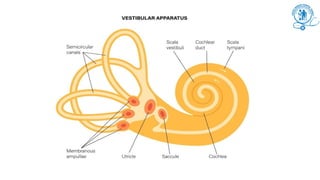
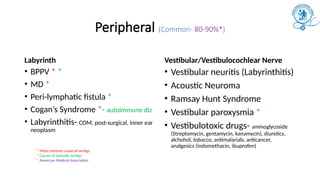
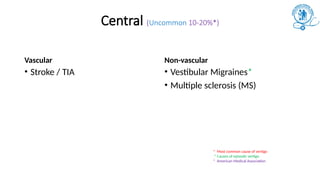
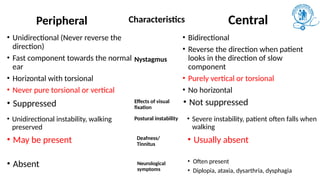
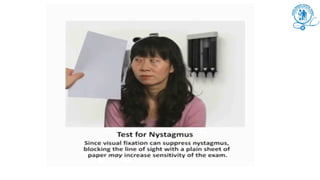
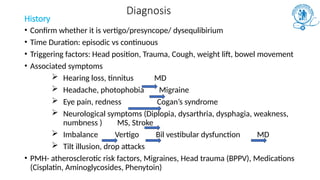
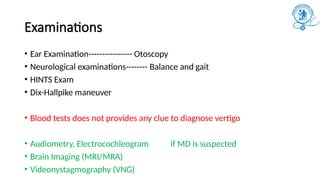
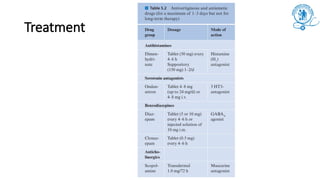
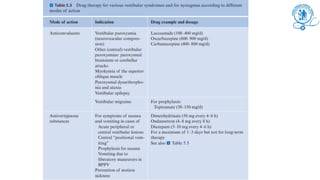
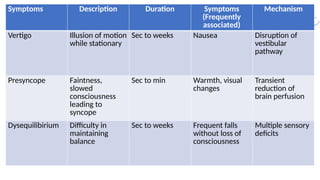
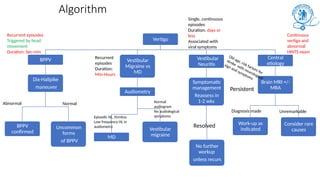
This document discusses the classification, diagnosis, and treatment of vertigo, emphasizing the importance of differentiating it from presyncope and disequilibrium. It covers both peripheral and central causes of vertigo, with a focus on common conditions like BPPV, vestibular migraines, and neurological implications. Diagnostic approaches include history taking, neurological examinations, and various imaging techniques to determine the underlying causes.