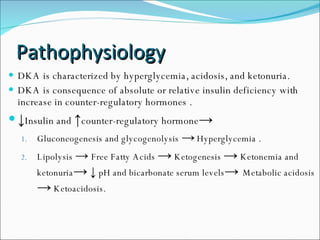
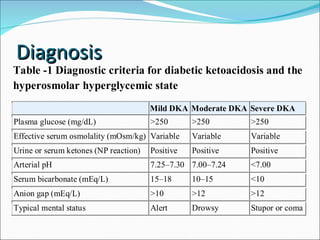
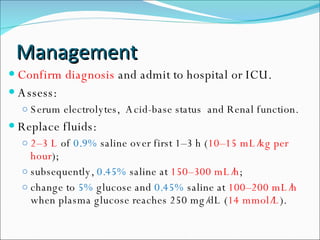
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes caused by low insulin levels and high levels of counter-regulatory hormones. This leads to hyperglycemia, lipolysis, ketogenesis, and metabolic acidosis. Common precipitants include infections, inadequate insulin treatment, and myocardial ischemia. Clinical features include nausea, vomiting, abdominal pain, dehydration, and Kussmaul breathing. Diagnosis involves measuring glucose, ketones, electrolytes, and acid-base status. Management consists of fluid resuscitation, insulin administration, electrolyte replacement, and treating any precipitating causes. Complications can include cerebral edema, cardiac dysrhythmias, and pulmonary edema. Pro