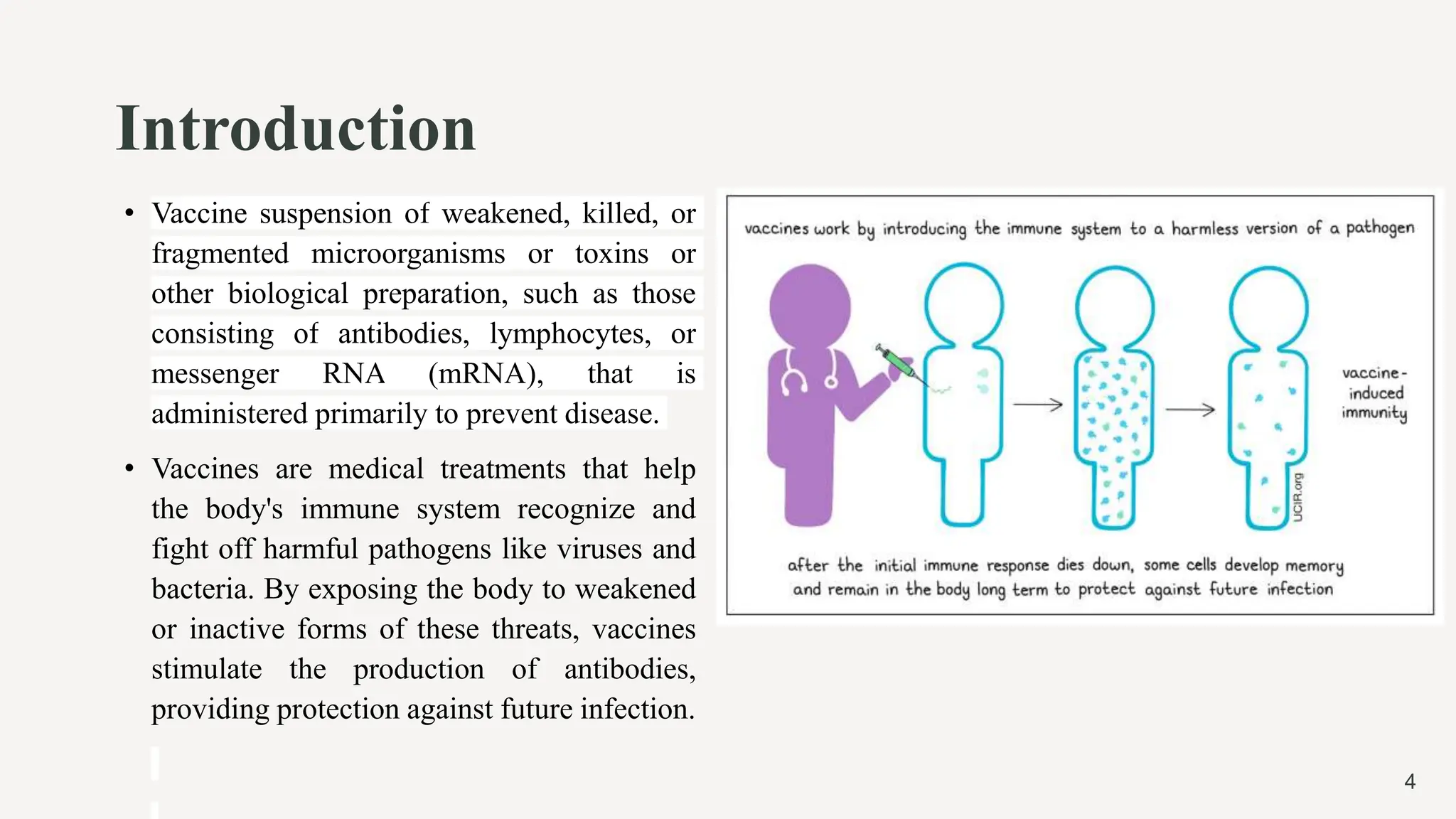
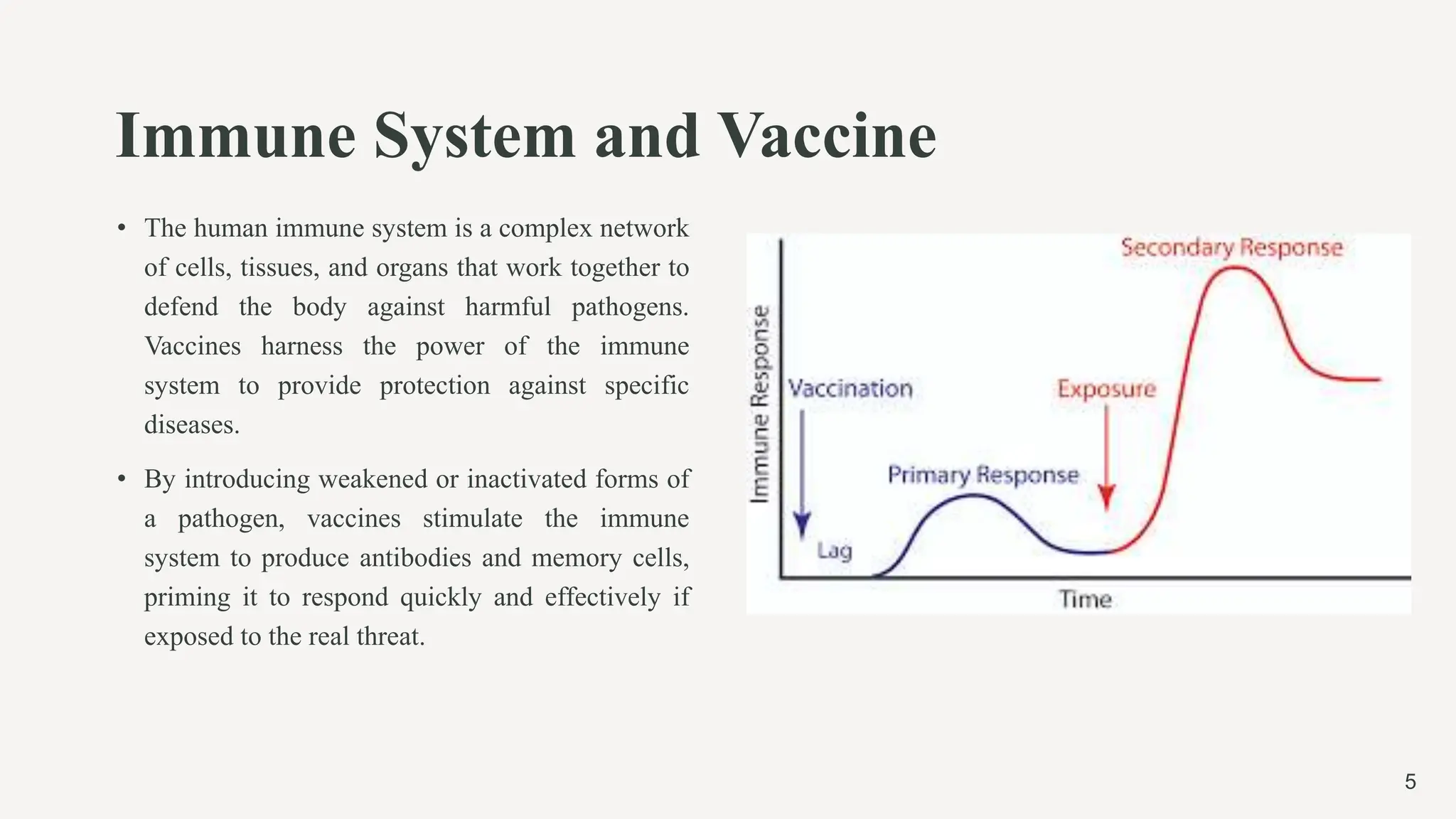
The document provides a comprehensive overview of vaccines, including their history, principles, types, and modes of action. It outlines key advancements in vaccination, such as Edward Jenner's smallpox vaccine and Jonas Salk's polio vaccine, while detailing how vaccines work with the immune system to provide protection against various diseases. Furthermore, it categorizes vaccine types, including live attenuated, inactivated, subunit, conjugate, and mRNA vaccines, explaining their mechanisms and examples.