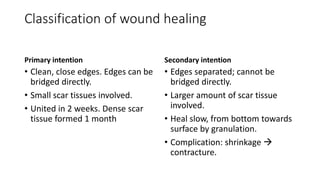
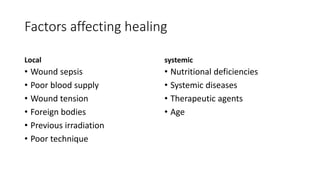
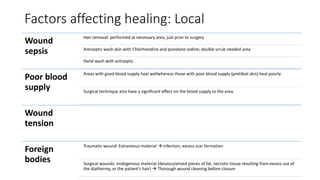
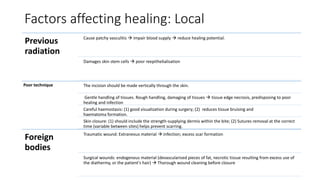
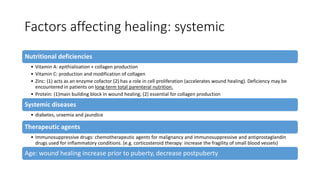
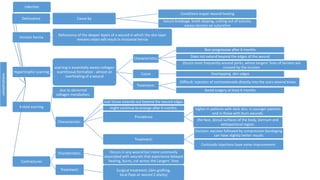
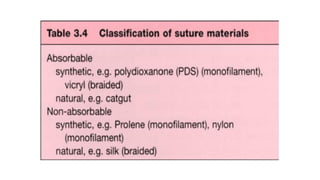
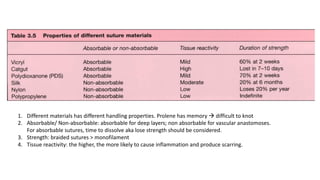
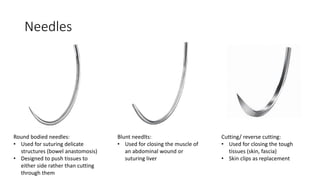
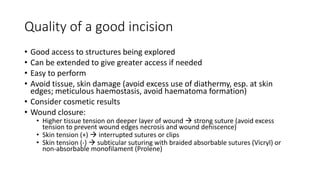
This document discusses wound healing and suture materials. It covers the classification and normal sequence of wound healing, factors that affect healing, potential complications, and different types of suture materials and needles. Wound healing involves hemostasis, inflammation, proliferation, and maturation phases. Factors like infection, blood supply, wound tension, and patient health can influence healing. Complications include infection, dehiscence, scarring, and contractures. A variety of suture materials exist with different properties, and the appropriate material depends on factors like strength needed and tissue reactivity. Needle shape also matters based on the tissue being sutured.