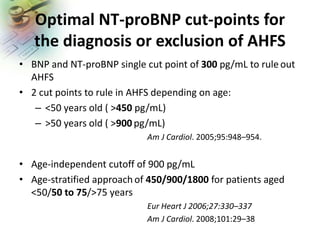
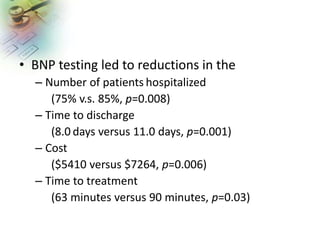
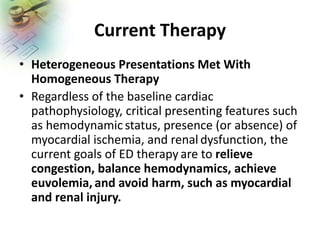
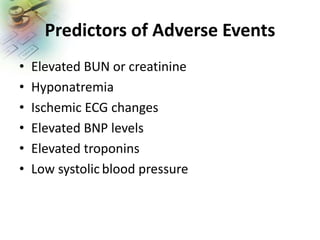
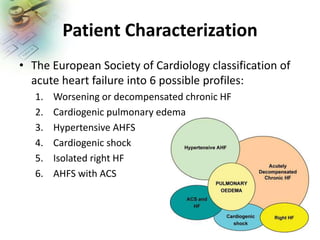
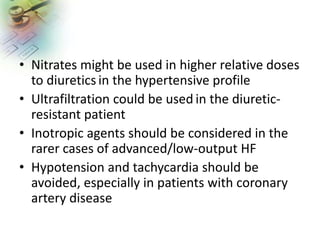
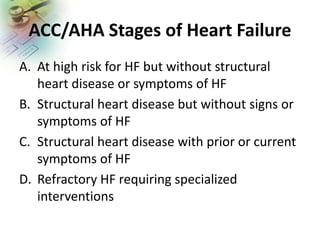
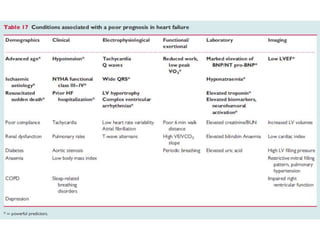
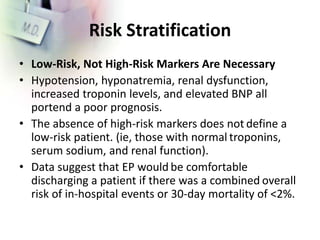
The document discusses current practices in the emergency department (ED) for diagnosing and treating acute heart failure syndromes (AHFS), highlighting the importance of rapid evaluation and appropriate interventions. Key diagnostic tools include BNP and NT-proBNP testing to assess AHFS severity and guide treatment decisions, while recommendations for therapy focus on fluid management and stabilizing hemodynamics. Additionally, it outlines risk stratification and prognostic indicators for patients with AHFS, emphasizing the need for early intervention and patient education to reduce readmissions.