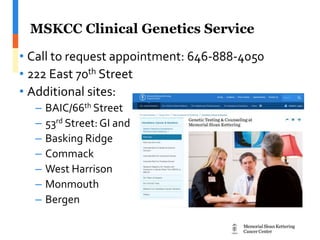
The document discusses genetic counseling related to breast and ovarian cancer, outlining its goals, processes, and the importance of understanding genetic contributions to these diseases. It emphasizes the need for genetic testing, risk assessment, and the support available for individuals with familial histories of cancer. Additionally, it provides information on how to find a genetic counselor and the different genetic syndromes linked to breast and ovarian cancer.