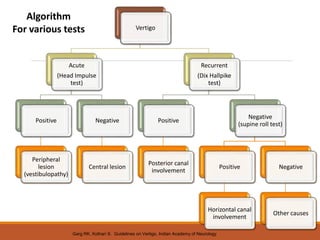
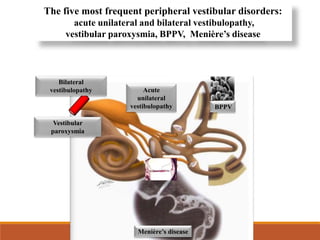
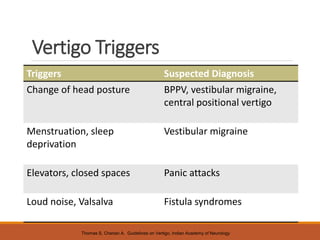
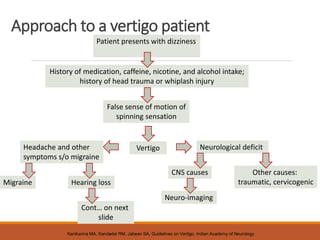
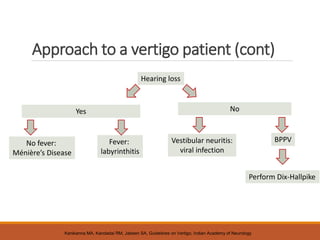
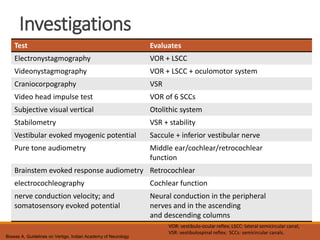
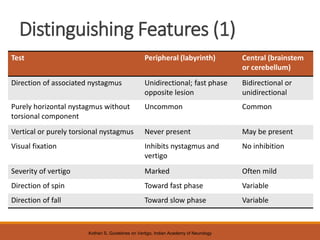
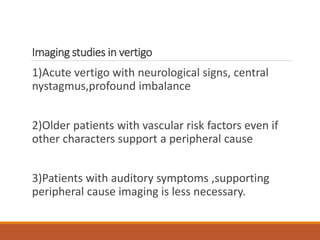
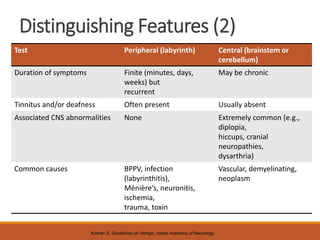
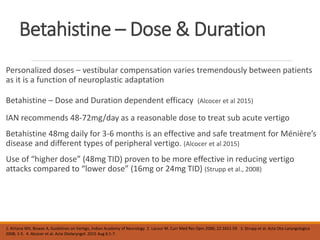
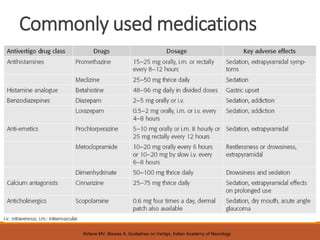
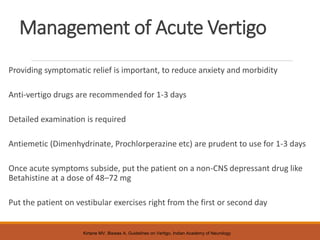
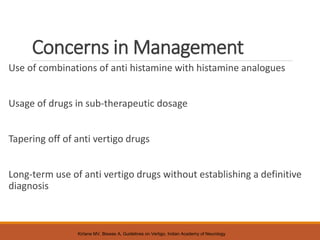
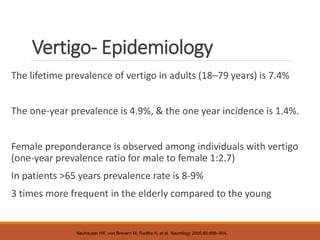
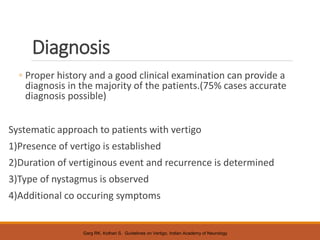
The document discusses the definition, epidemiology, diagnosis, and management of vertigo, characterized by the sensation of motion without actual movement. It highlights a significant lifetime prevalence of vertigo, particularly among females and the elderly, and outlines diagnostic approaches and treatment options, including vestibular rehabilitation and pharmacotherapy. Effective management requires accurate diagnosis, with a focus on alleviating anxiety and addressing underlying conditions while utilizing specialized exercises and medications like betahistine.
![Vertigo- Definition
‘The sensation of motion when no motion is occurring relative to
earth’s gravity’1
A feeling of movement, a sensation as if the external world were
revolving around the patient (objective vertigo) or as if he himself
were revolving in space (subjective vertigo)2
Sense of rotation
Symptom expression of disorder of vestibular system
1. Committee on Hearing and Equilibrium , Otolaryngol Head Neck Surg 1995;113:181–5. 2. International Classification of Disease [Online] Access at
http://www.icd9data.com/2012/Volume1/780- 799/780-789/780/780.4.htm](https://image.slidesharecdn.com/2-240613161555-cdeb36c5/85/2-Vertigo-Diagnosis-Management_Short-version-pptx-2-320.jpg)

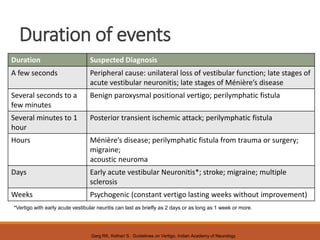
![Duration of vertiginous event and recurrence
1) BPPV: few seconds to <1 min [recurrent]
2)Menieres disease:20 min to 20 hr/few hr[recurrent]
3)Migraine associated vertigo: >few min to 60min [recurrent]
4)Acute long duration:vestibular neuritis,labyrinthitis,labyrinthine
concussion/ischemia
cerebellar infarct/ischemia,brain stem infarct/ischemia](https://image.slidesharecdn.com/2-240613161555-cdeb36c5/85/2-Vertigo-Diagnosis-Management_Short-version-pptx-7-320.jpg)