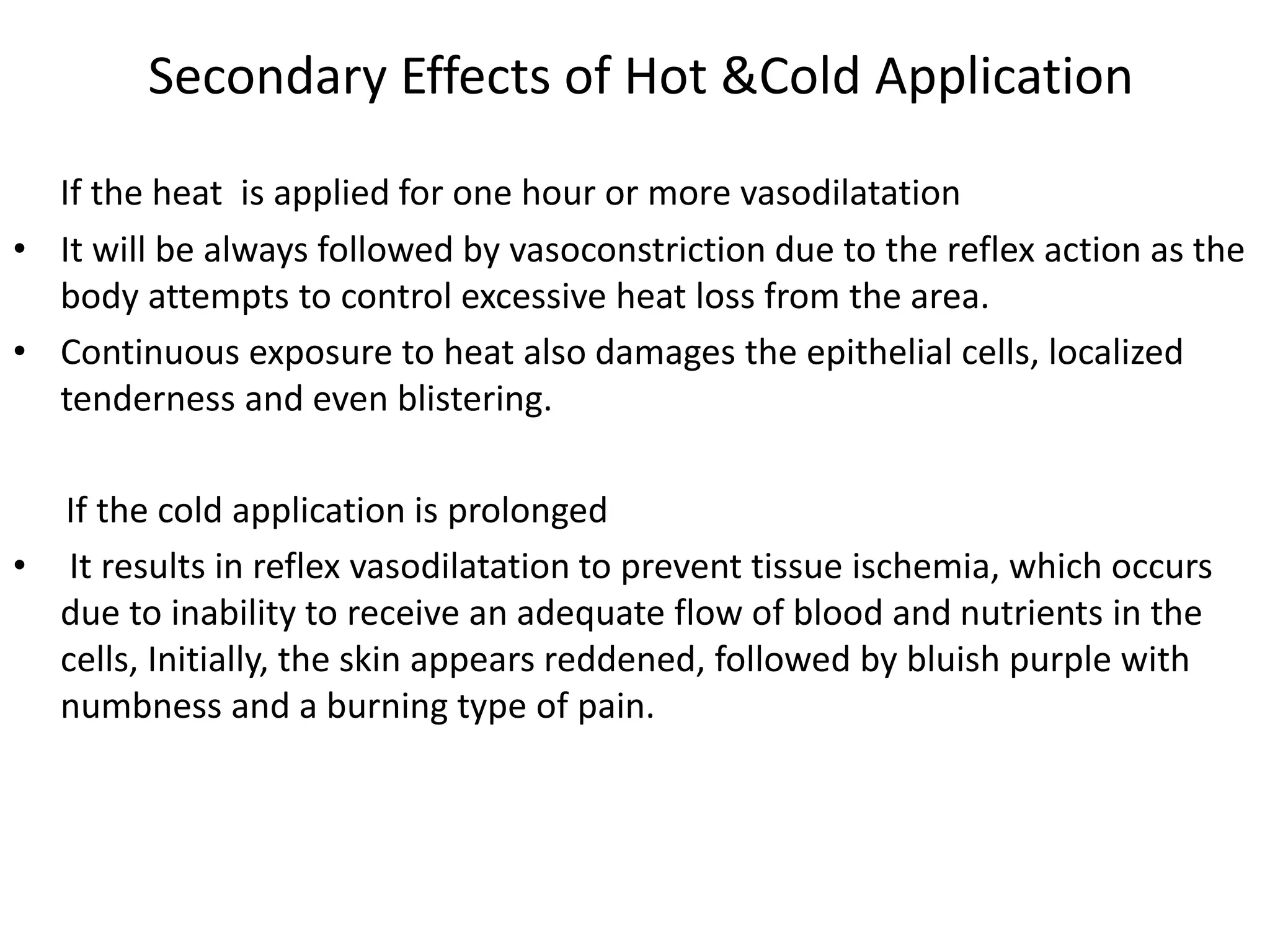
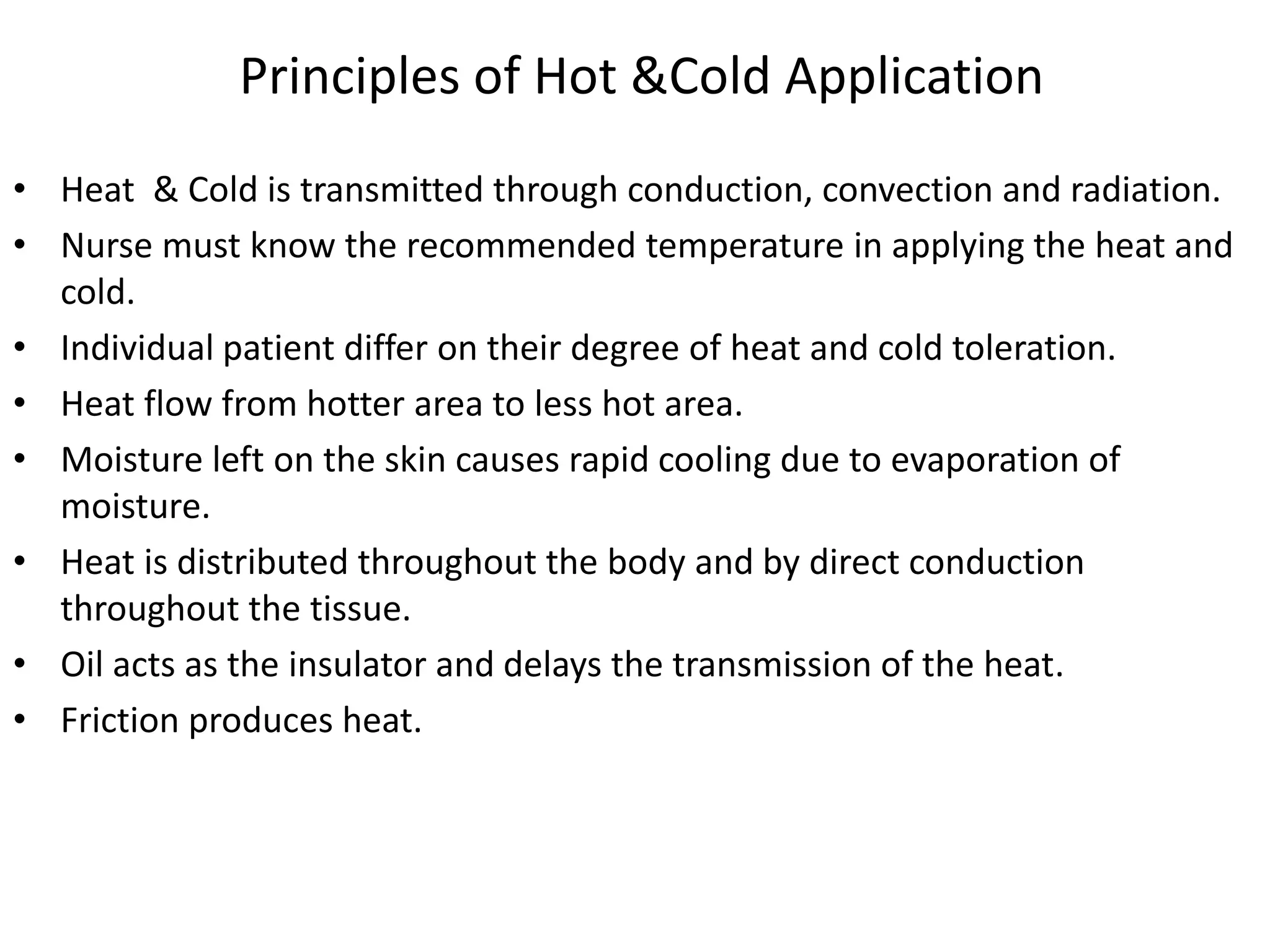
