This document summarizes deep vein thrombosis (DVT) prophylaxis for orthopedic surgeries. It discusses that without prophylaxis, the risk of DVT is 50% for orthopedic surgeries and the risk of fatal pulmonary embolism is 2.0-2.5% for hip replacement and 2.5-7.5% for fractured hip. It reviews various risk assessment models and prophylaxis methods, including mechanical methods like compression stockings and intermittent pneumatic compression, and pharmacological methods like low molecular weight heparins, warfarin, and newer oral anticoagulants. It provides comparisons of effectiveness and safety between different prophylaxis options. National guidelines for











![Interpretation
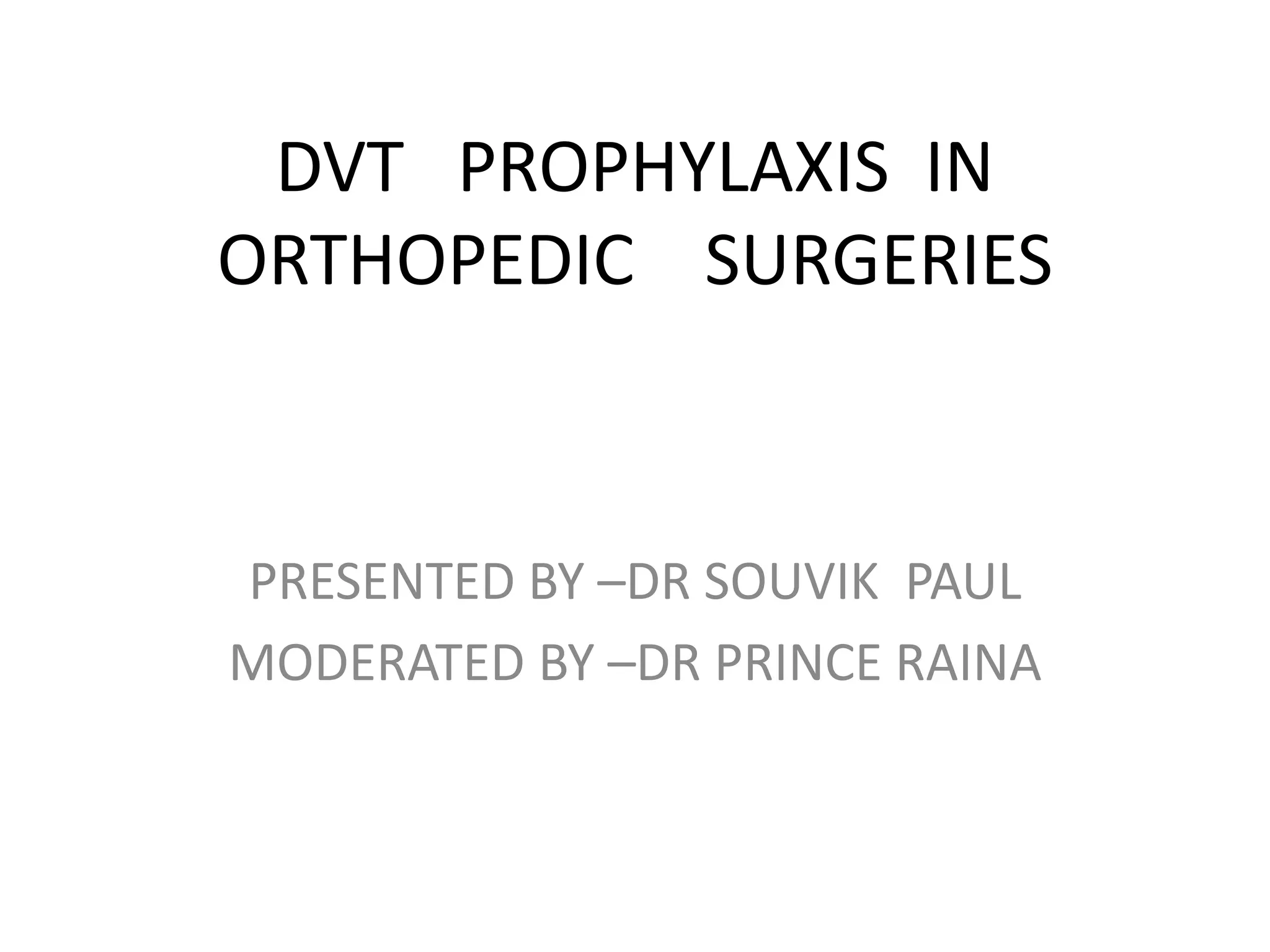
High probability: ≥ 3 (Prevalence of DVT - 53%)
Moderate probability: 1-2 (Prevalence of DVT - 17%)
Low probability: ≤ 0 (Prevalence of DVT - 5%)
Adapted from Anand SS, et al. JAMA. 1998; 279 [14];1094](https://image.slidesharecdn.com/mypresentation-161218165918/75/DVT-PROPHYLAXIS-IN-ORTHOPEDIC-SURGERIES-15-2048.jpg)












![Update of
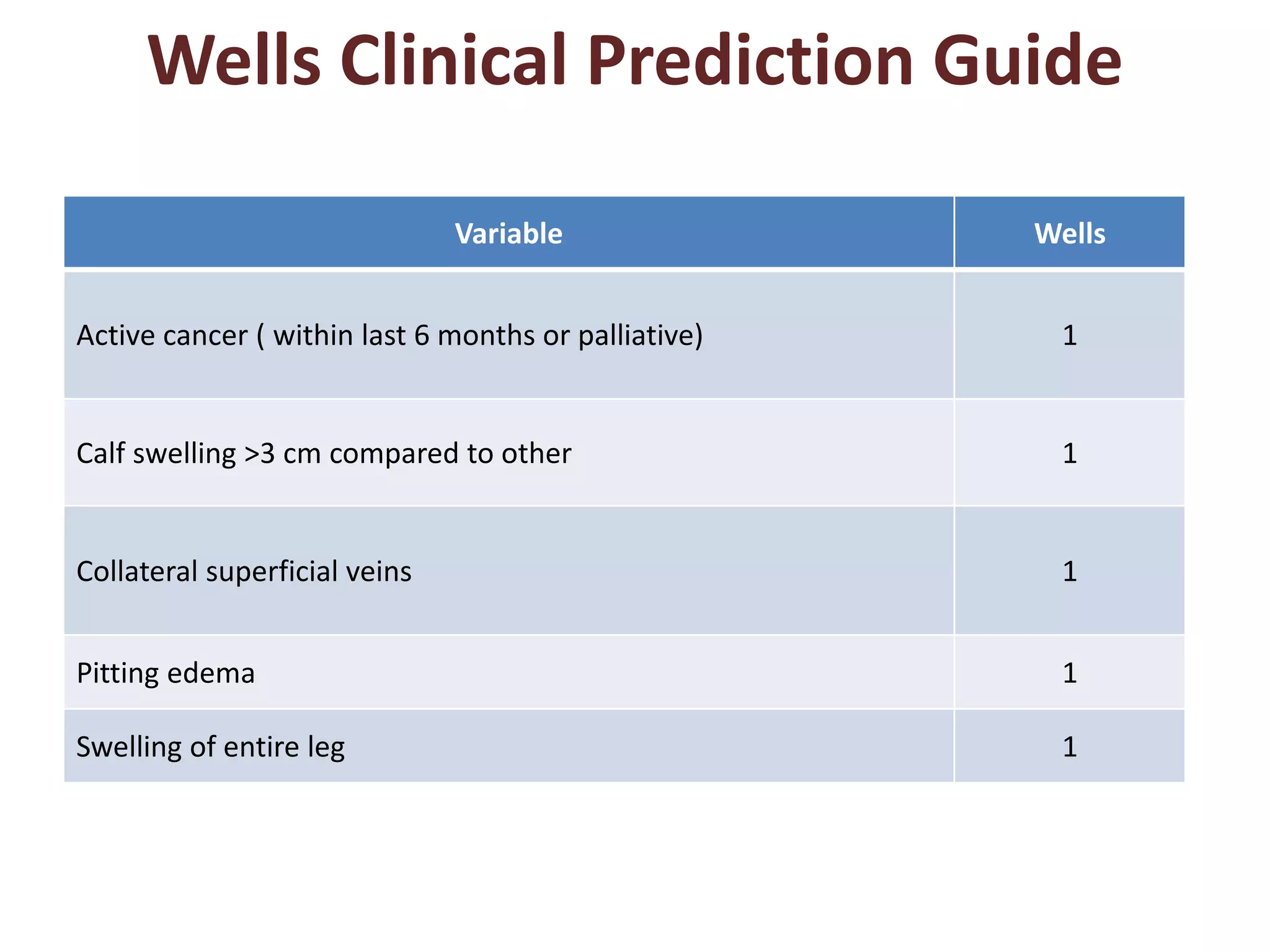
Elastic compression stockings for prevention of deep vein
thrombosis. [Cochrane Database Syst Rev. 2010]
19 RCTs
1681 individual patients and 1064 individual legs (2745 analytic units).
