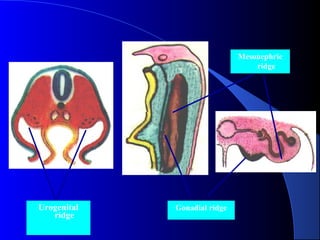
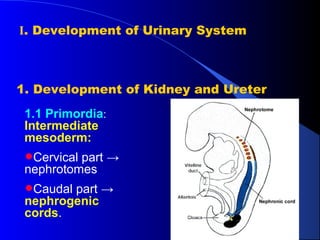
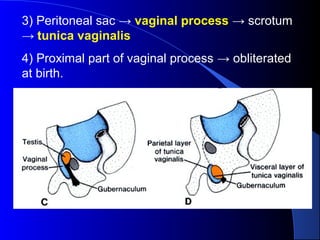
1. The document discusses the development of the urinary and genital systems from primordia to fully formed organs, including the development of the kidneys, gonads, genital ducts, bladder, and external genitalia.
2. It describes the sex differentiation of the gonads, with the testes developing in males due to SRY and the ovaries developing in females in the absence of SRY.
3. Various congenital malformations are also summarized such as cryptorchidism, hermaphroditism, and hypospadias.