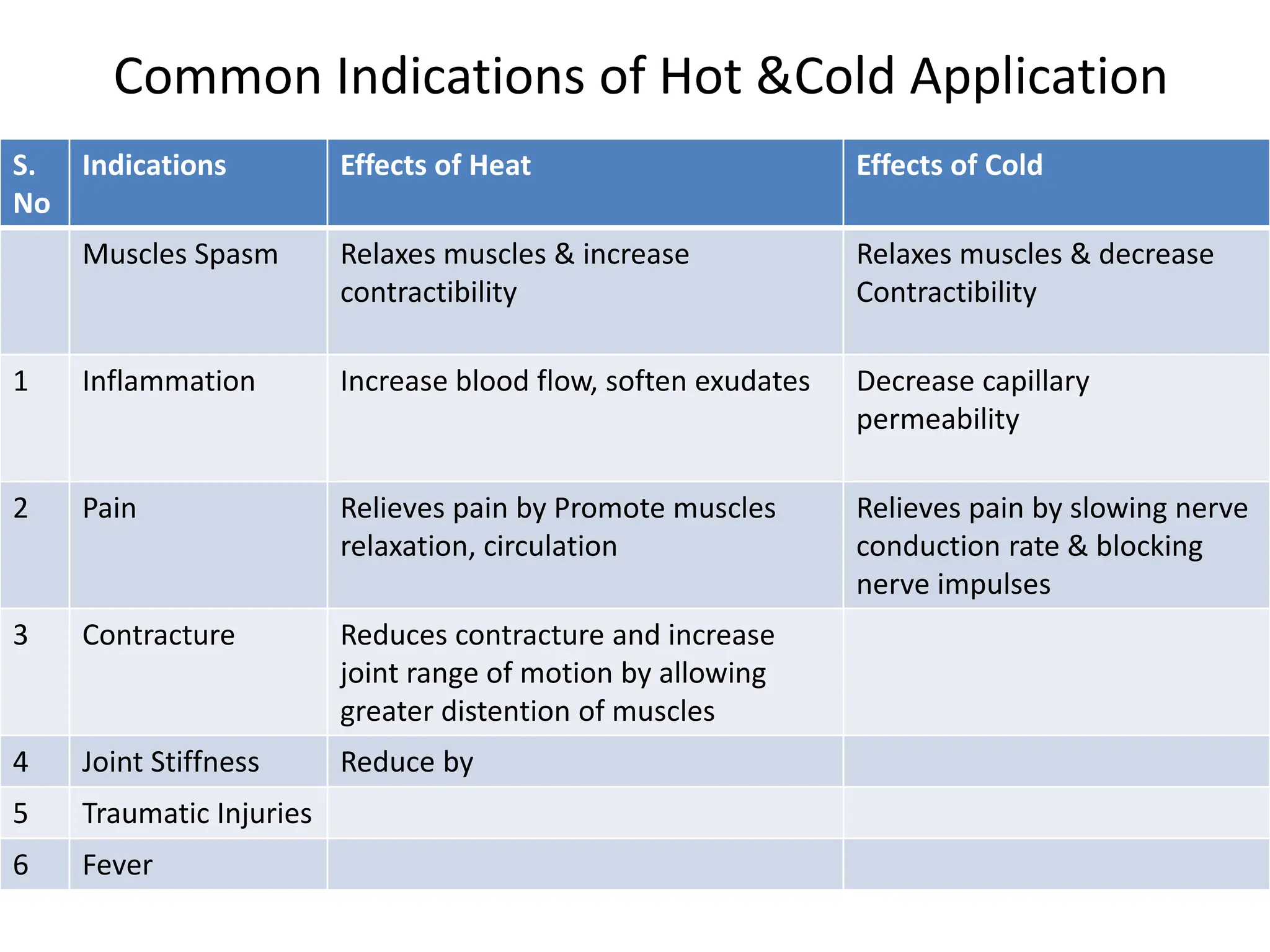
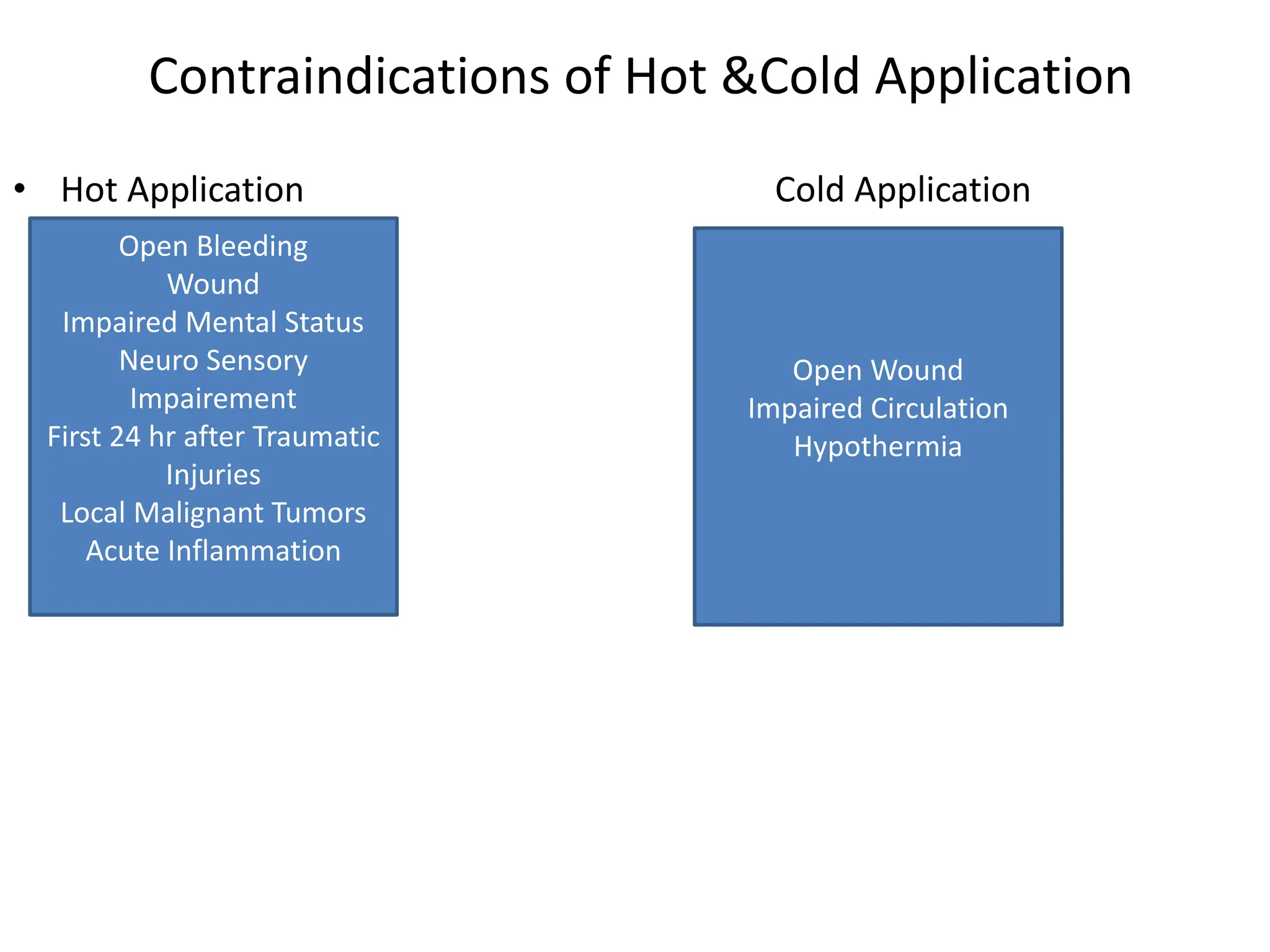
