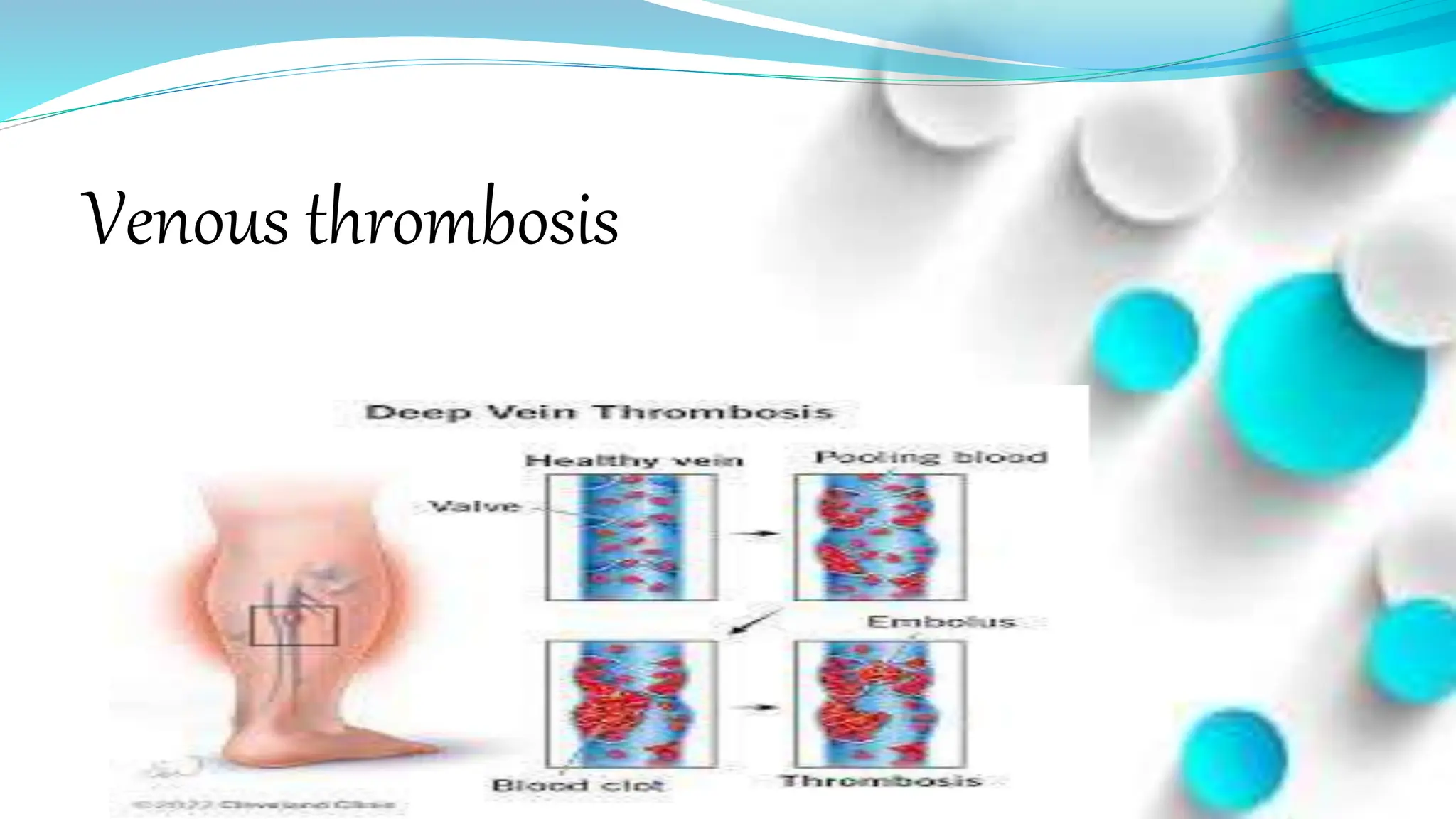
The document discusses varicose veins and venous thrombosis. It defines varicose veins as dilated, elongated veins caused by venous hypertension. Valves in the veins and factors like muscle contraction help venous return. Varicose veins are caused by prolonged standing, family history, pregnancy, aging and other factors. Symptoms include leg pain, swelling and heaviness. Treatment involves leg elevation, compression stockings, sclerotherapy and surgery. Venous thrombosis occurs when blood clots form in the veins. Risk factors include immobility, surgery and genetic factors. Symptoms are pain, swelling and fever. Treatment aims to prevent further clots and embolisms with anticoagulants, compression and exercise. Nursing