Embed presentation
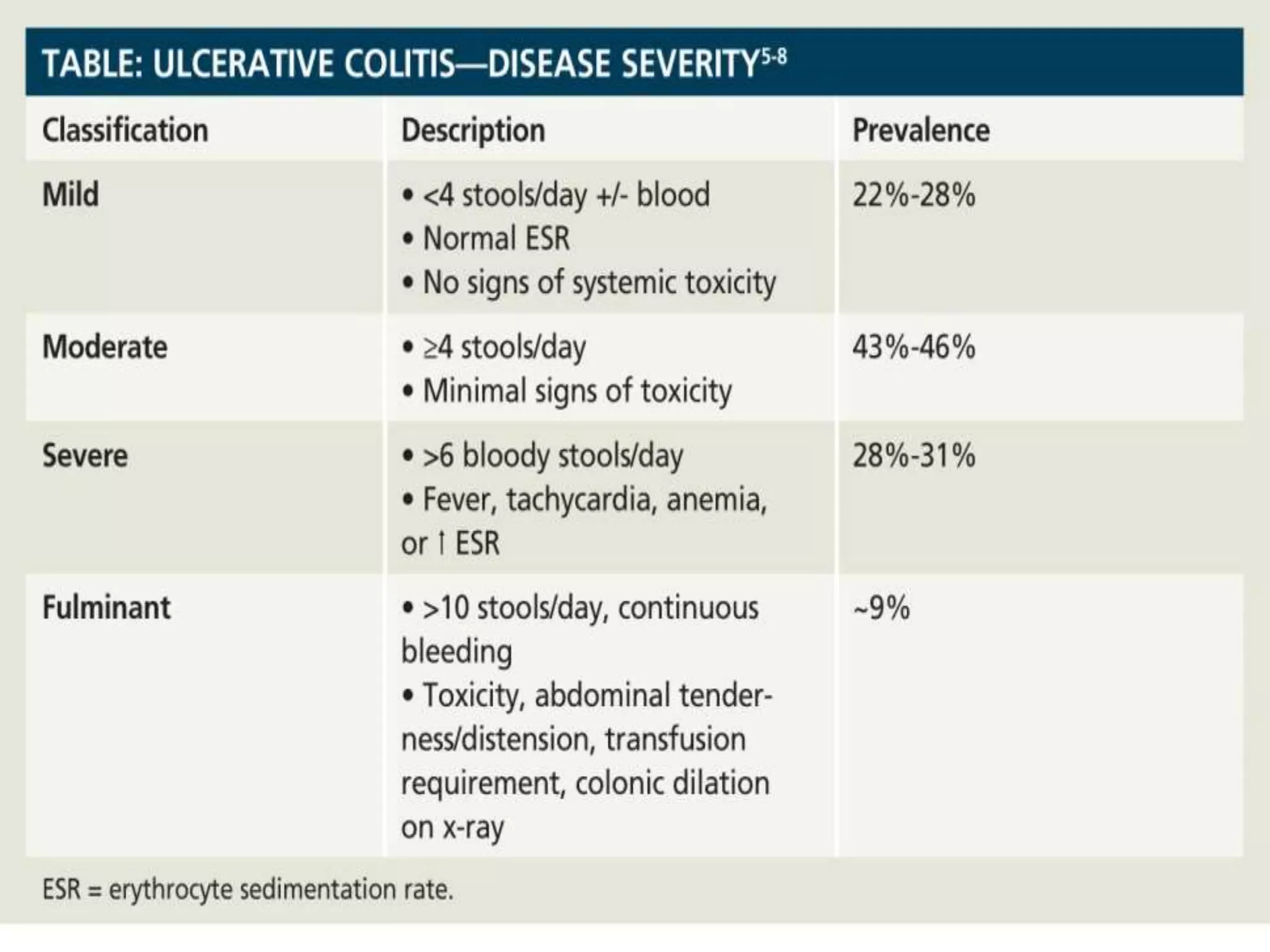
