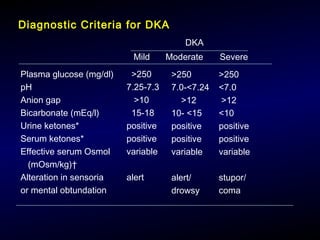
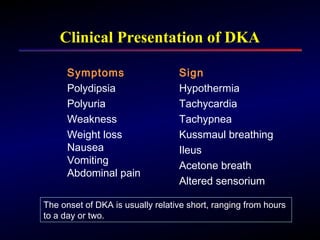
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes caused by relative or absolute insulin deficiency that results in hyperglycemia, ketosis, and acidosis. It occurs most often in patients with type 1 diabetes but can also affect those with type 2 diabetes. Treatment of DKA involves fluid resuscitation, intravenous insulin therapy, electrolyte replacement, and monitoring to correct acidosis and rehydrate the patient. Complications can include hypokalemia, hypoglycemia, cerebral edema, and pulmonary edema. Strict prevention and management of diabetes is important to reduce the risks of DKA.











![Serum Sodium
Hyponatremia is common in patients with DKA
H2O
H2O
H2O
Serum glucose
Na+
H2O
Correction of Serum sodium:
Corrected Na+
= [Na+
] 1.6 x glucose (mg/dl) – 100
100](https://image.slidesharecdn.com/dka-pathphysiologymanagement2014-copy-140202235658-phpapp02-140524123236-phpapp01/85/Dka-pathphysiologymanagement2014-copy-140202235658-phpapp02-15-320.jpg)

![Anion Gap Formula
• Anion gap can be measured as
• AG=[(Na)-(Hco3+CL)]](https://image.slidesharecdn.com/dka-pathphysiologymanagement2014-copy-140202235658-phpapp02-140524123236-phpapp01/85/Dka-pathphysiologymanagement2014-copy-140202235658-phpapp02-17-320.jpg)