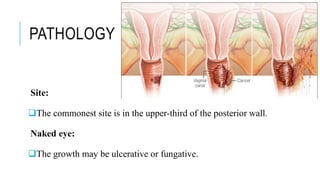
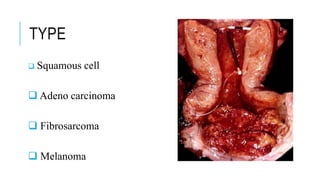
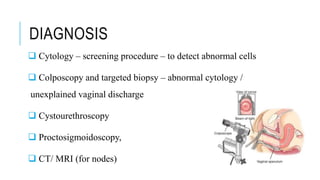
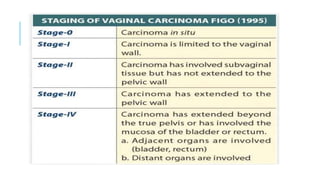
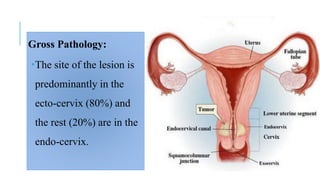
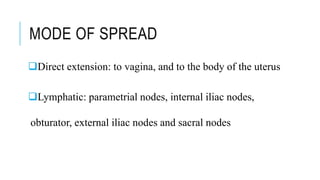
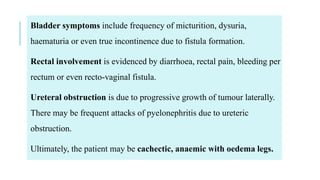
Vaginal carcinoma is a rare type of cancer making up about 1% of genital malignancies. Risk factors include HPV, a history of cervical cancer, and exposure to diethylstilbestrol (DES) in utero. Symptoms may include abnormal vaginal bleeding, discharge, or asymptomatic growths. Diagnosis involves cytology, colposcopy, and biopsy of any abnormal cells or growths. Treatment depends on the type and stage but can include surgery, radiation, chemotherapy, or a combination. The most common type is squamous cell carcinoma arising from the upper third of the posterior vaginal wall. It typically spreads locally or via lymph nodes but can metastasize to distant organs in more advanced cases.