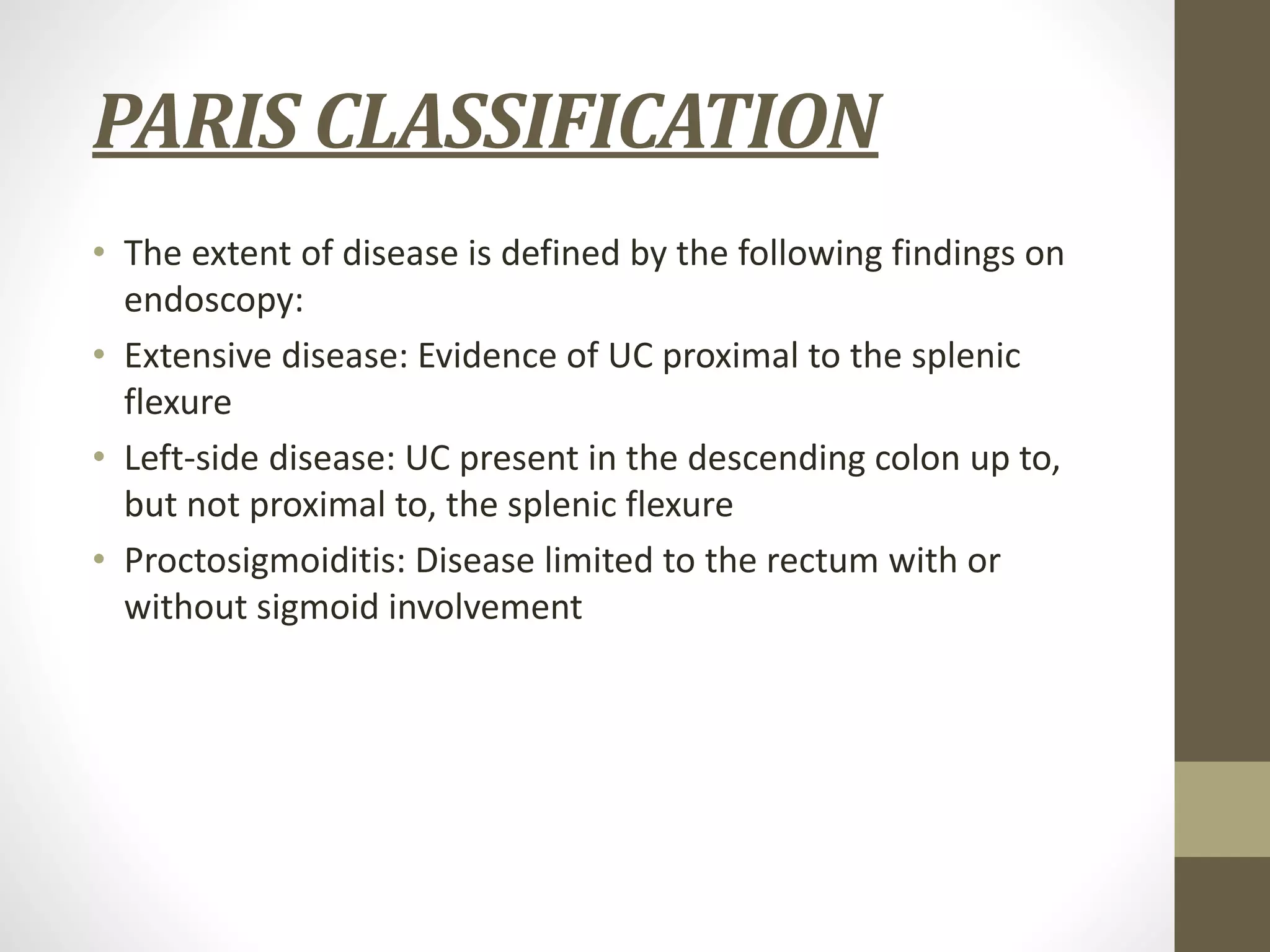
