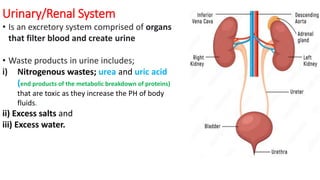
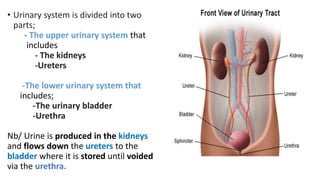
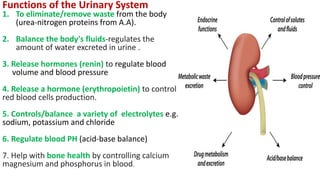
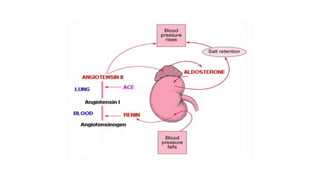
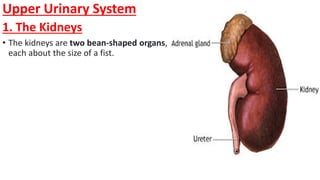
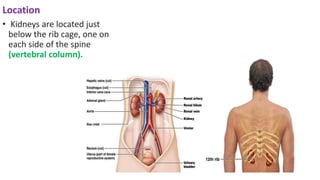
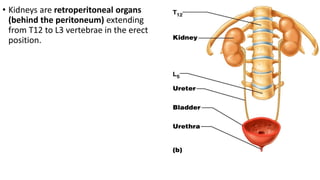
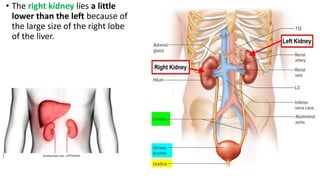
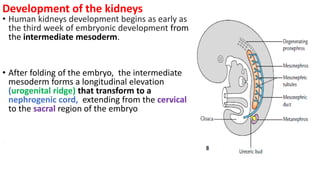
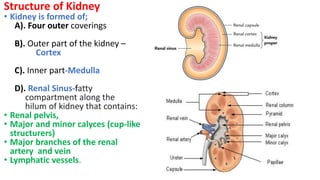
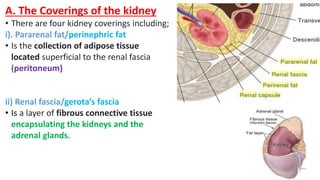
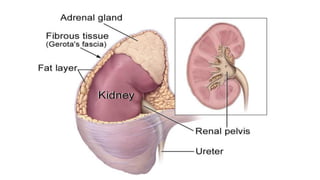
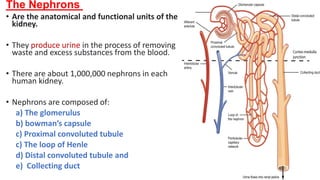
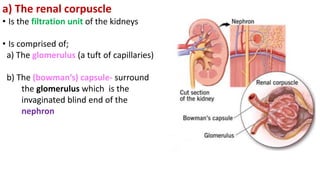
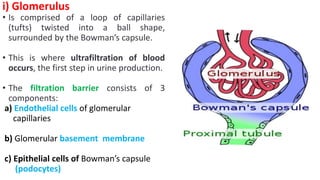
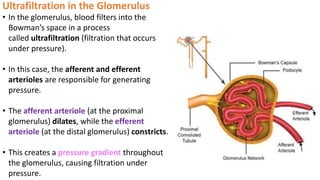
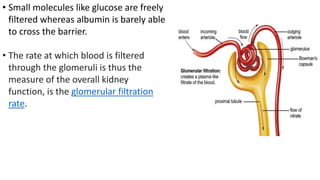
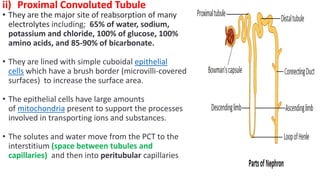
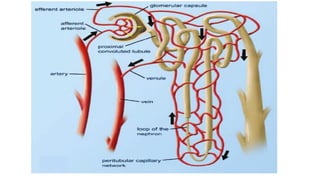
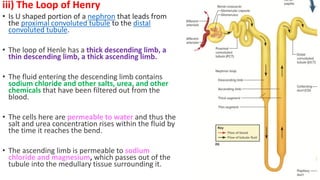
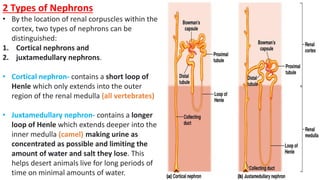
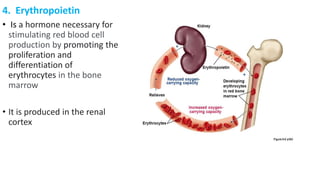
The urinary/renal system is an excretory system that filters blood and produces urine, consisting of the kidneys, ureters, urinary bladder, and urethra. Its functions include waste elimination, fluid balance, hormone release, and electrolyte regulation. The kidneys, with their complex structure and nephron function, are crucial in processing blood and maintaining homeostasis.