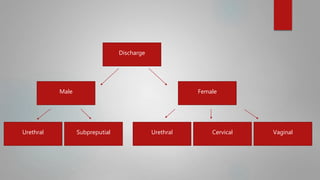
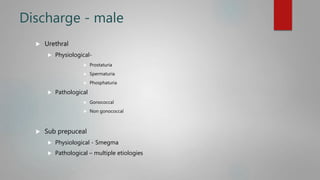
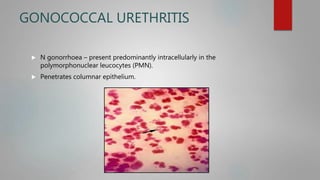
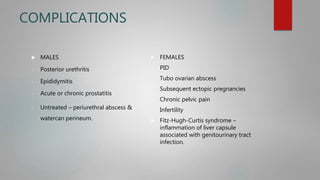
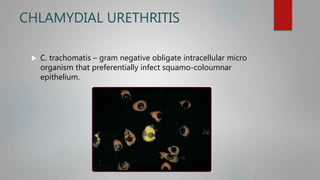
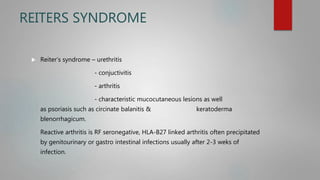
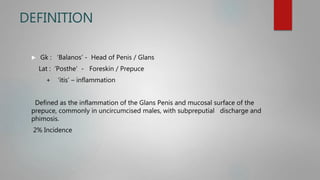
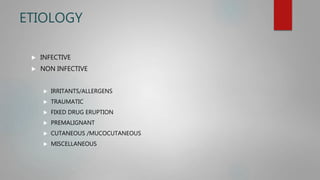
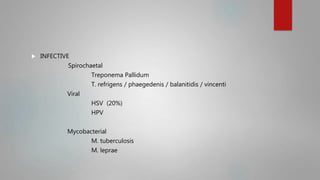
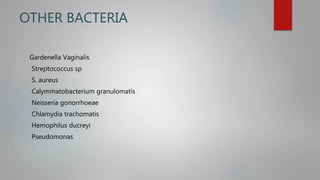
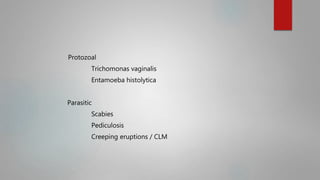
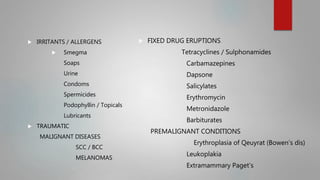
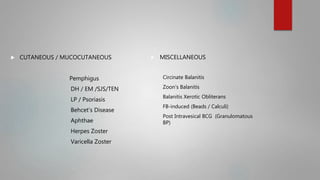
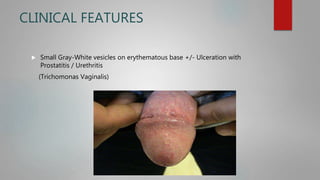
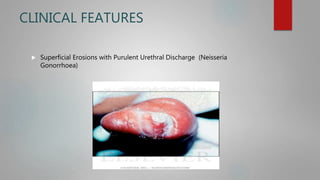
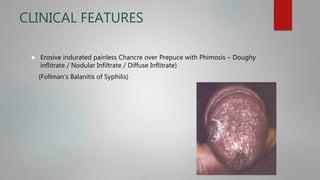
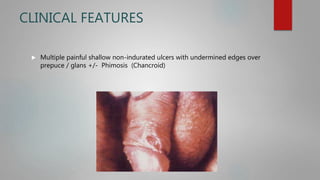
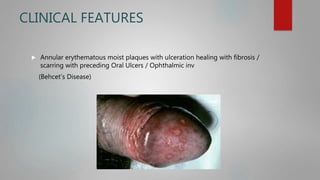
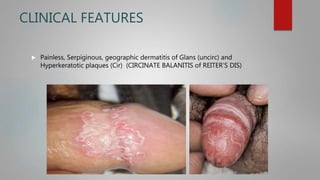
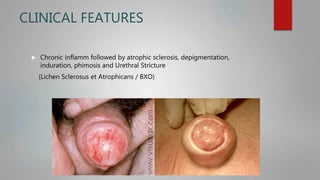
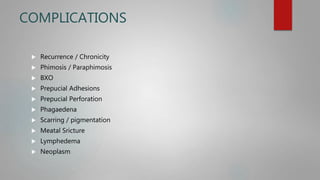
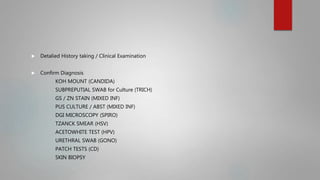
This document discusses urethritis and balanoposthitis. It begins by defining urethritis as inflammation of the urethra and describing the different types of urethritis including gonococcal and non-gonococcal causes. It then focuses on gonococcal urethritis caused by Neisseria gonorrhoeae. It describes the clinical features, investigations, management, and complications of gonococcal and chlamydial urethritis. The document then defines balanoposthitis as inflammation of the glans penis and prepuce. It discusses the various etiologies, clinical features, investigations, and management of balanoposthitis.