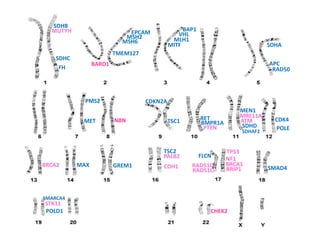
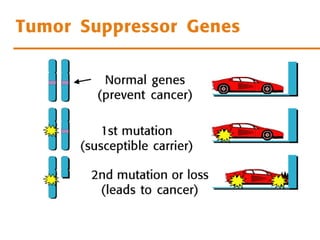
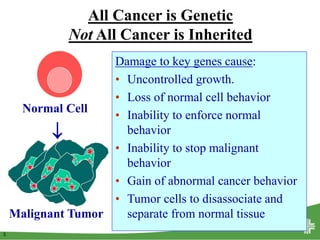
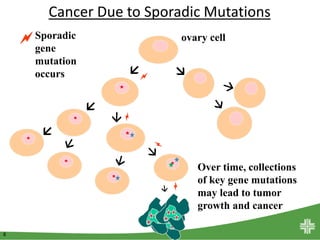
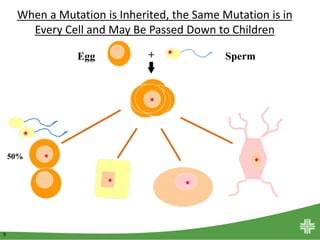
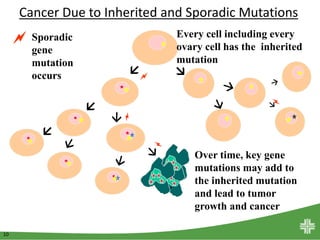
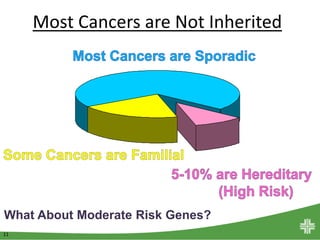
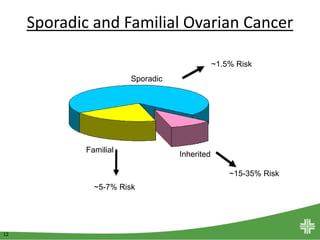
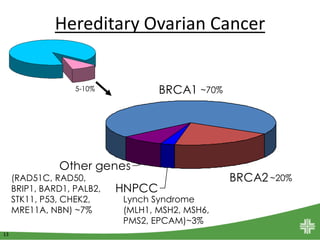
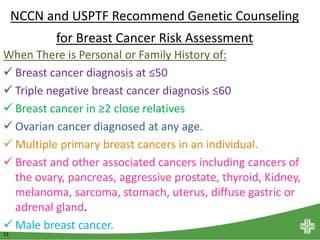
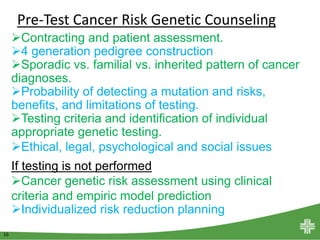
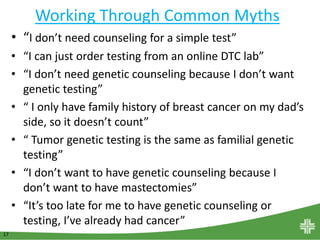
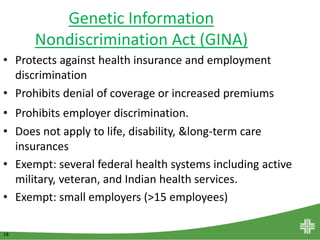
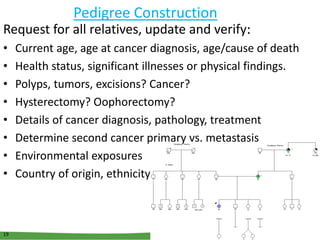
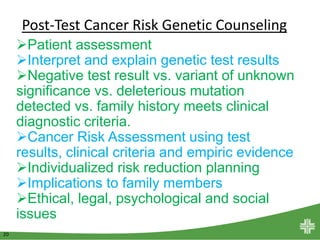
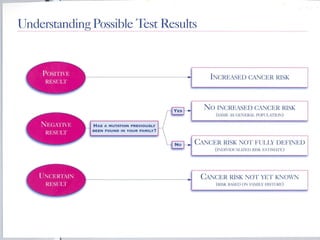
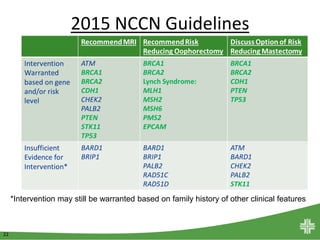
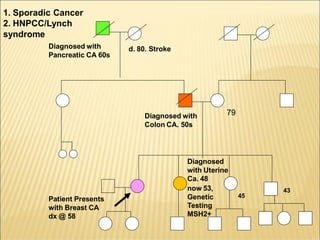
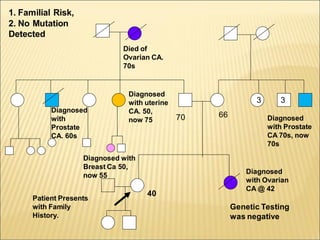
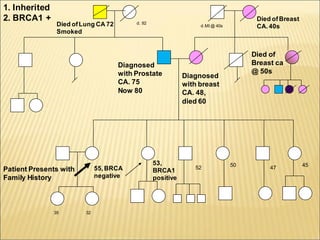
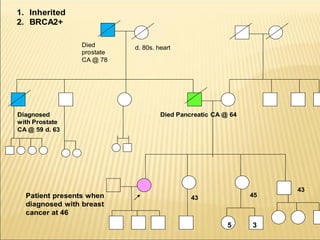
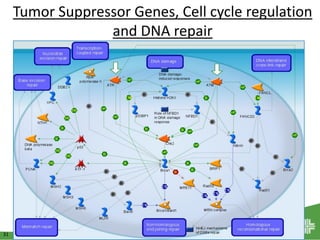
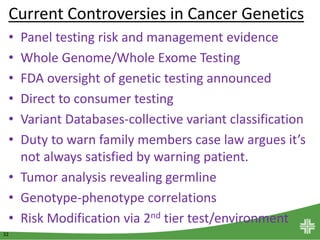
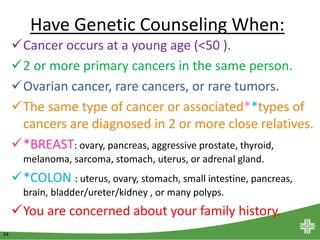
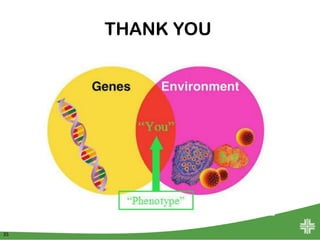
This document discusses genetic counseling for cancer risk assessment. It begins with an introduction to Sandra Brown and her role as manager of the Cancer Genetics Program. It then provides information on various genes associated with cancer risks and how damage to these genes can cause uncontrolled growth and malignant tumors. The rest of the document discusses the differences between sporadic, familial, and inherited cancers; the process of genetic counseling before and after genetic testing; recommendations for who should receive genetic counseling; challenges like interpreting results and informing family; and current issues and controversies in cancer genetics.