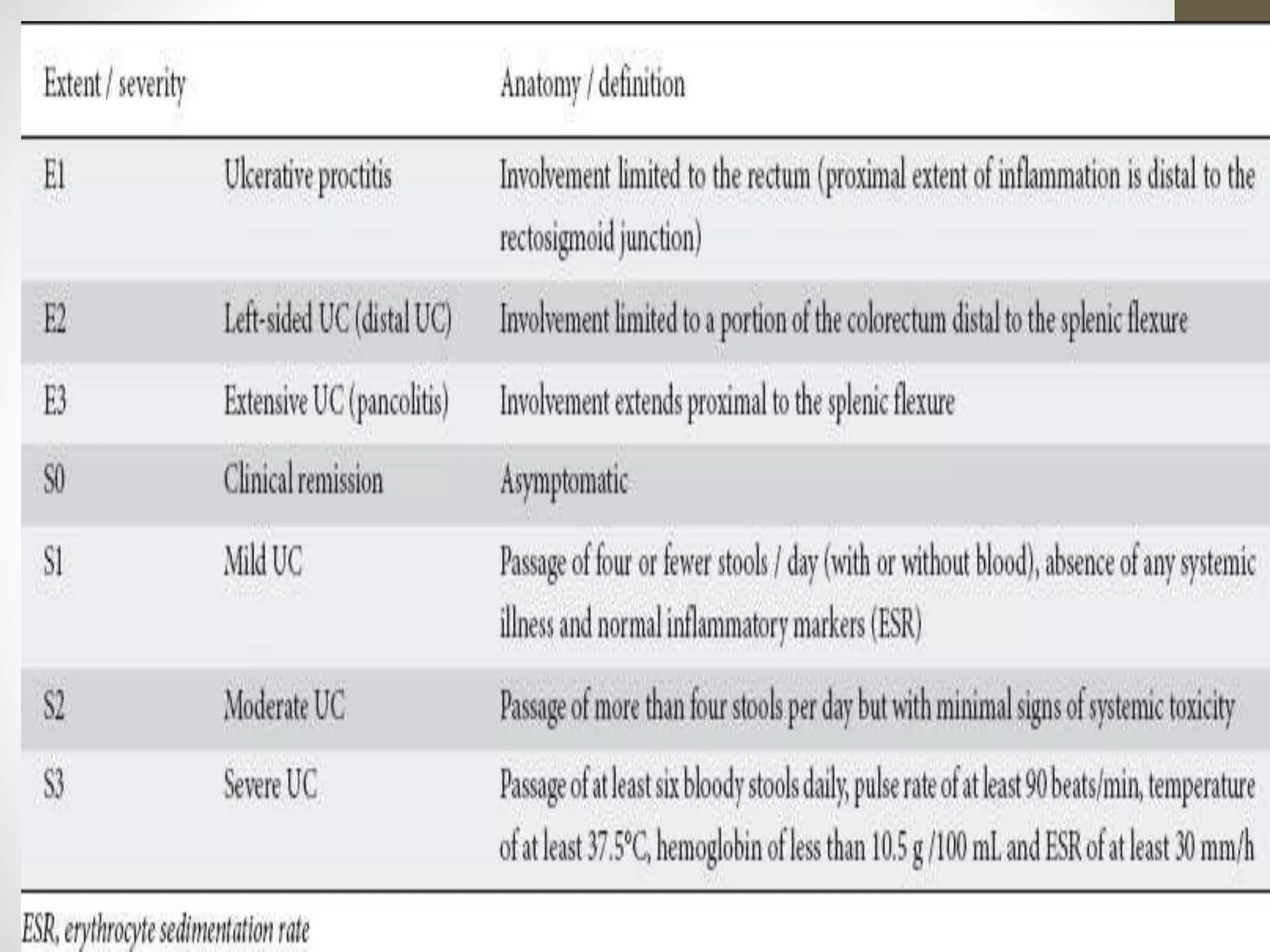
