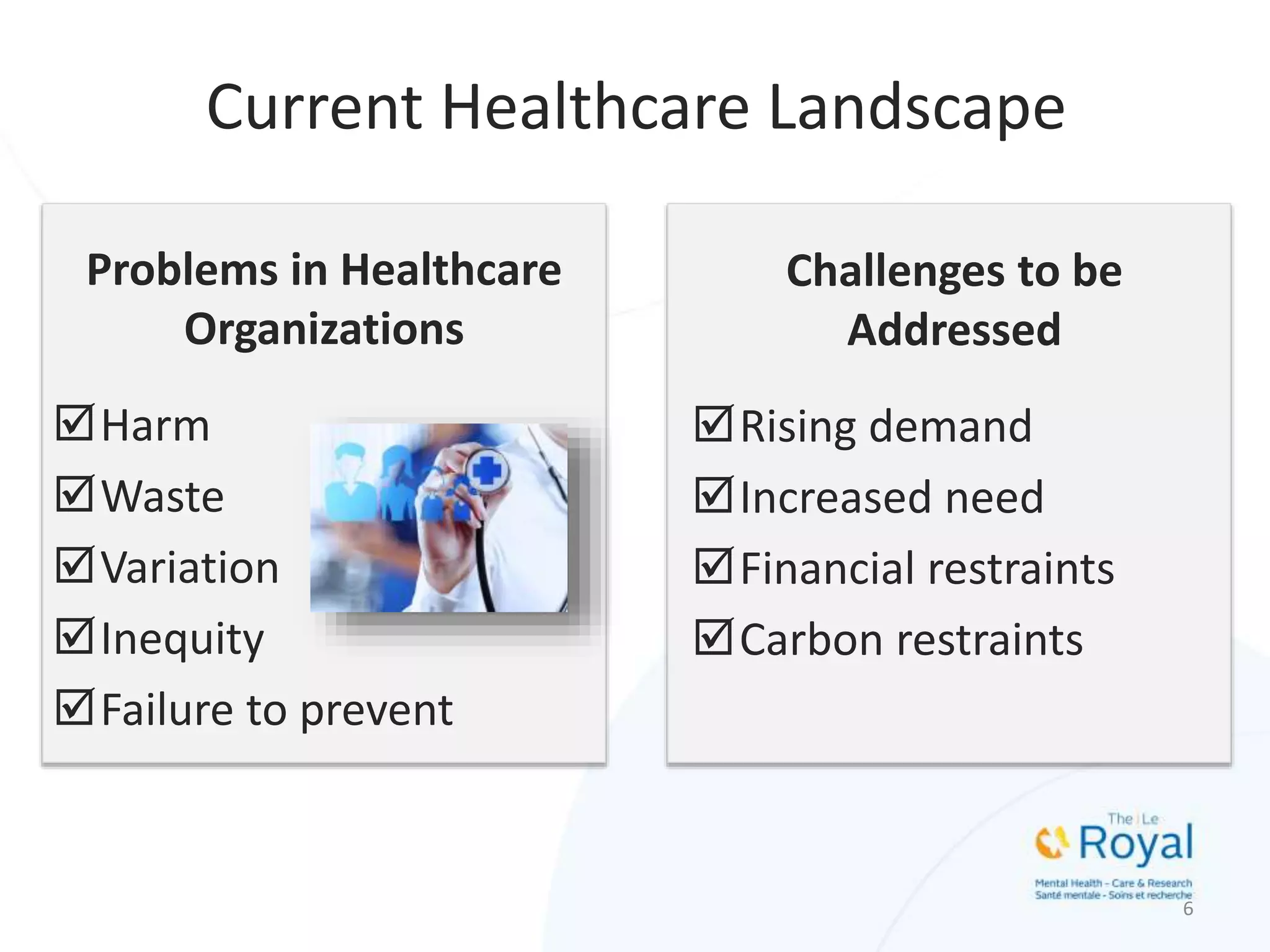
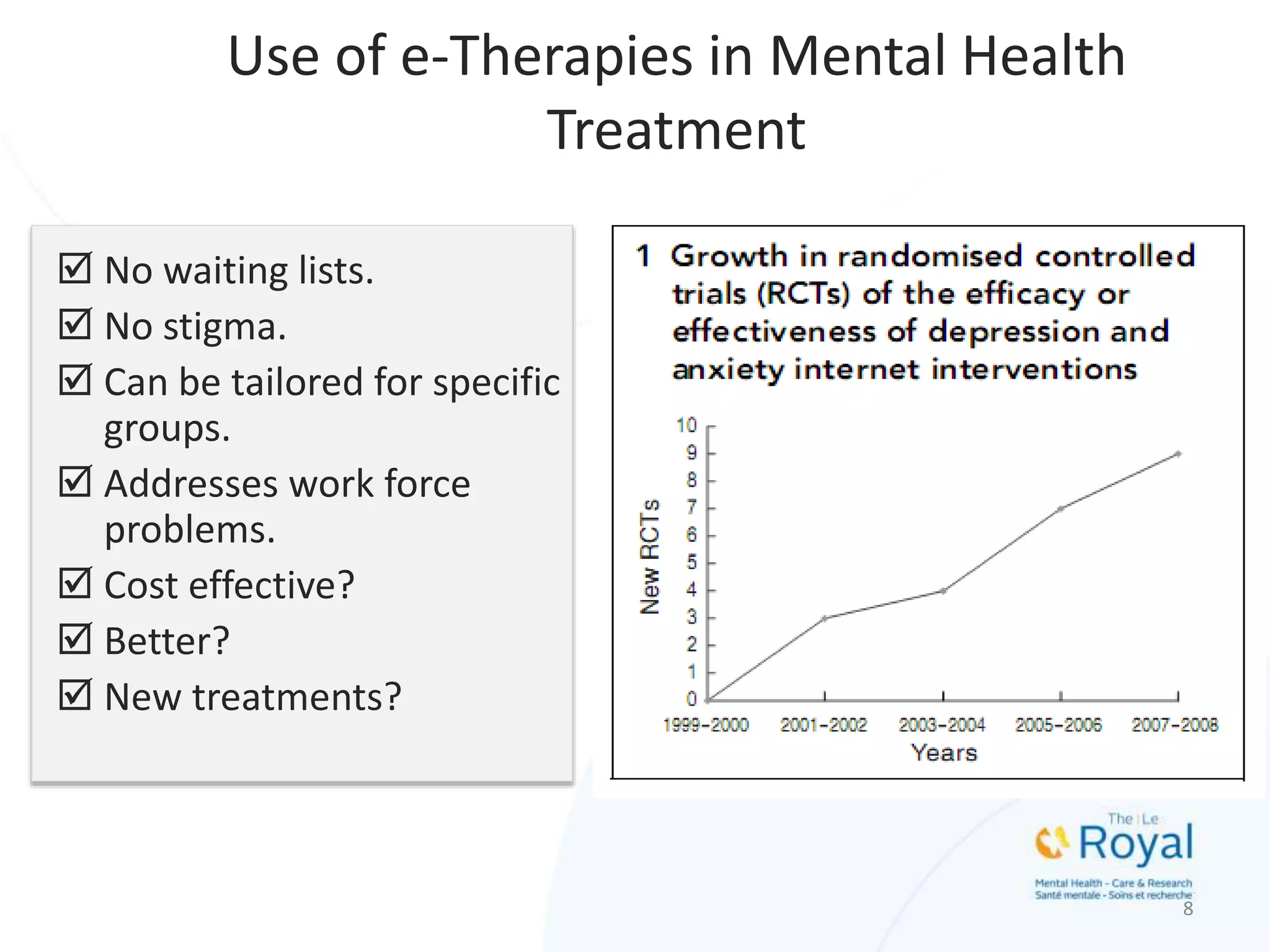
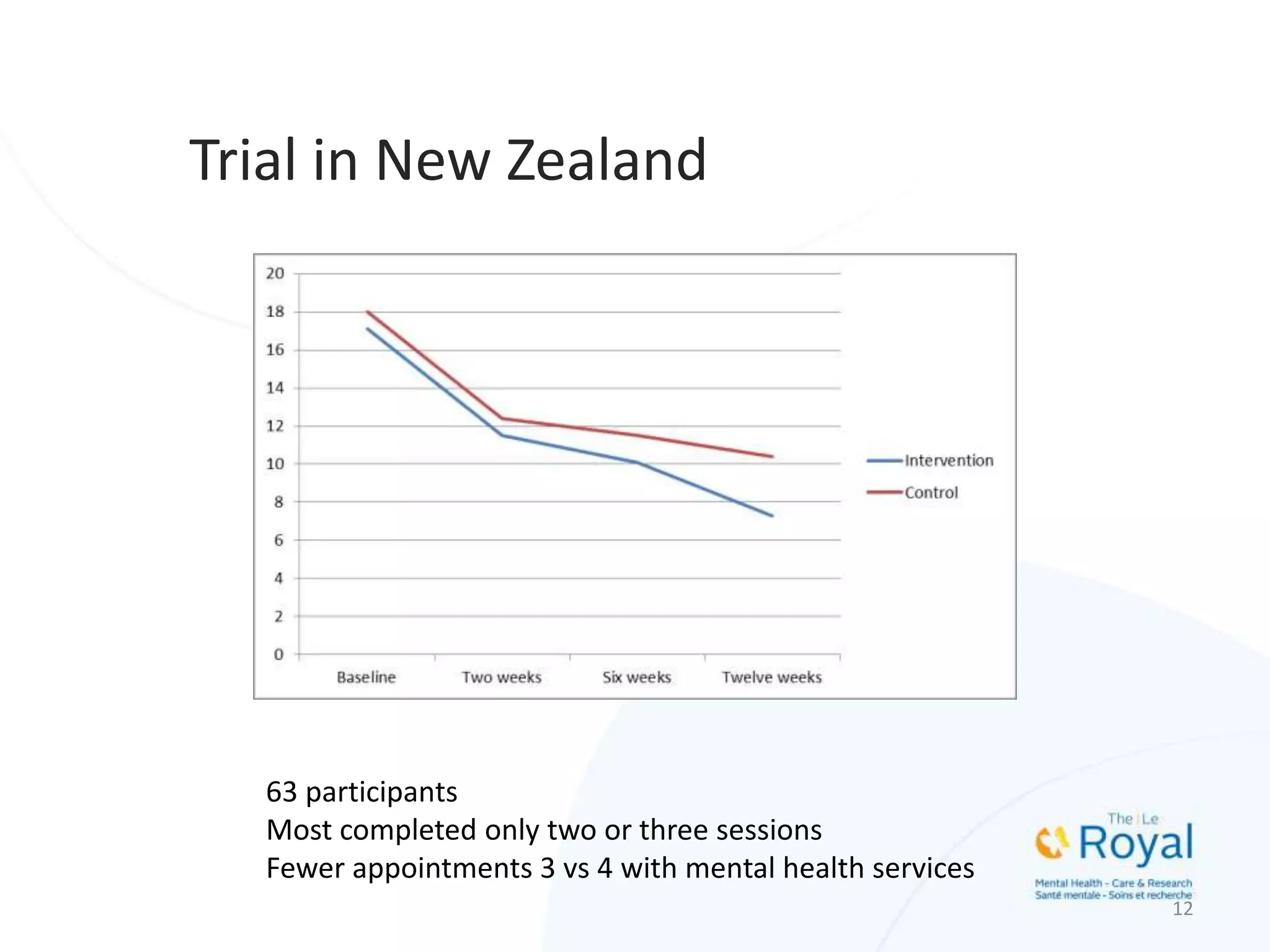
Dr. Simon Hatcher discusses the evolution of e-therapies for mental health treatment, emphasizing their potential to address current healthcare challenges like demand and inequity. The presentation outlines various generations of digital therapy, highlighting their effectiveness, limitations, and the need for personalized and integrated approaches in mental health care. Innovations such as smartphone applications, virtual reality, and wearable technologies are also explored for their applications in treating mental health issues.