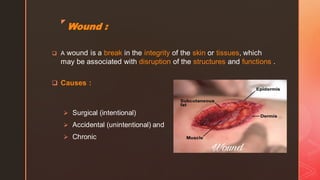
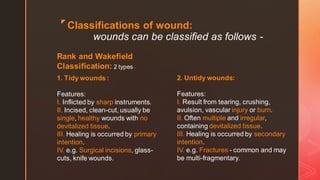
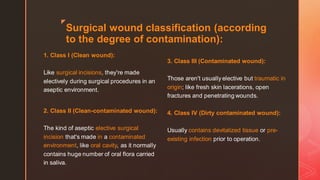
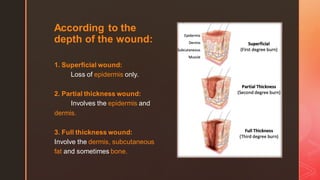
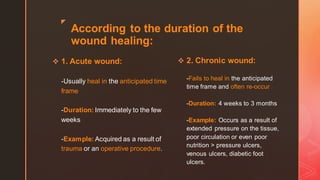
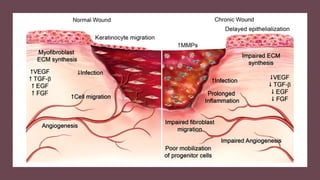
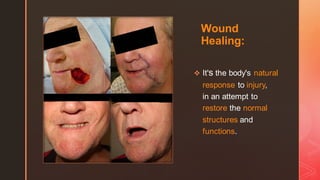
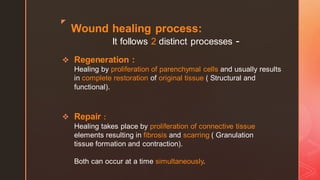
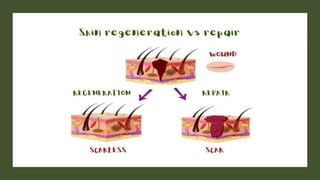
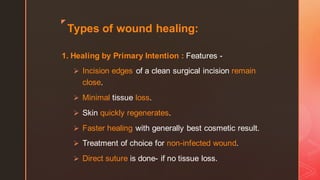
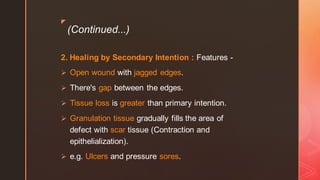
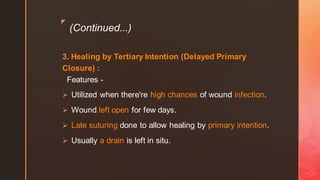
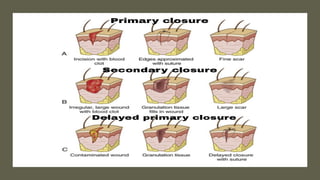
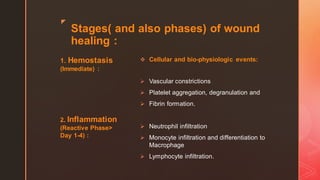
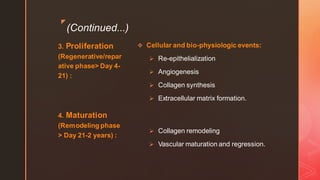
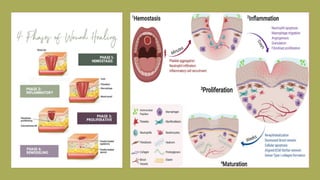
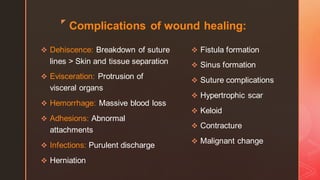
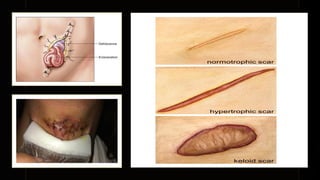
This document discusses wound healing, defining wounds and classifying them. It covers the definition and process of wound healing, involving hemostasis, inflammation, proliferation, and maturation phases. Factors that influence and delay wound healing are addressed. Management of wounds involves cleaning, debridement if needed, approximating edges, dressing, and antibiotics if infected. The goal of wound healing treatment is satisfactory repair.