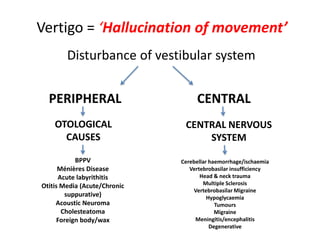
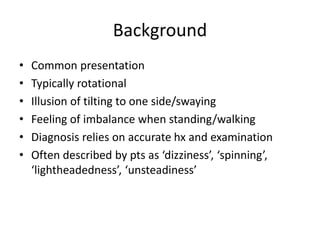
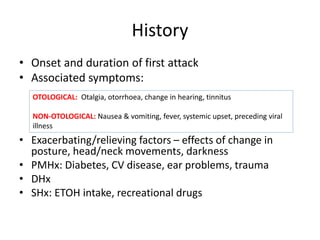
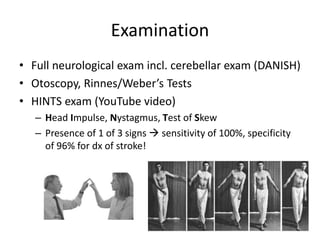
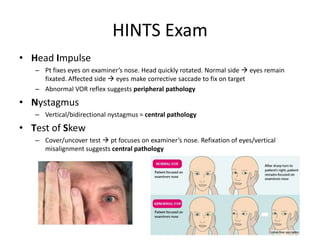
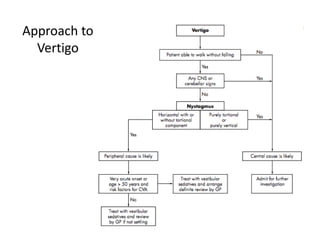
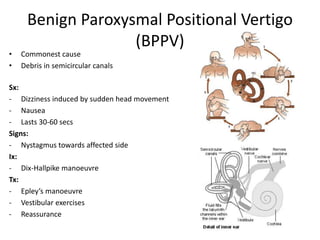
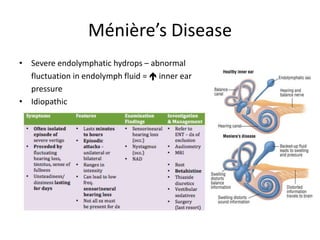
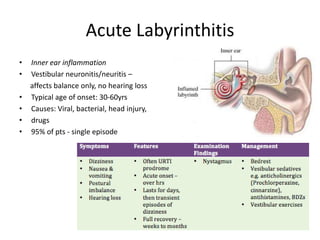
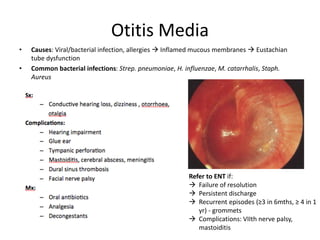
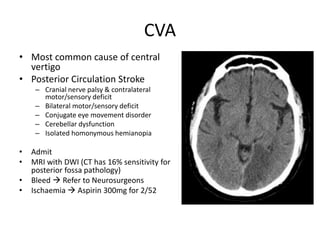
The document discusses vertigo, highlighting its definition as a hallucination of movement and detailing various central and peripheral causes, including otological and neurological origins. It emphasizes the importance of history and examination in diagnosis and describes specific types of vertigo such as benign paroxysmal positional vertigo (BPPV) and Ménière’s disease, along with their symptoms, signs, and treatments. It further notes the significance of differentiating central causes of vertigo, particularly those related to the posterior circulation stroke.