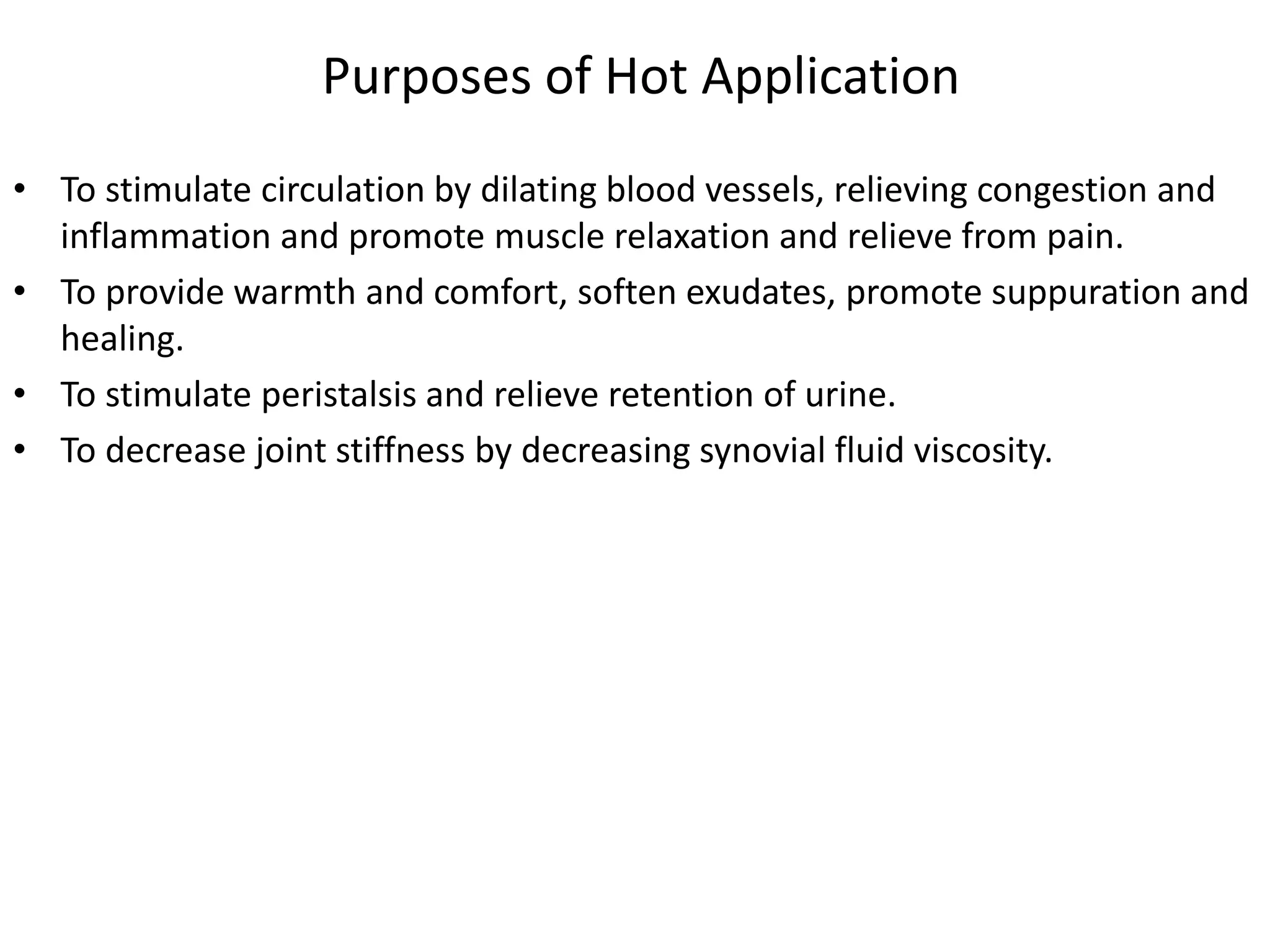
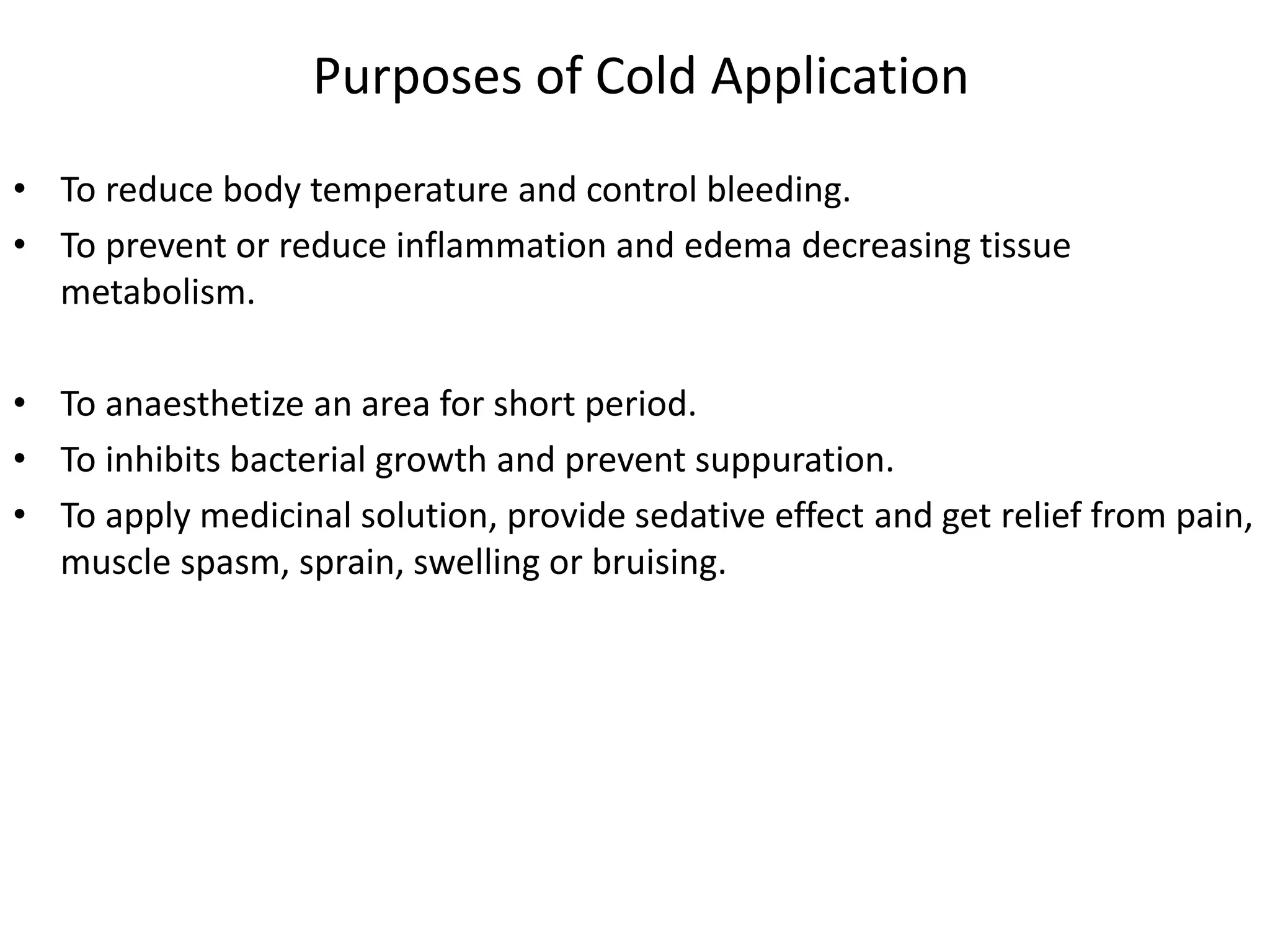
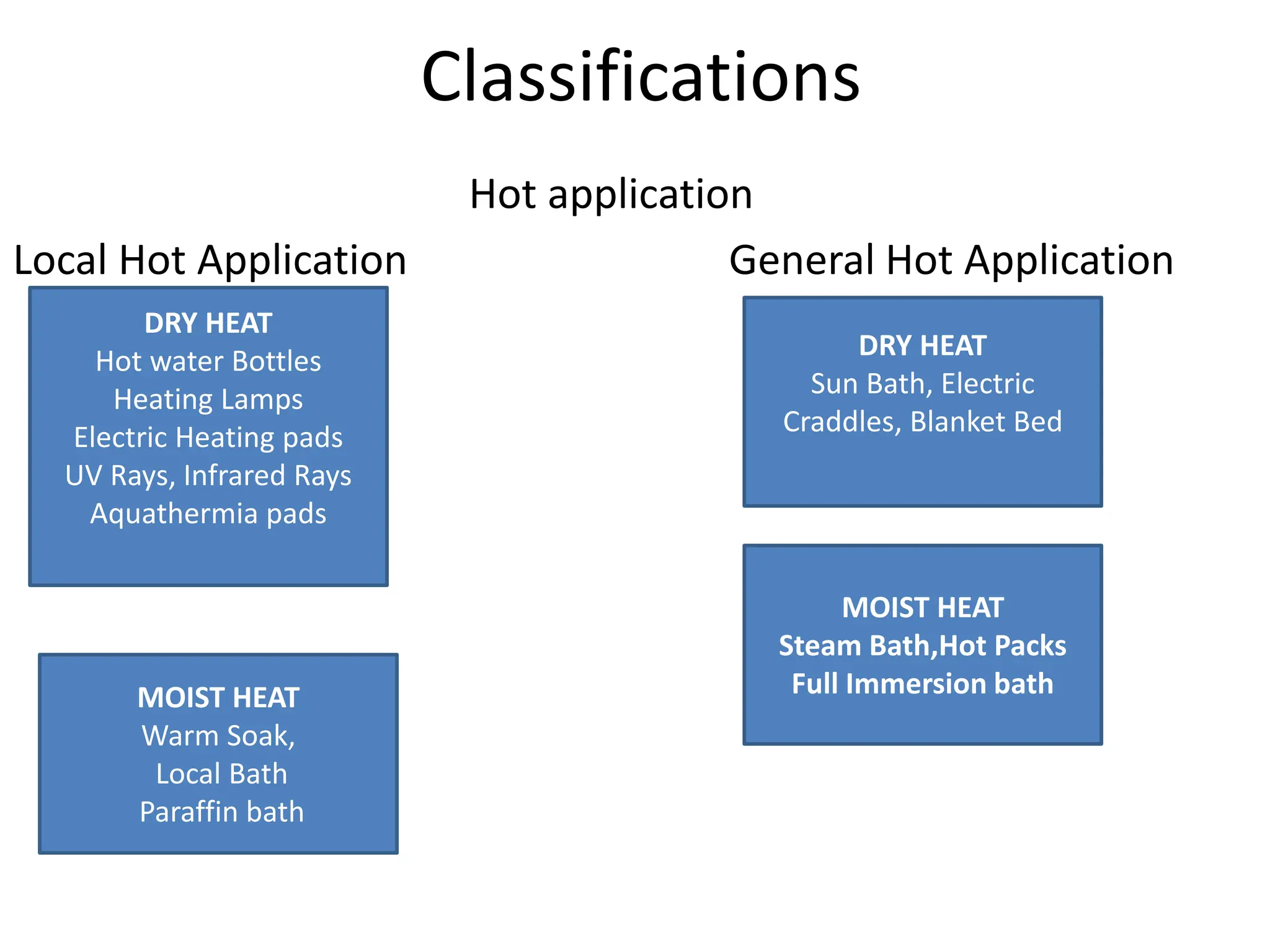
