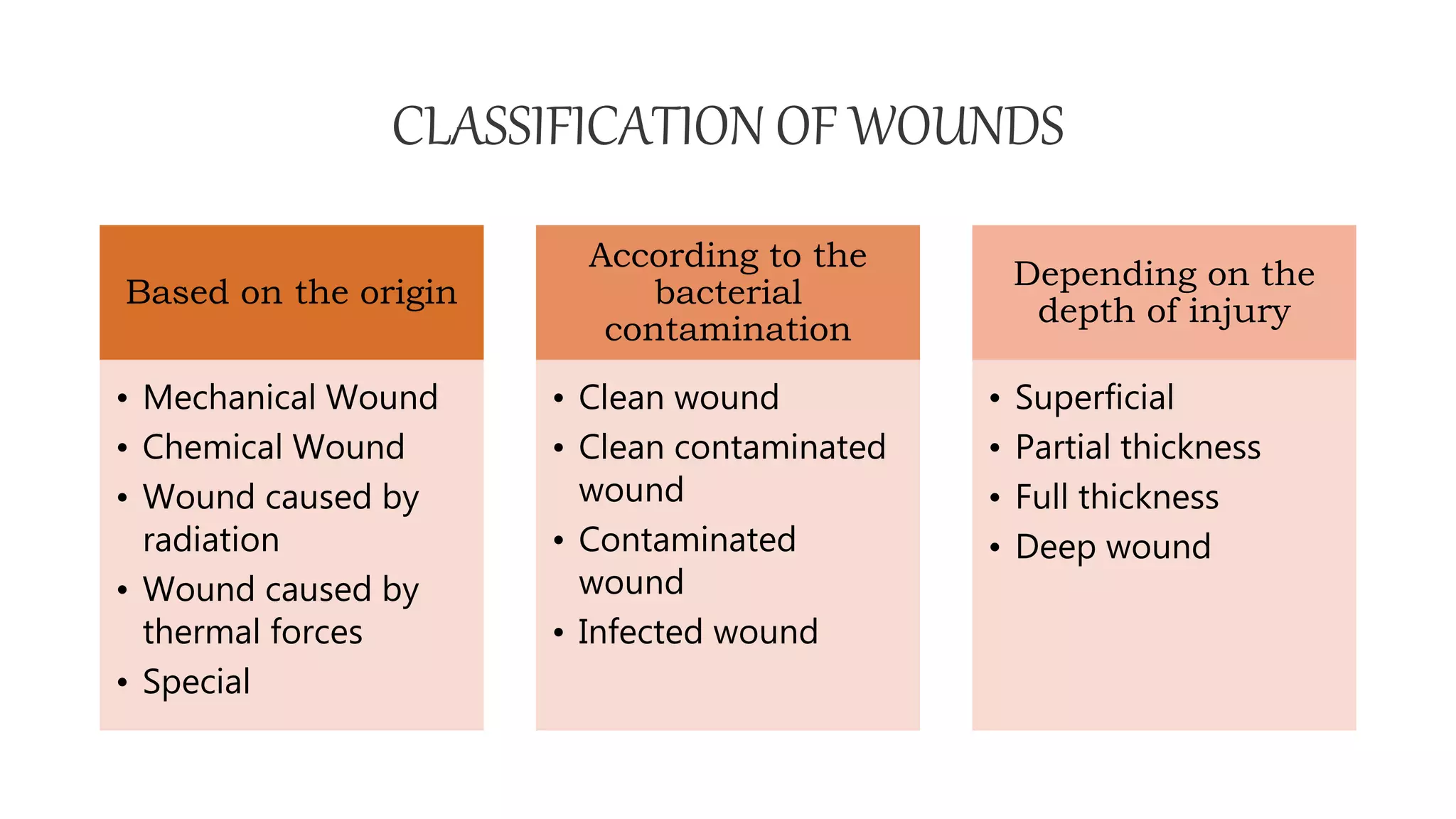
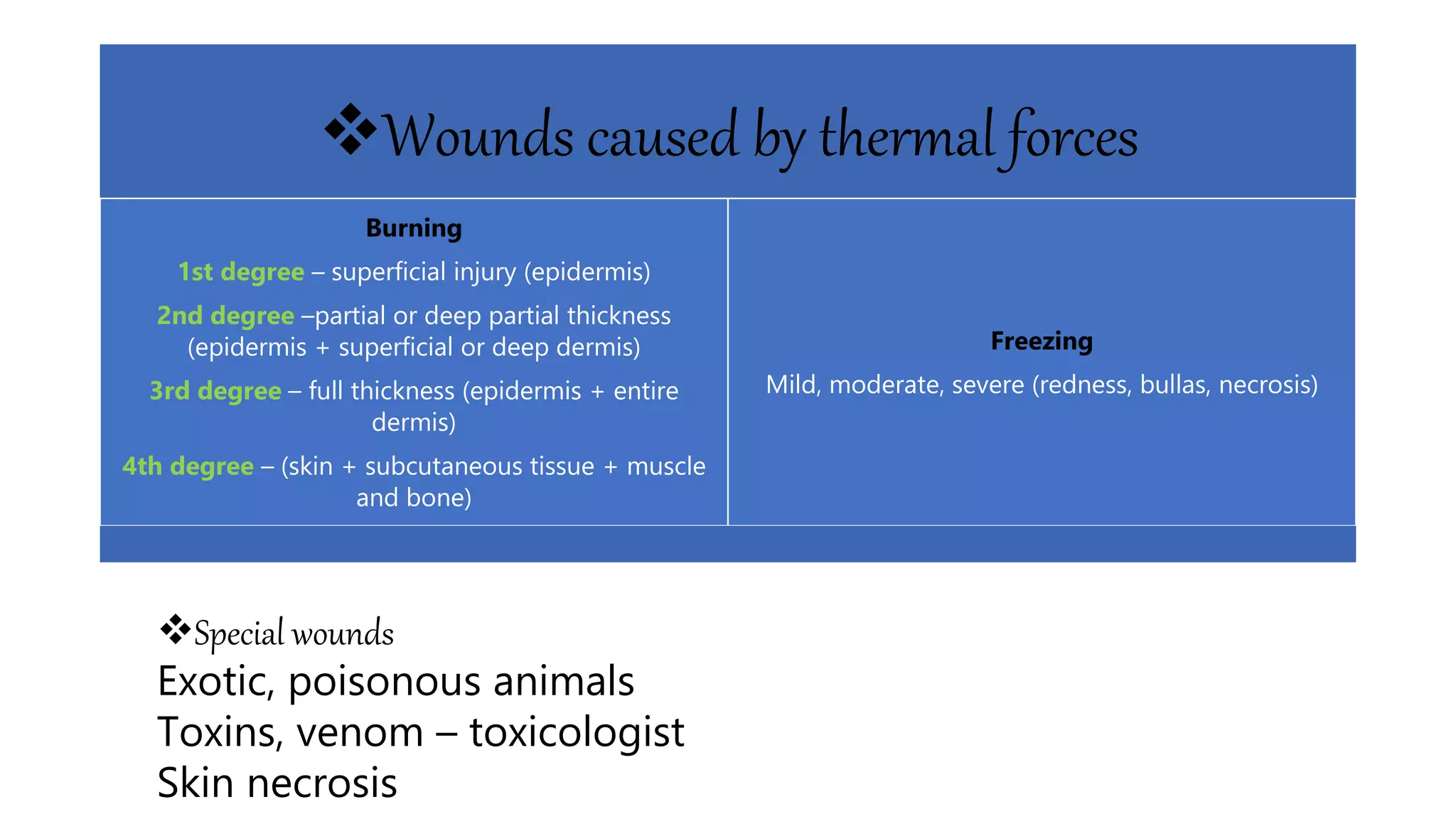
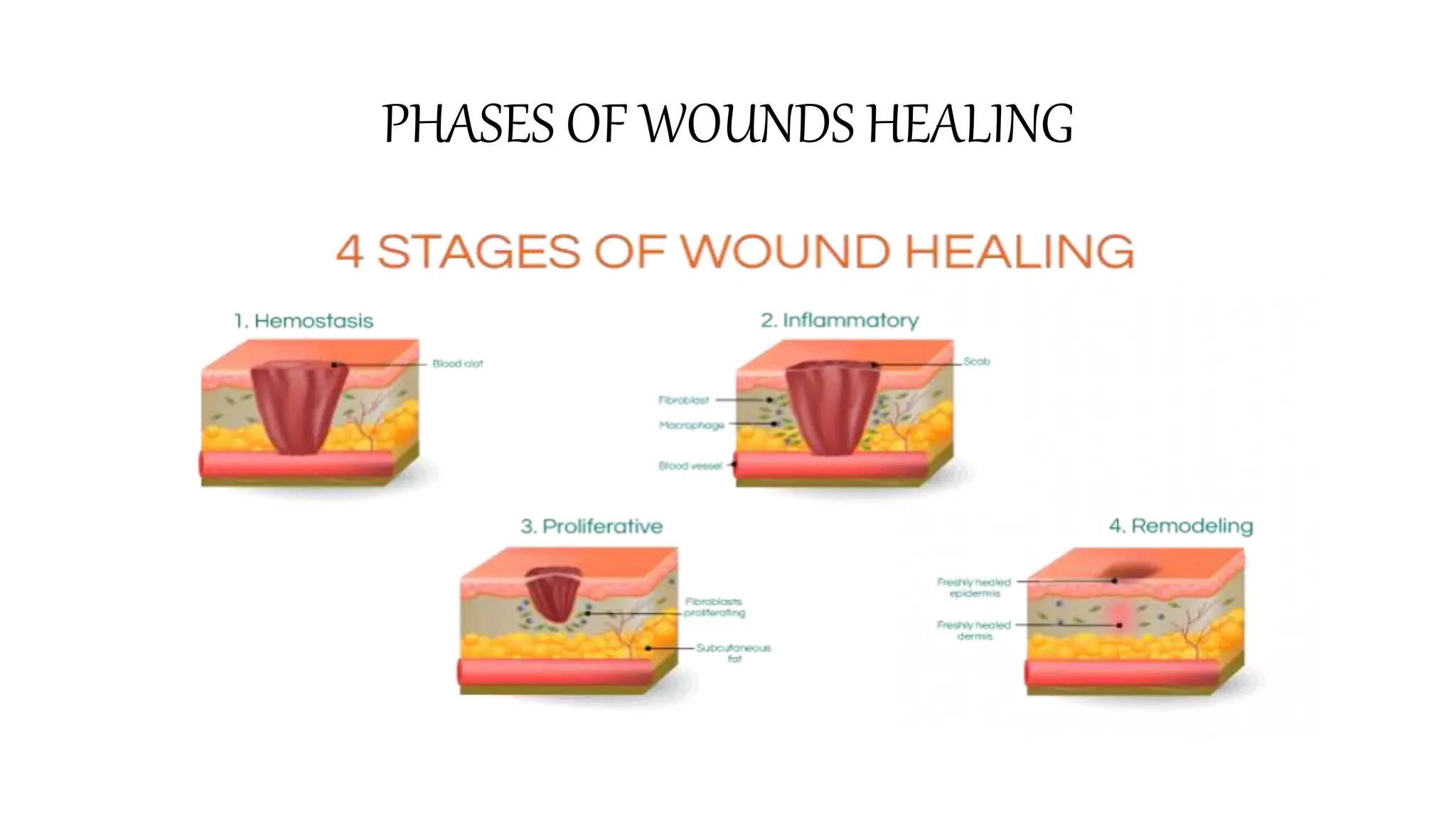
Wound management involves classifying wounds based on their origin, depth, and bacterial contamination. The document outlines the stages of wound healing - inflammation, proliferation, and maturation. Local and systemic factors can affect wound healing. Physiotherapists play an important role in treating chronic or non-healing wounds through cleaning, debridement, dressing application, compression therapy, and patient education.