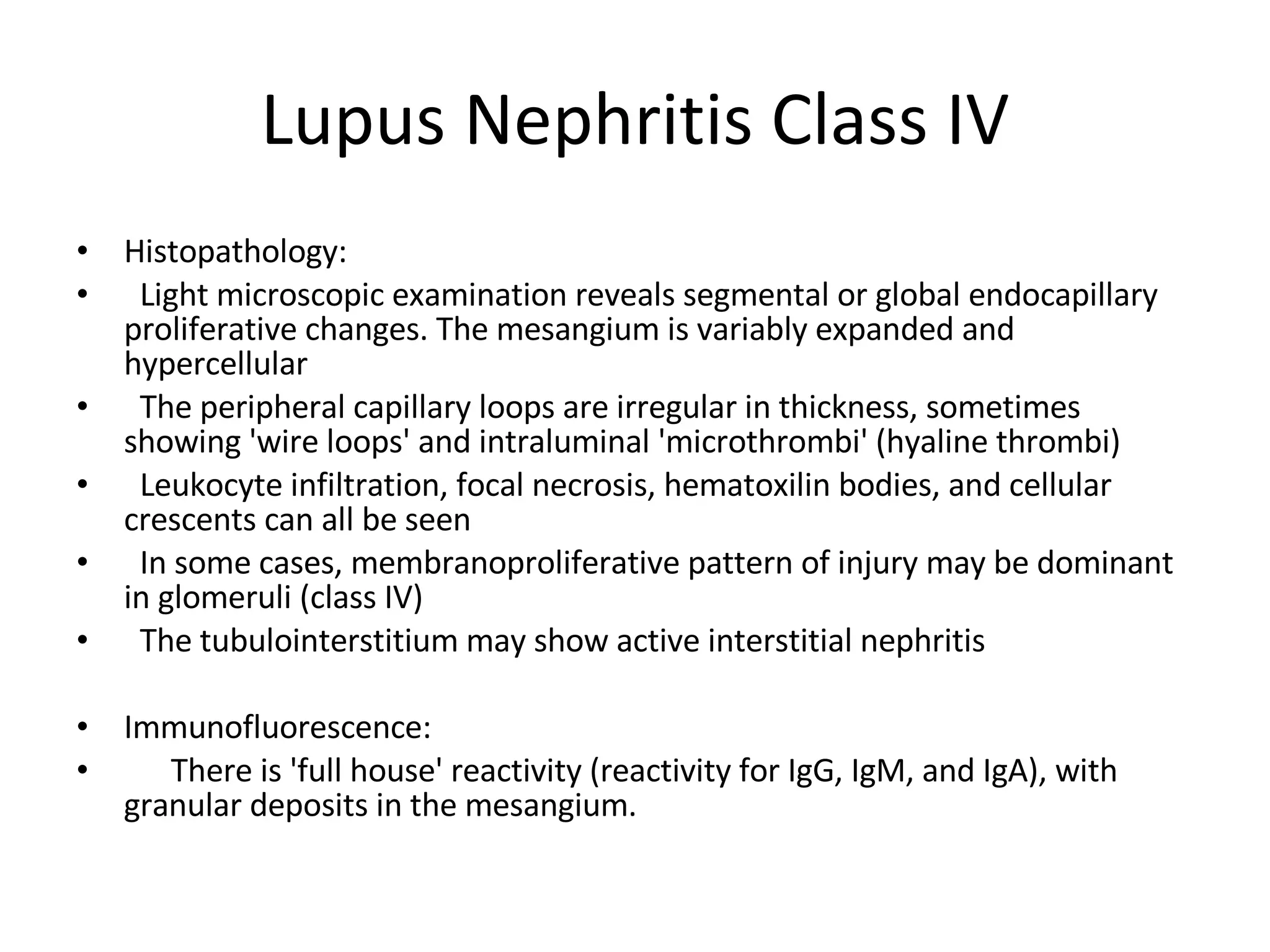
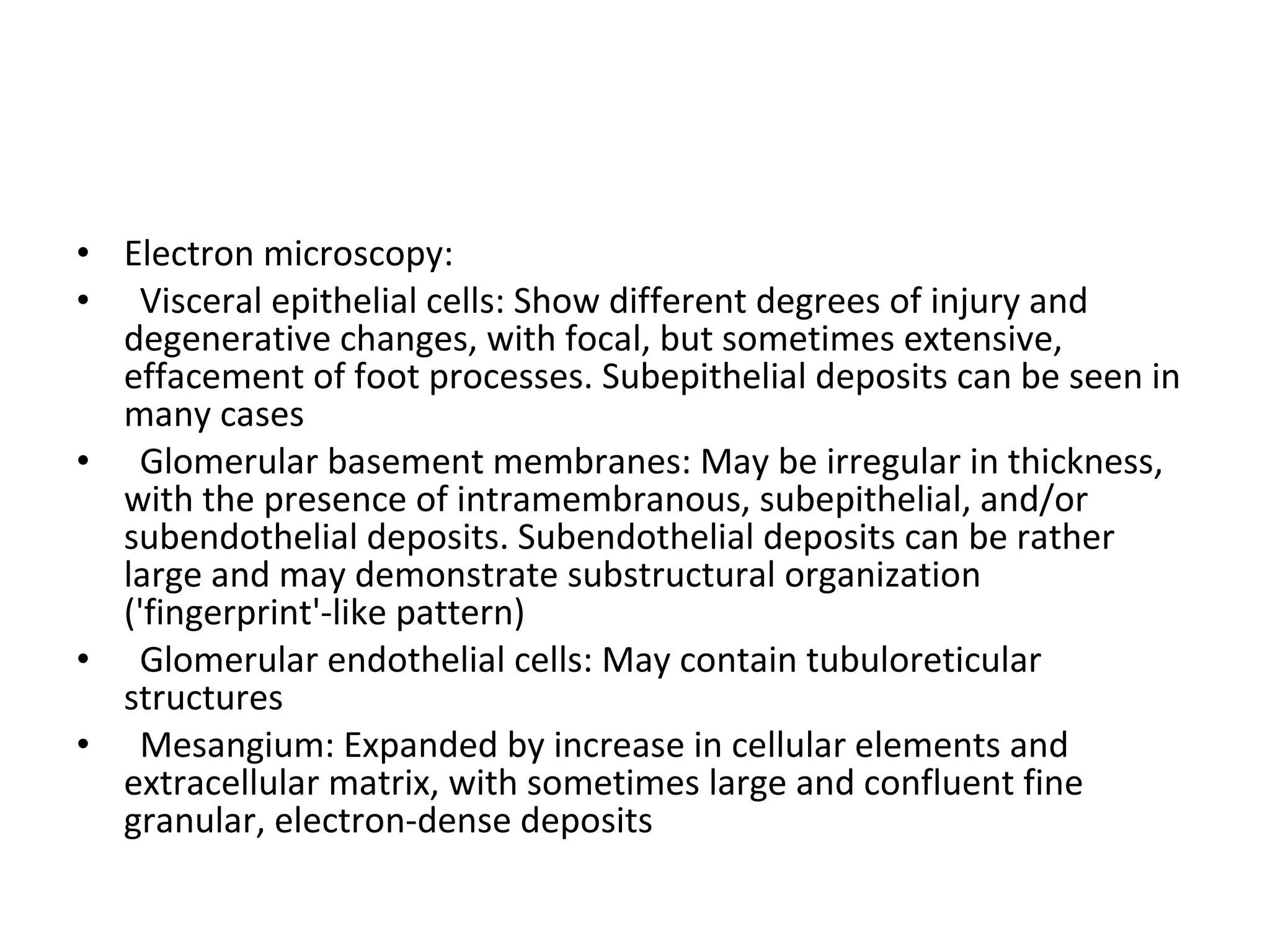
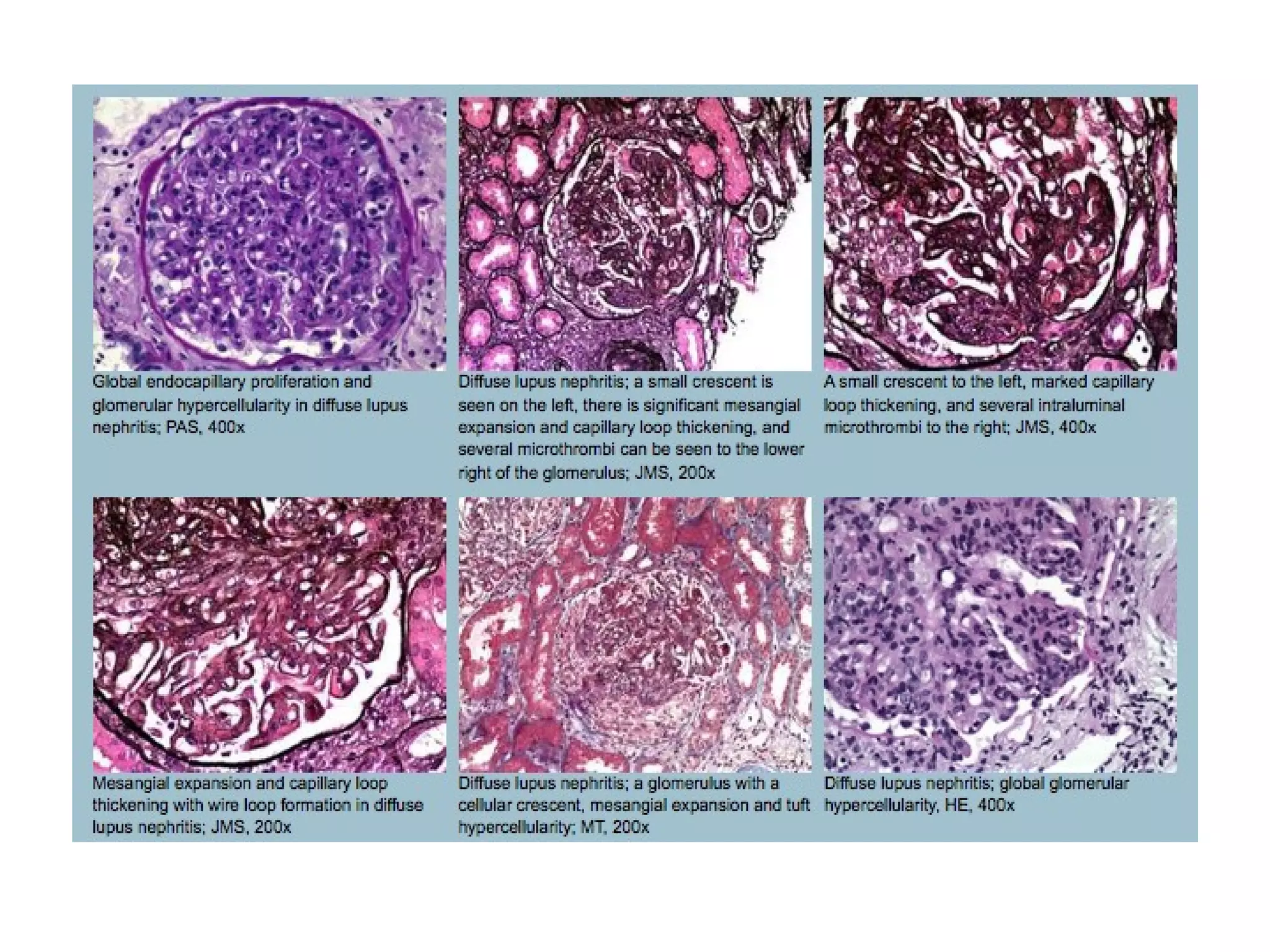
