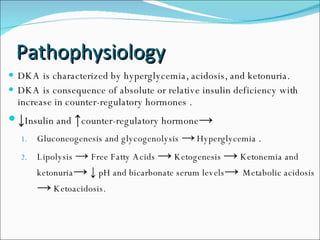
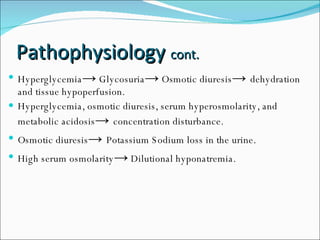
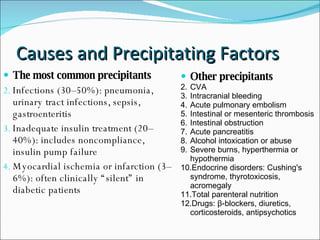
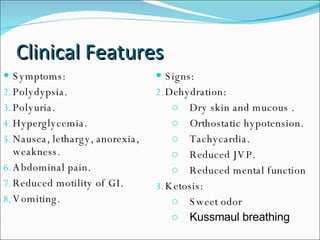
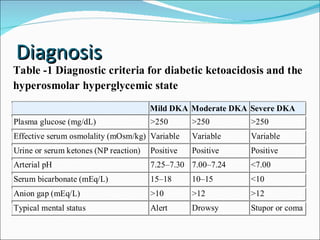
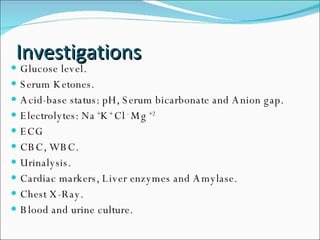
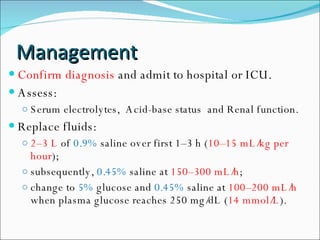
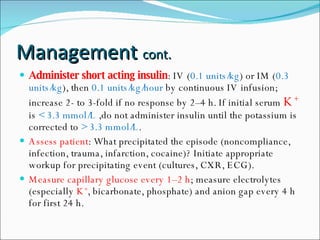
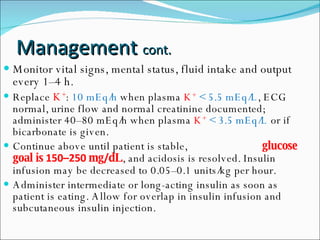
The document discusses diabetic ketoacidosis (DKA), providing definitions, pathophysiology, causes, clinical features, investigations, management, complications, and prognosis. DKA is an acute, life-threatening complication of diabetes characterized by hyperglycemia, acidosis, and ketonuria due to insulin deficiency and increased counter-regulatory hormones. Common causes include infections, inadequate insulin treatment, and medical issues like myocardial infarction. Management involves fluid resuscitation, insulin administration, electrolyte replacement, and treating any precipitating conditions. Complications can include cerebral edema, cardiac dysrhythmias, and pulmonary edema. Prognosis is generally excellent with treatment but worse for older patients with severe illnesses.