This document summarizes a presentation on genetic testing for cancer risk. The presentation covered:
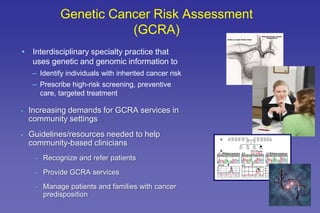
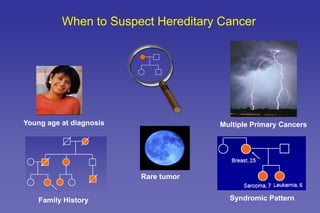
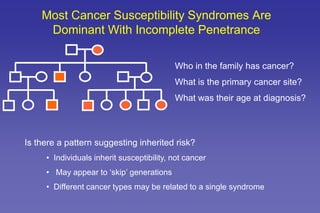
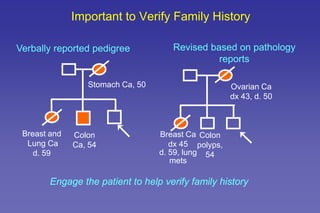
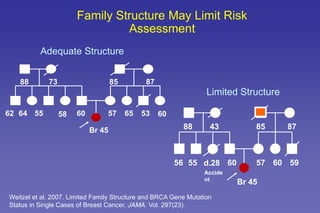
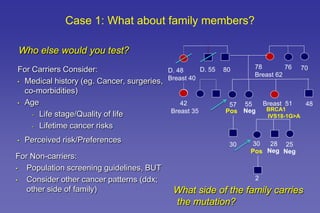
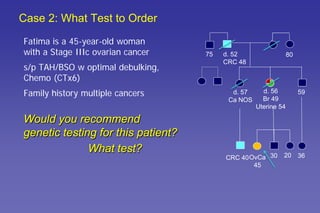
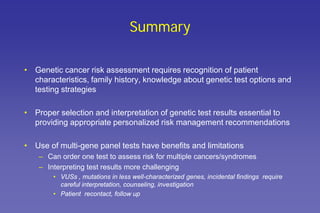
- The role of genetic cancer risk assessment in identifying inherited cancer risk.
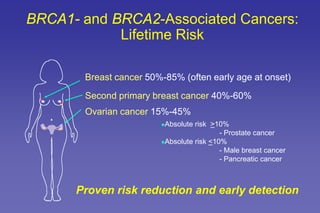
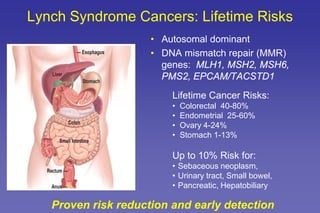
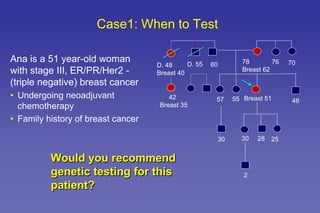
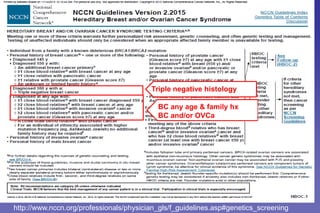
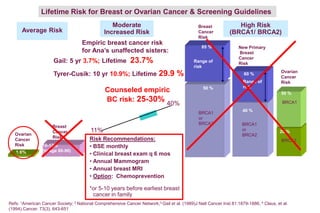
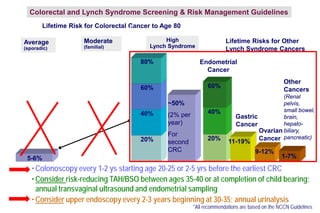
- Common hereditary cancer syndromes like BRCA1/2 and Lynch syndrome and their associated cancer risks.
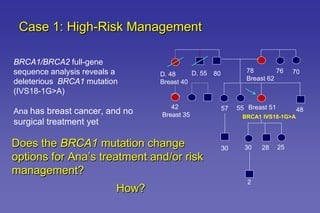
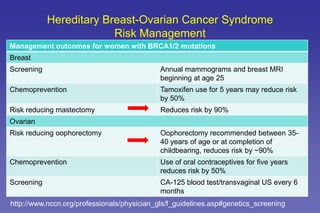
- Guidelines for cancer screening and management based on genetic test results.
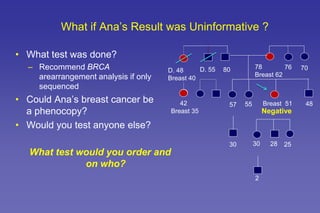
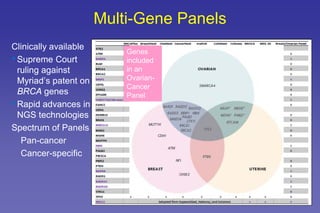
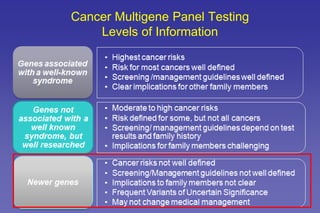
- The benefits and limitations of multi-gene cancer panels.
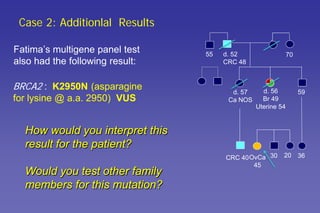
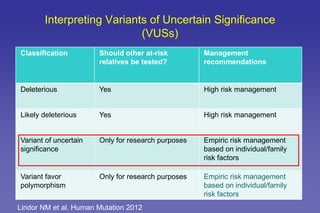
- How to interpret genetic test results and provide appropriate risk management recommendations to patients.