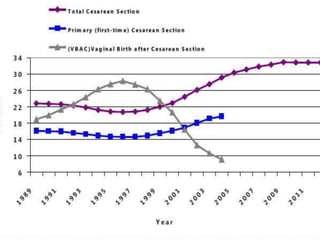
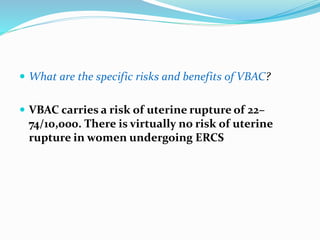
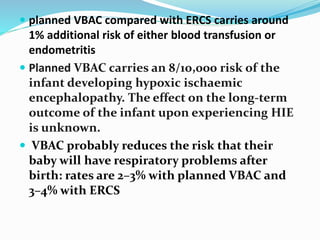
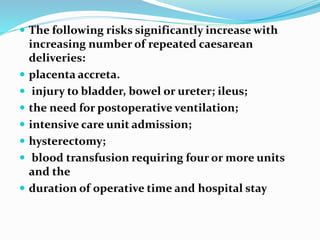
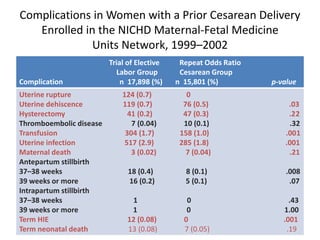
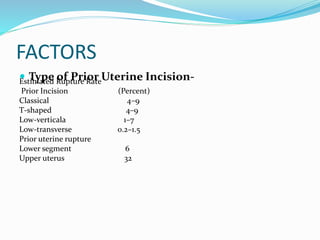
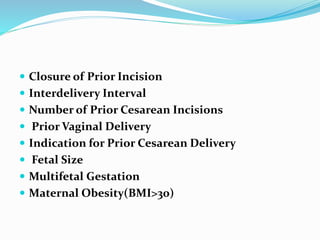
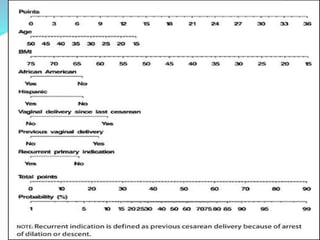
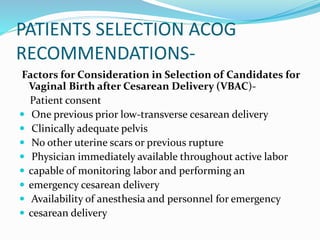
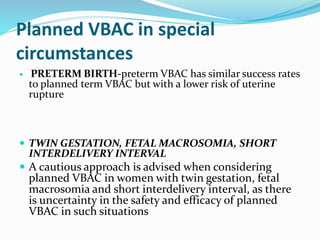
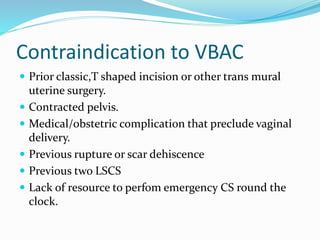
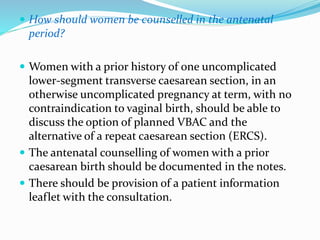
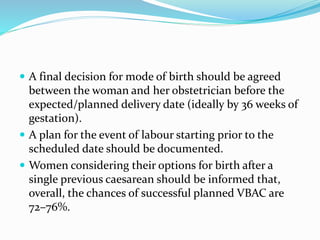
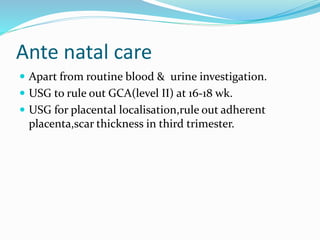
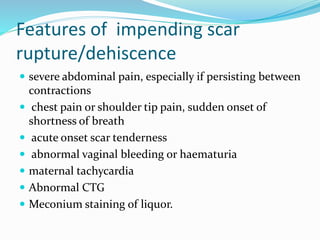
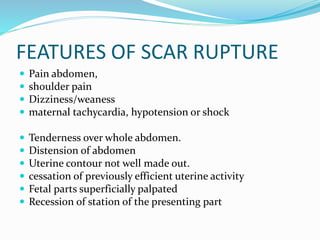
This document discusses the history and risks/benefits of vaginal birth after cesarean (VBAC) versus elective repeat cesarean section. It notes that while VBAC was originally encouraged due to risks of multiple c-sections, safety concerns led to declining VBAC rates. VBAC carries risks of uterine rupture but reduces risks of respiratory issues compared to repeat c-section. Proper patient selection and access to emergency c-section are important to support a planned VBAC attempt. The risks and benefits should be discussed thoroughly to help each woman make an informed decision.