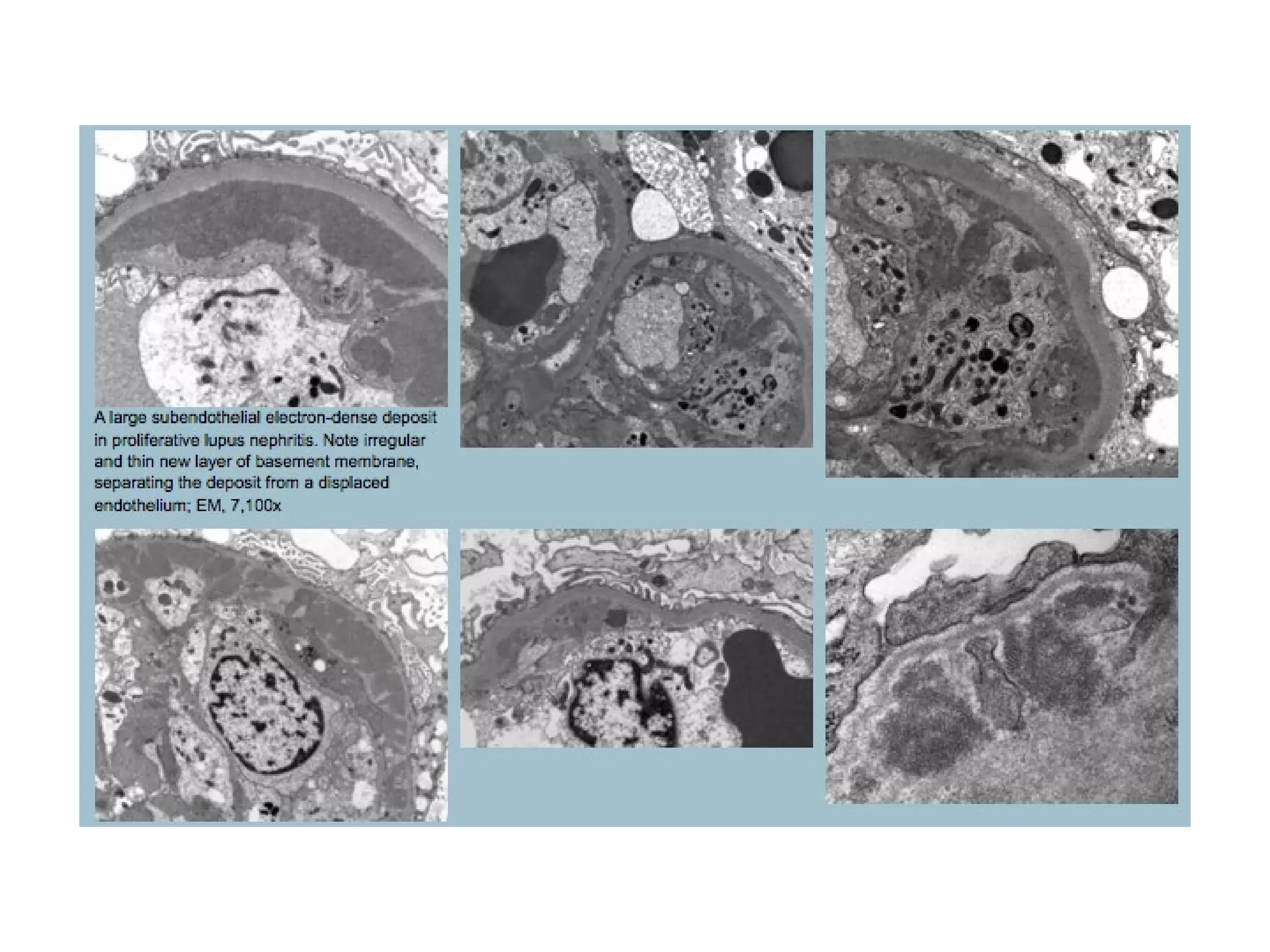
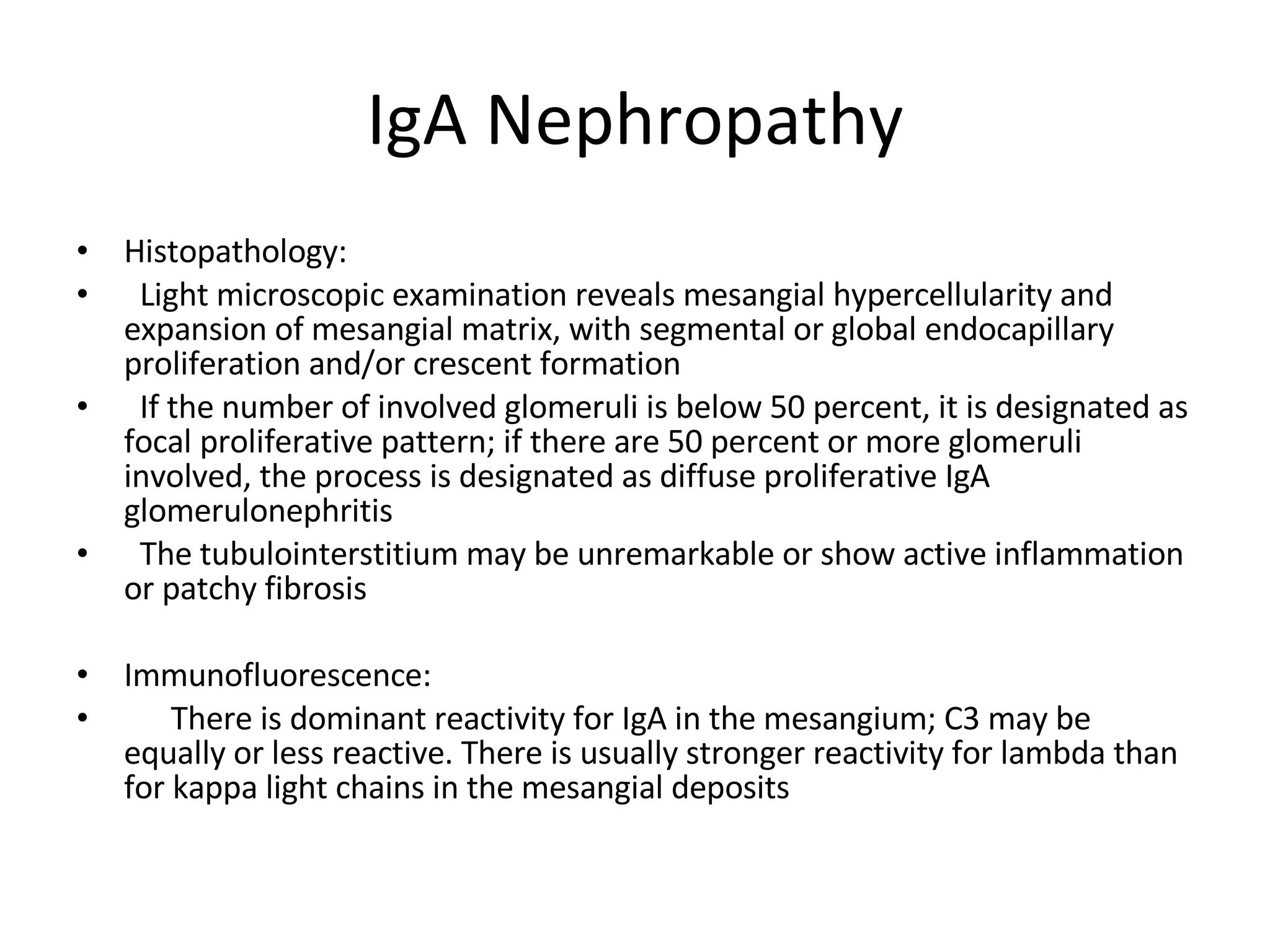
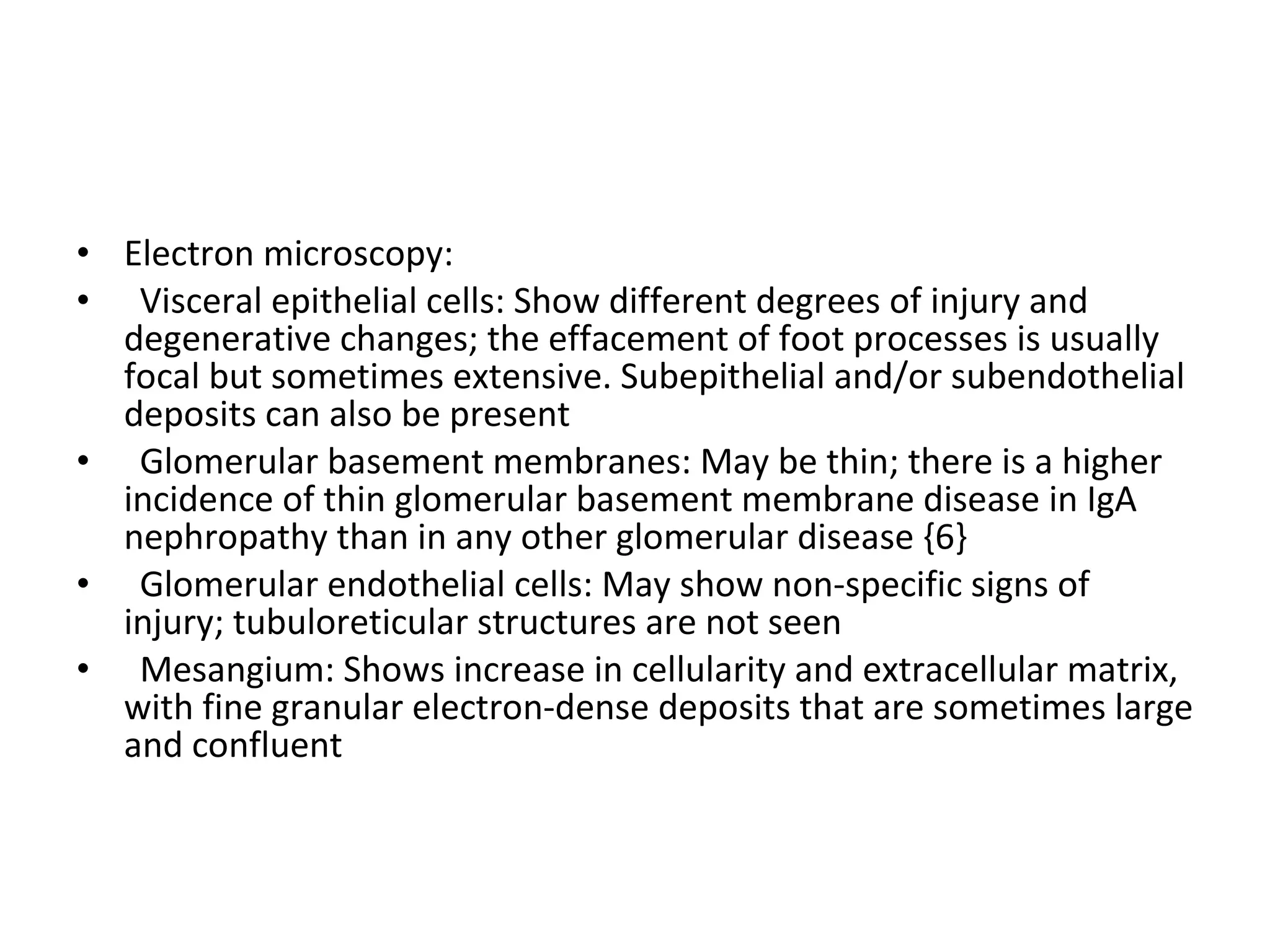
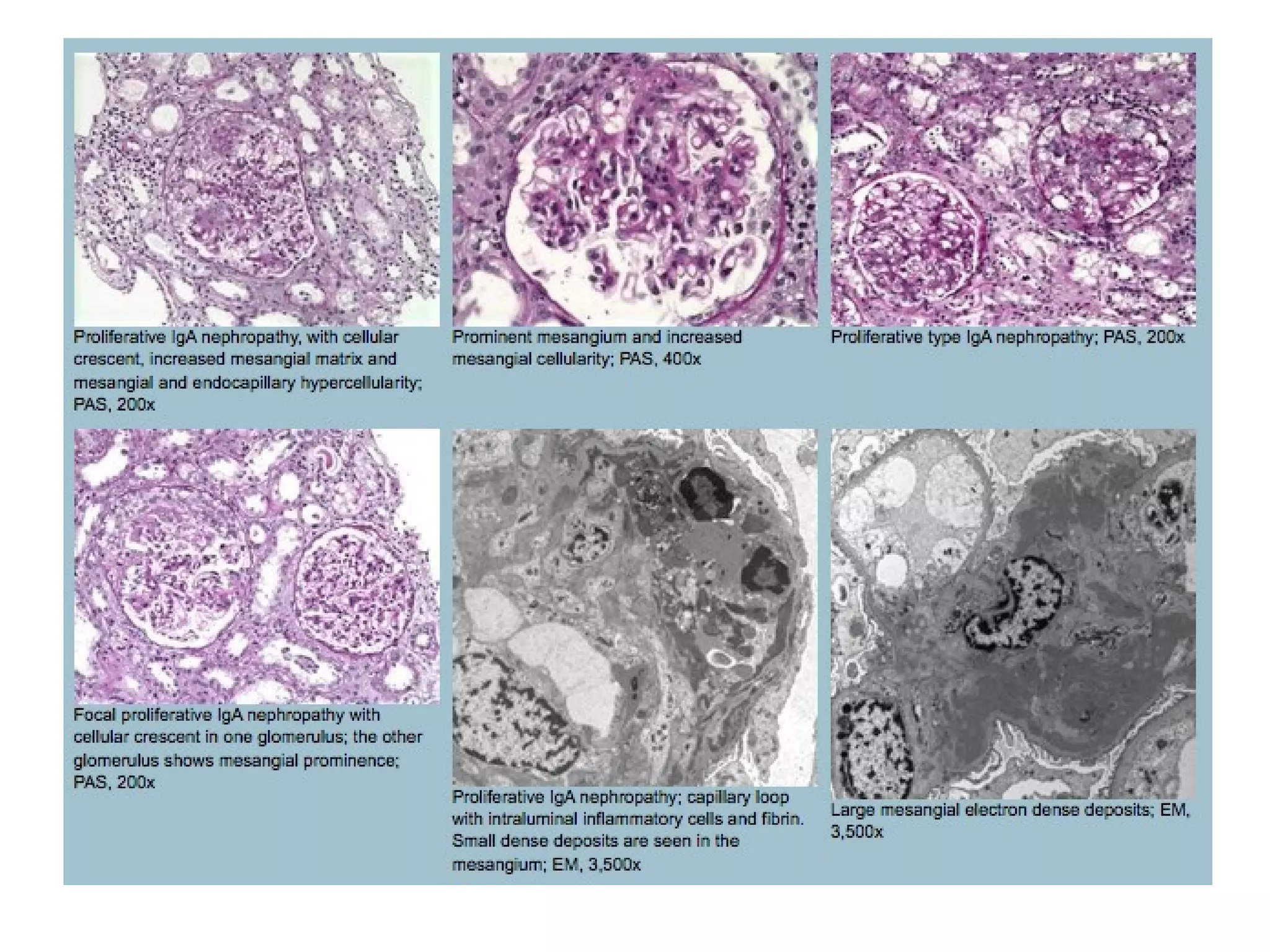
