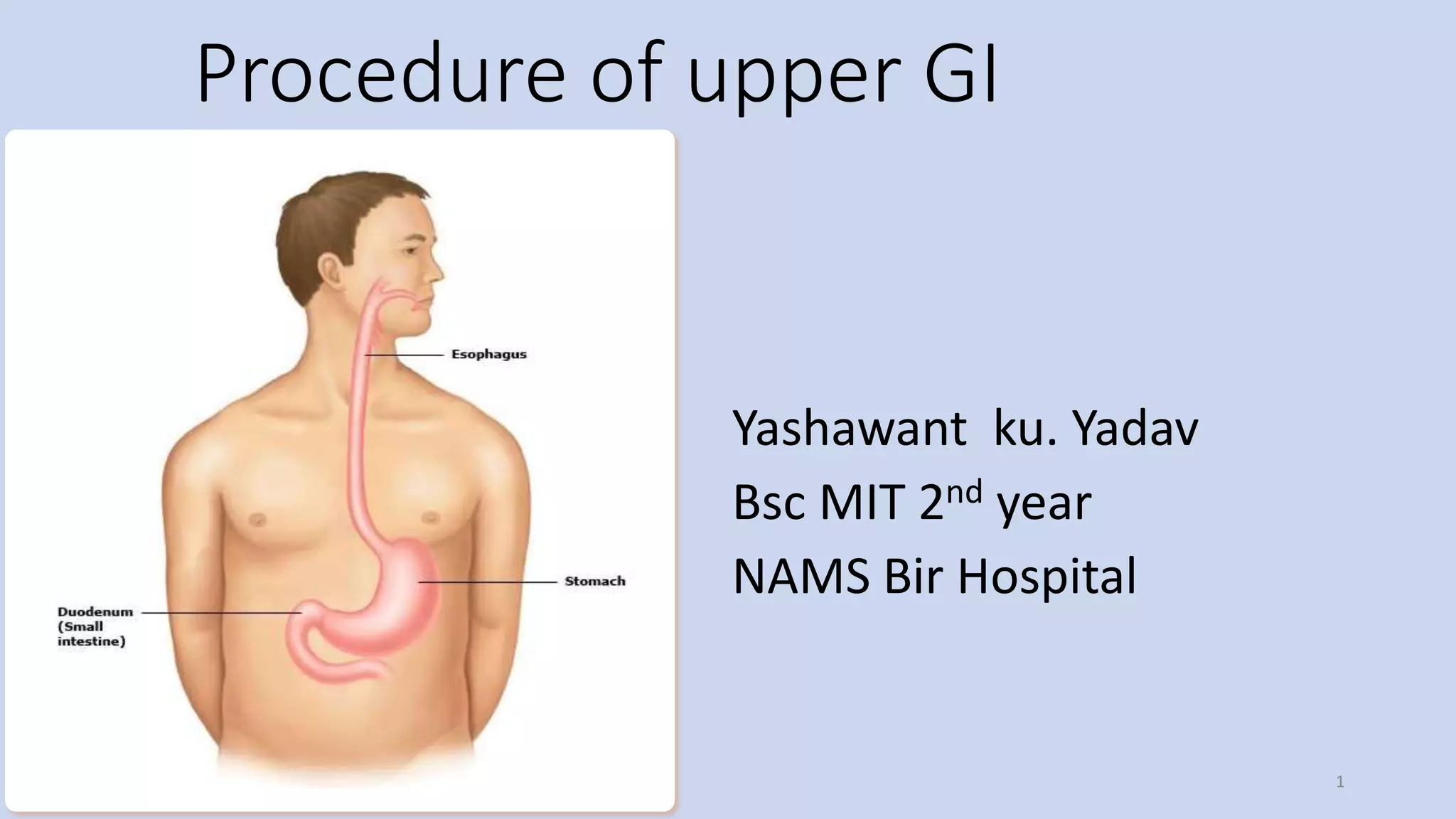
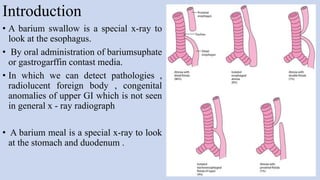
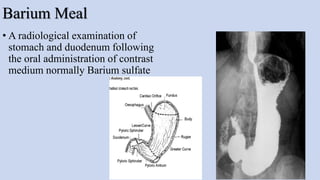
1. The document describes the procedure for an upper GI exam, including barium swallow and barium meal.
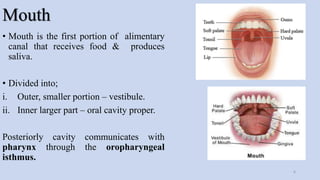
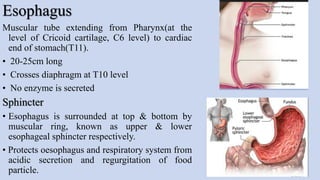
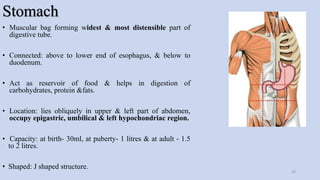
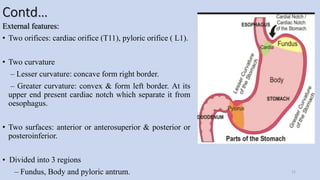
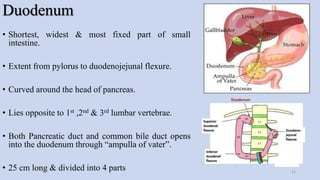
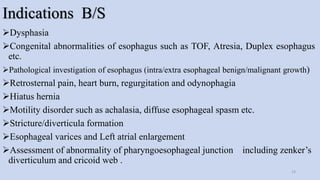
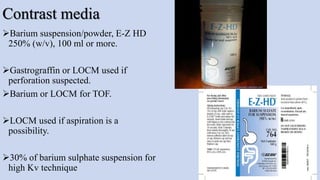
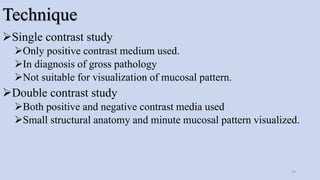
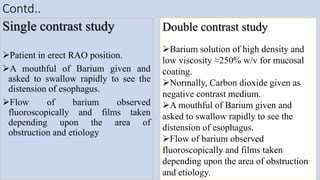
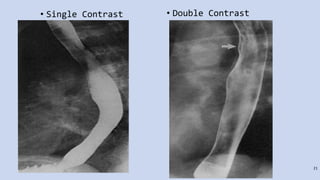
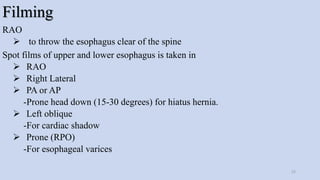