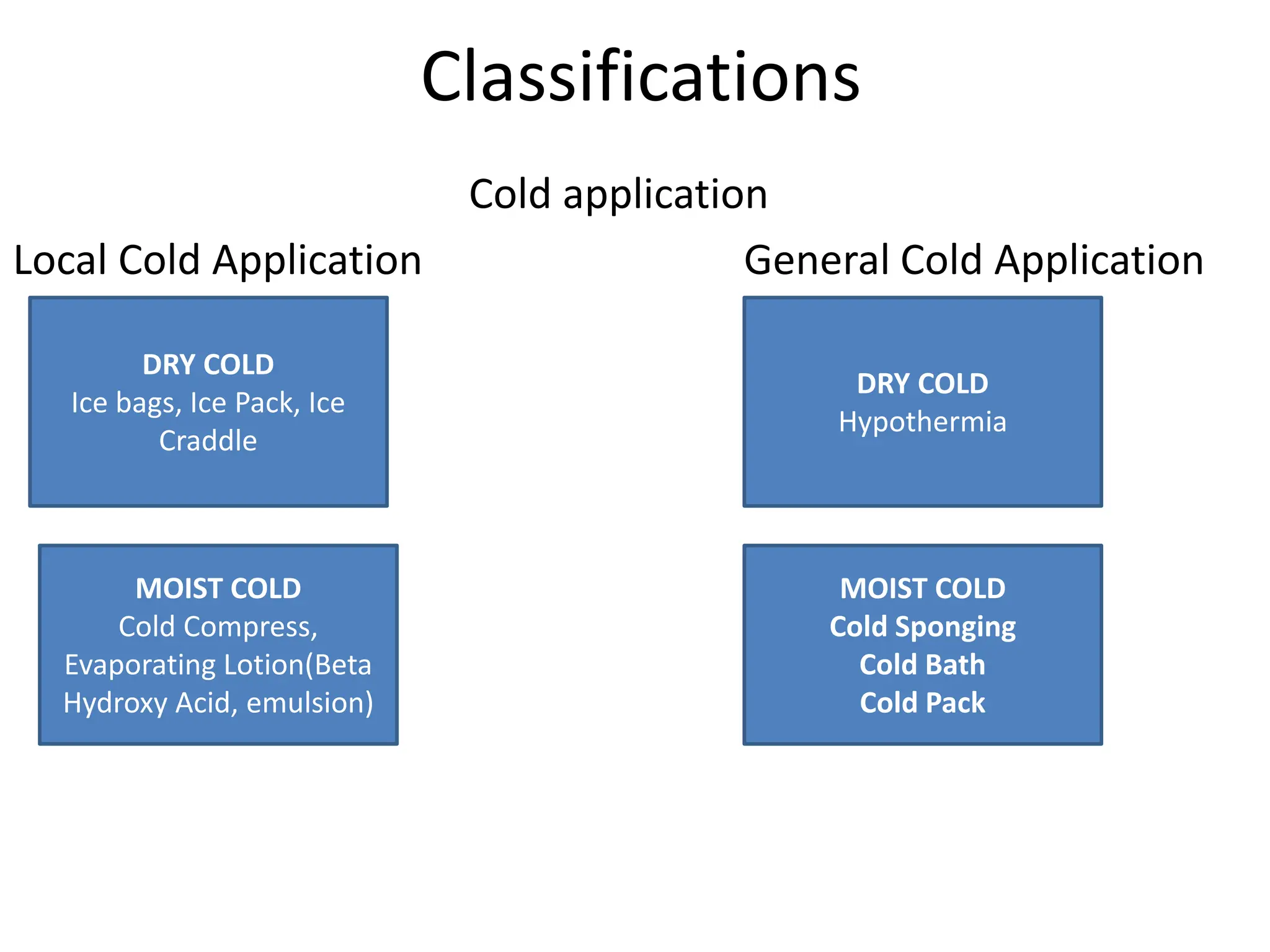
The document provides a comprehensive overview of hot and cold applications, including definitions, effects, purposes, and procedures for their application. Hot applications promote circulation and relieve pain, while cold applications reduce inflammation and control hemorrhage. It also outlines contraindications and nursing responsibilities to ensure patient safety during these treatments.