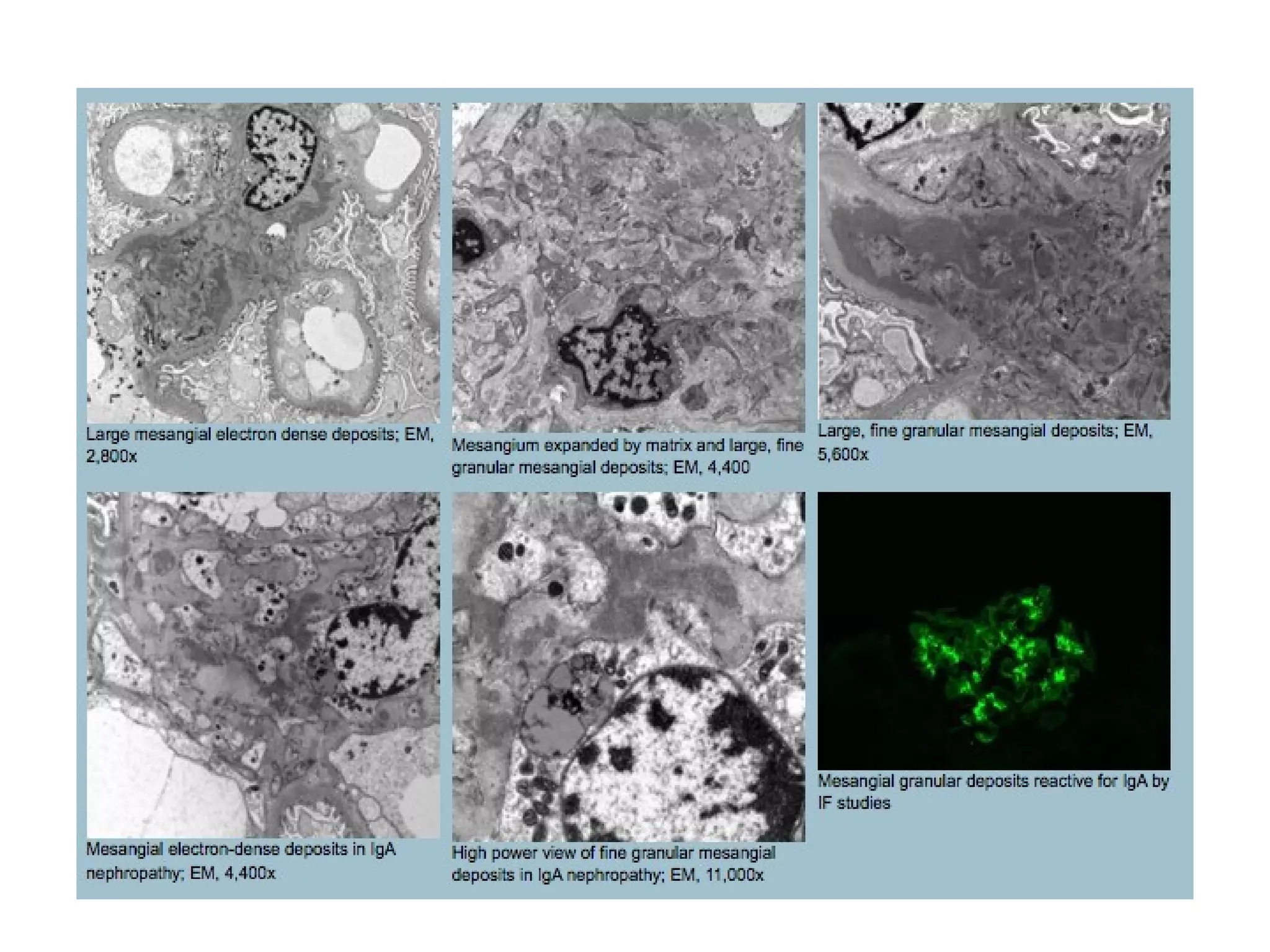
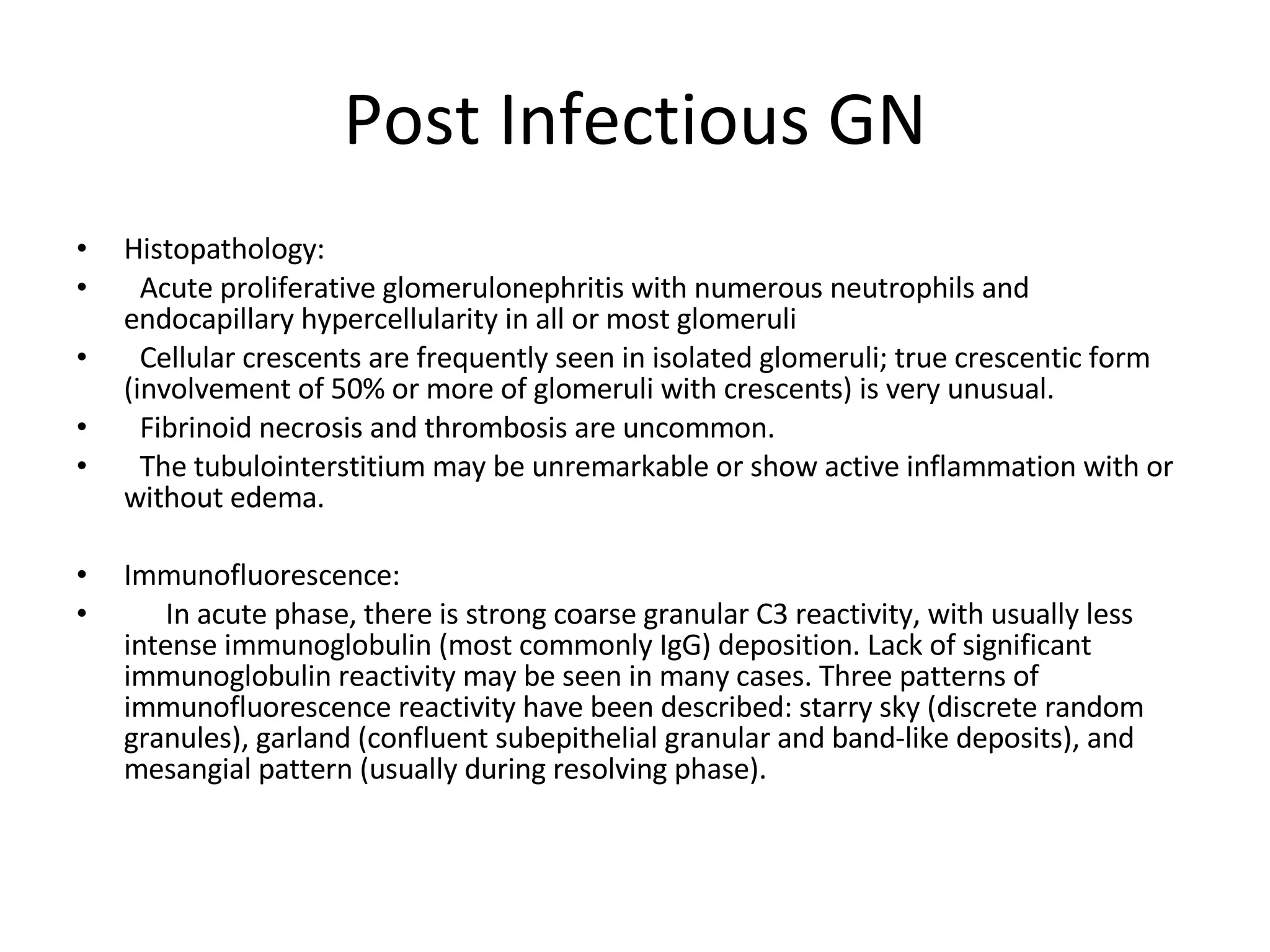
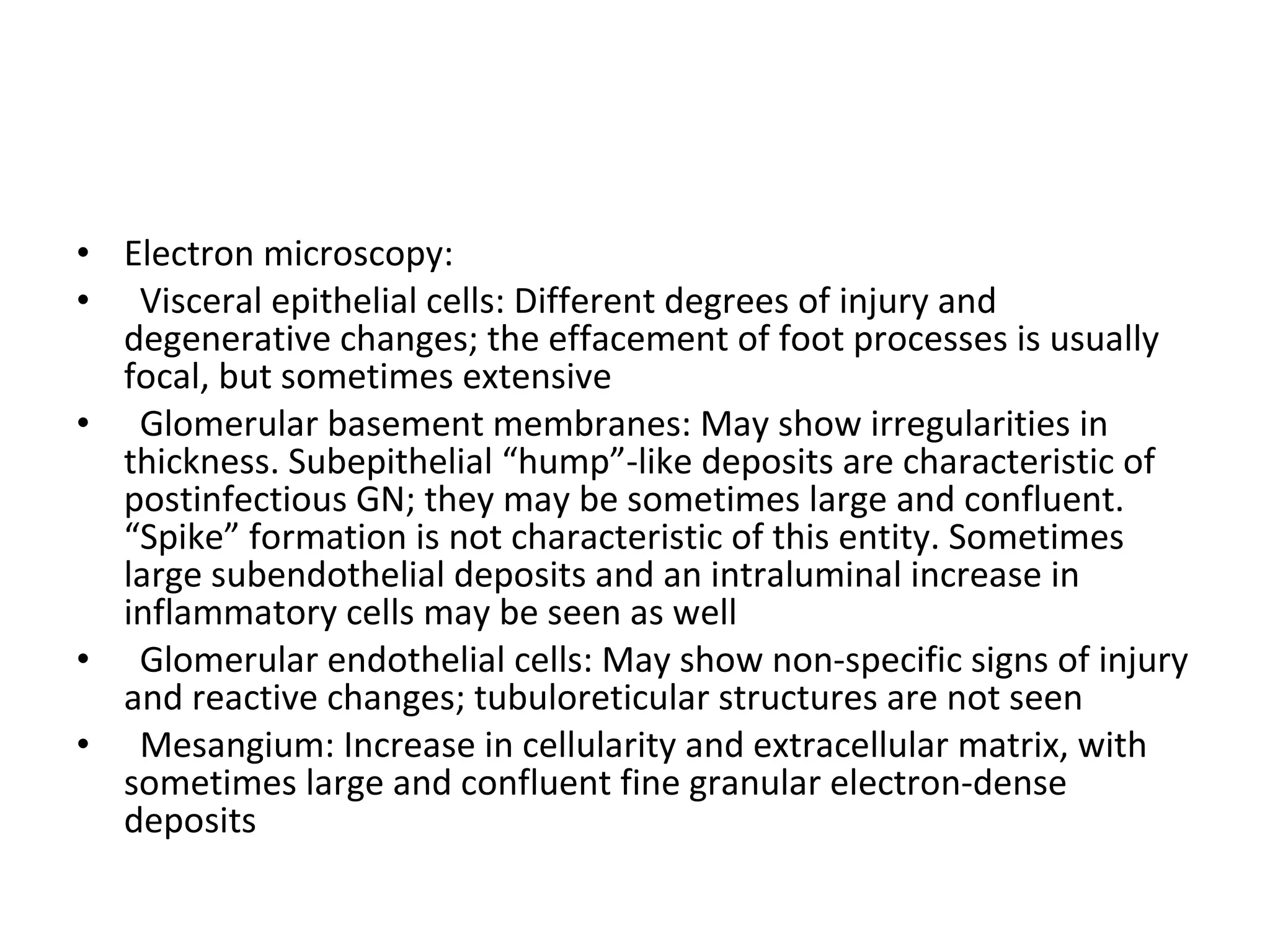