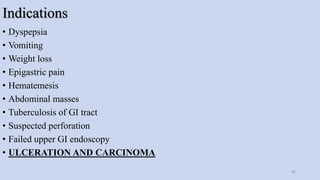
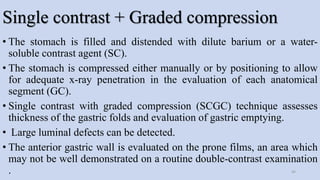
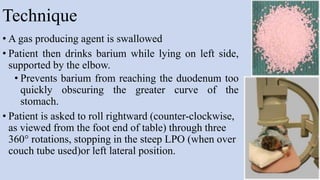
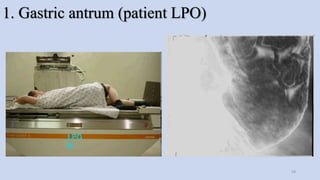
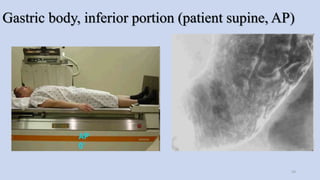
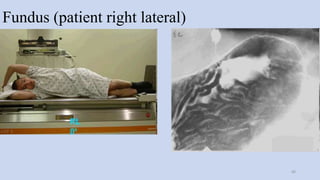
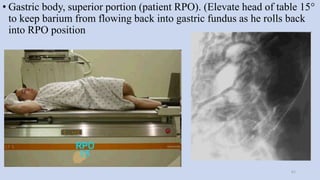
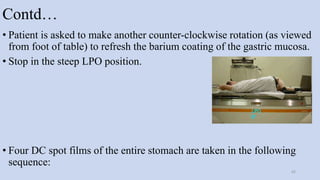
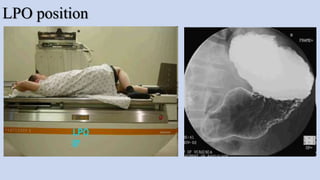
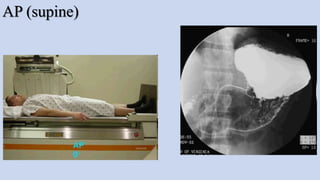
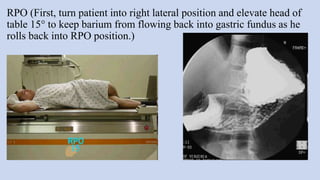
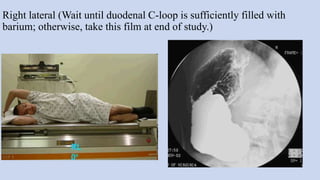
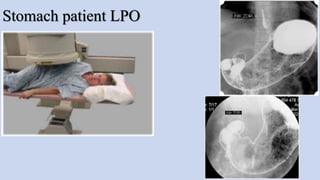
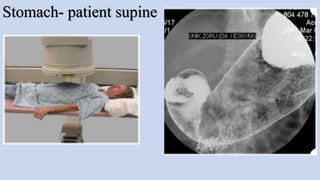
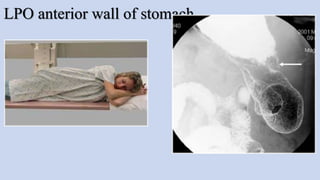
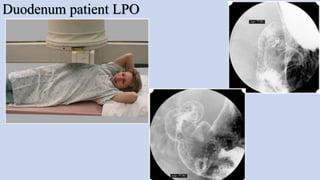