9 TRIALS- general surgery,
6 TRIALS- orthopaedic surgery,
1 TRIAL- medical patients.
G c s applied on the day before surgery or on the day of surgery . worn up
until discharge or until the patients were fully mobile](https://image.slidesharecdn.com/mypresentation-161218165918/75/DVT-PROPHYLAXIS-IN-ORTHOPEDIC-SURGERIES-29-2048.jpg)

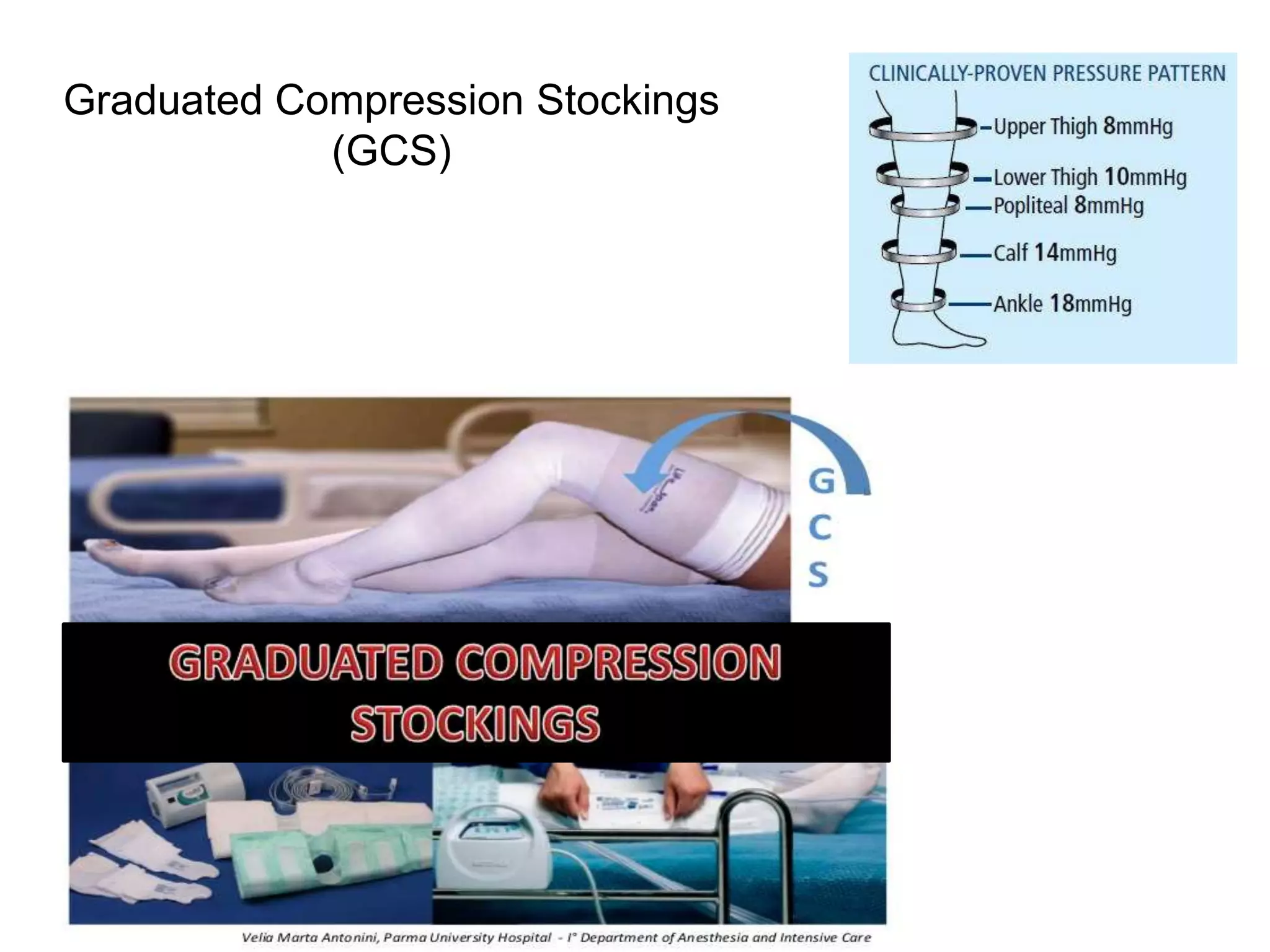
![INTERMITTENT PNEUMATIC
COMPRESSION [IPC]
• Inflation Cycle :10-20 secs
• Deflation cycle :30 secs](https://image.slidesharecdn.com/mypresentation-161218165918/75/DVT-PROPHYLAXIS-IN-ORTHOPEDIC-SURGERIES-31-2048.jpg)



![A: Venous blood flow velocity in the posterior tibial vein during compression by a foot cuff (velocity/ time
B: Venous blood flow velocity in the femoral vein during compression by a foot cuff (velocity [cm/s] vs. time [1
second per vertical dotted line]).](https://image.slidesharecdn.com/mypresentation-161218165918/75/DVT-PROPHYLAXIS-IN-ORTHOPEDIC-SURGERIES-35-2048.jpg)