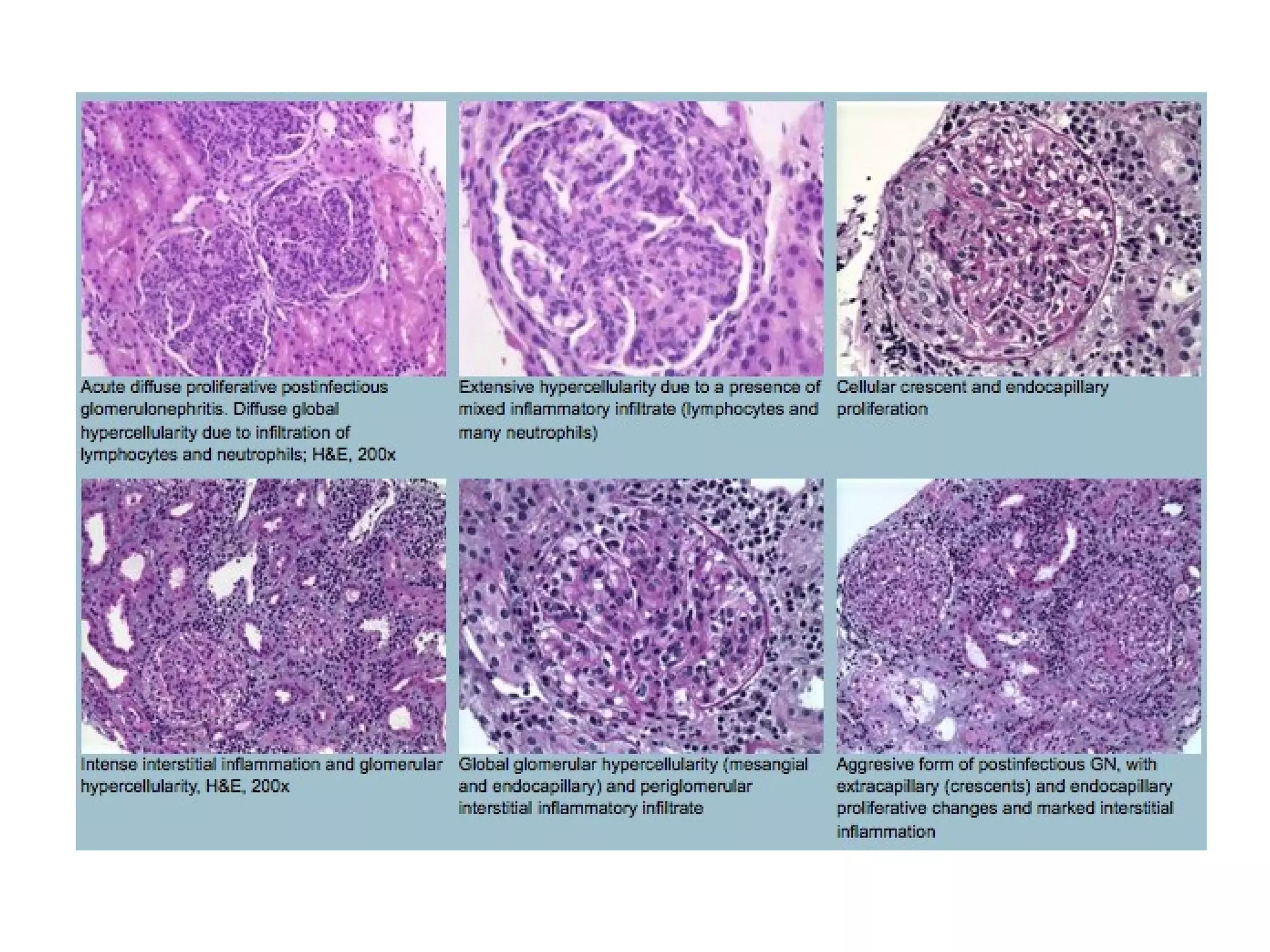
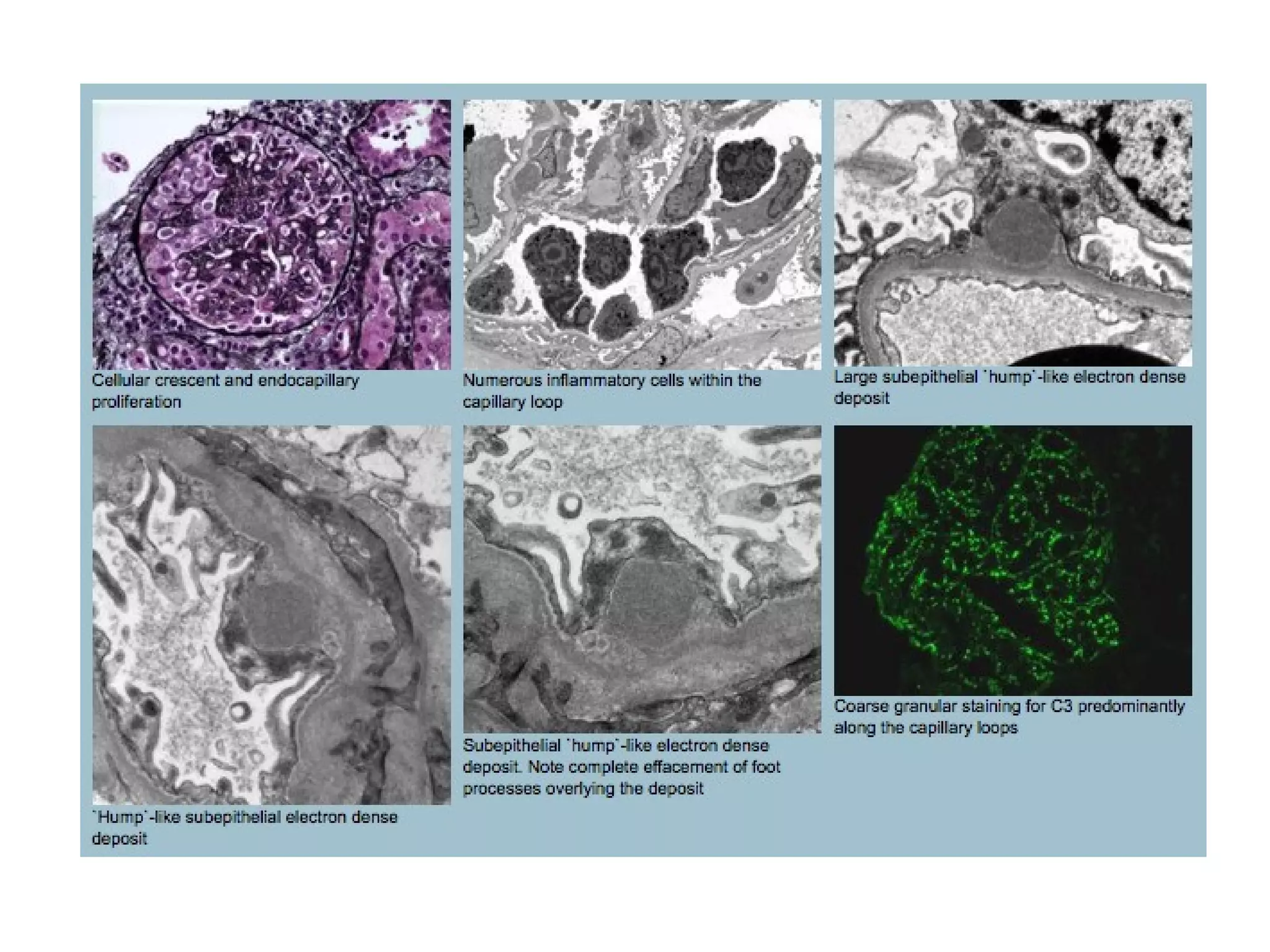
This document discusses the histopathological features of several types of crescentic glomerulonephritis (GN), including anti-glomerular basement membrane (GBM) disease, pauci-immune GN, immune complex-mediated GN, lupus nephritis class IV, IgA nephropathy, and post infectious GN. Key findings include fibrinoid necrosis, crescent formation, immune complex deposition patterns on immunofluorescence, and electron-dense deposits, effacement of foot processes, and basement membrane abnormalities on electron microscopy. The diseases are distinguished by their pathogenic mechanisms and specific immune staining and ultrastructural characteristics.