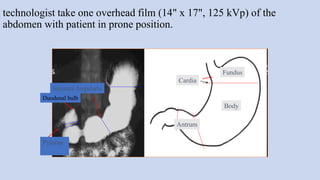
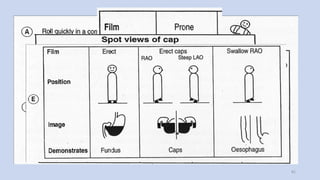
2. It details the anatomy of the upper GI tract, indications, contraindications, equipment, and techniques for barium swallow and barium meal exams.
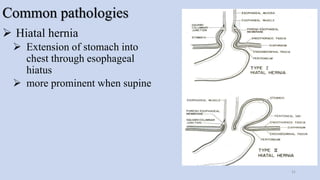
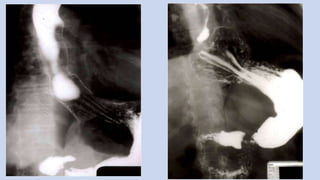
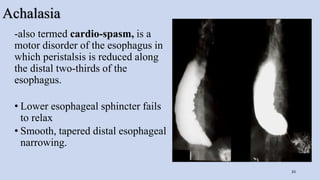
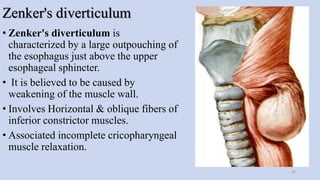
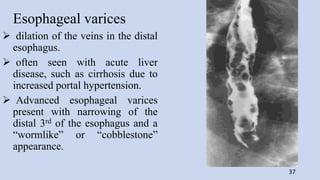
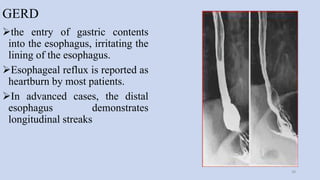
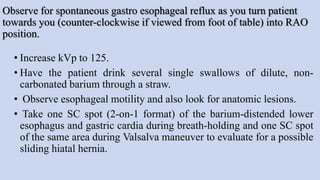
3. Common pathologies that can be detected include hiatal hernia, achalasia, Zenker's diverticulum, esophageal varices, and GERD.