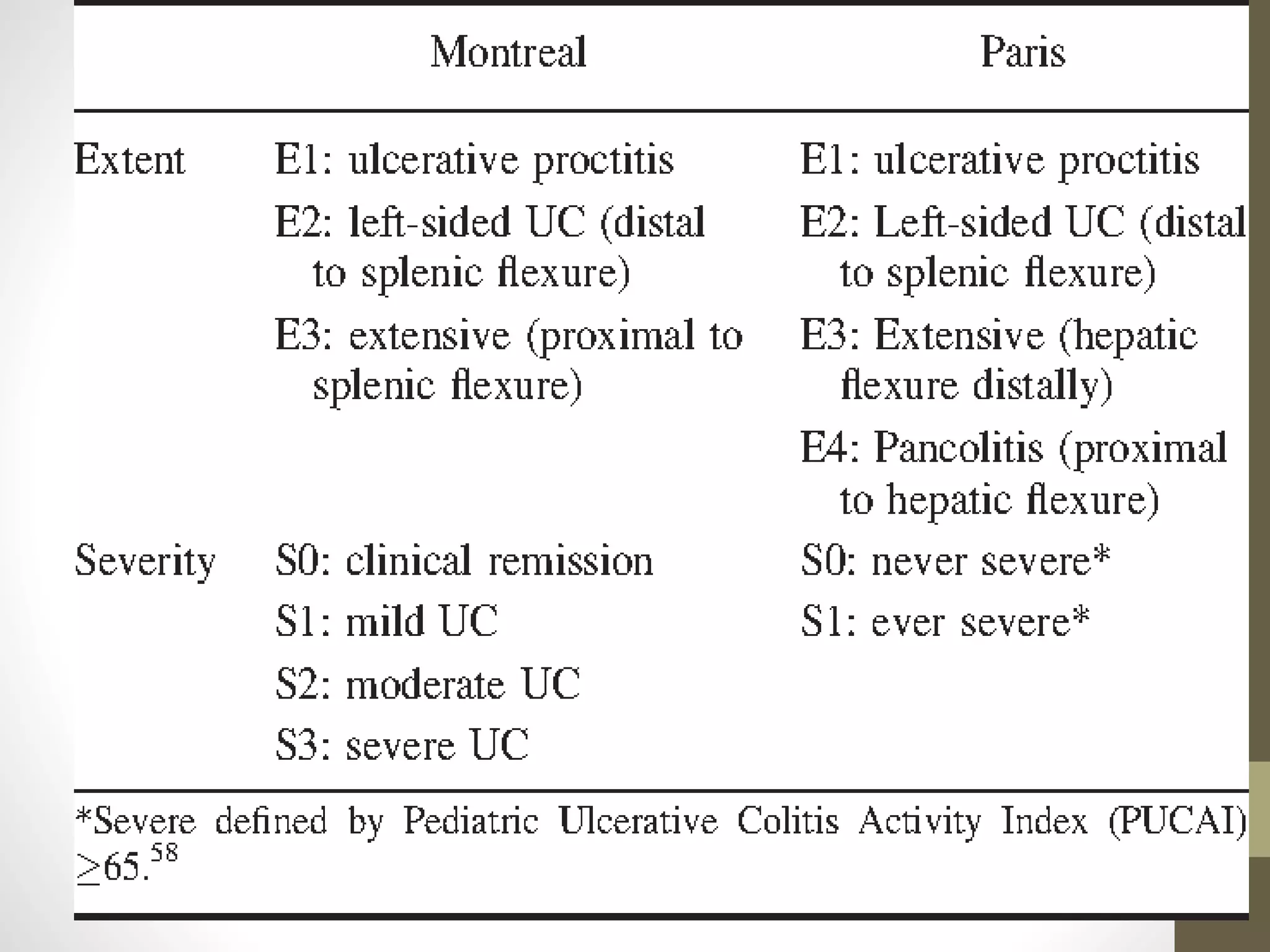
Download to read offline
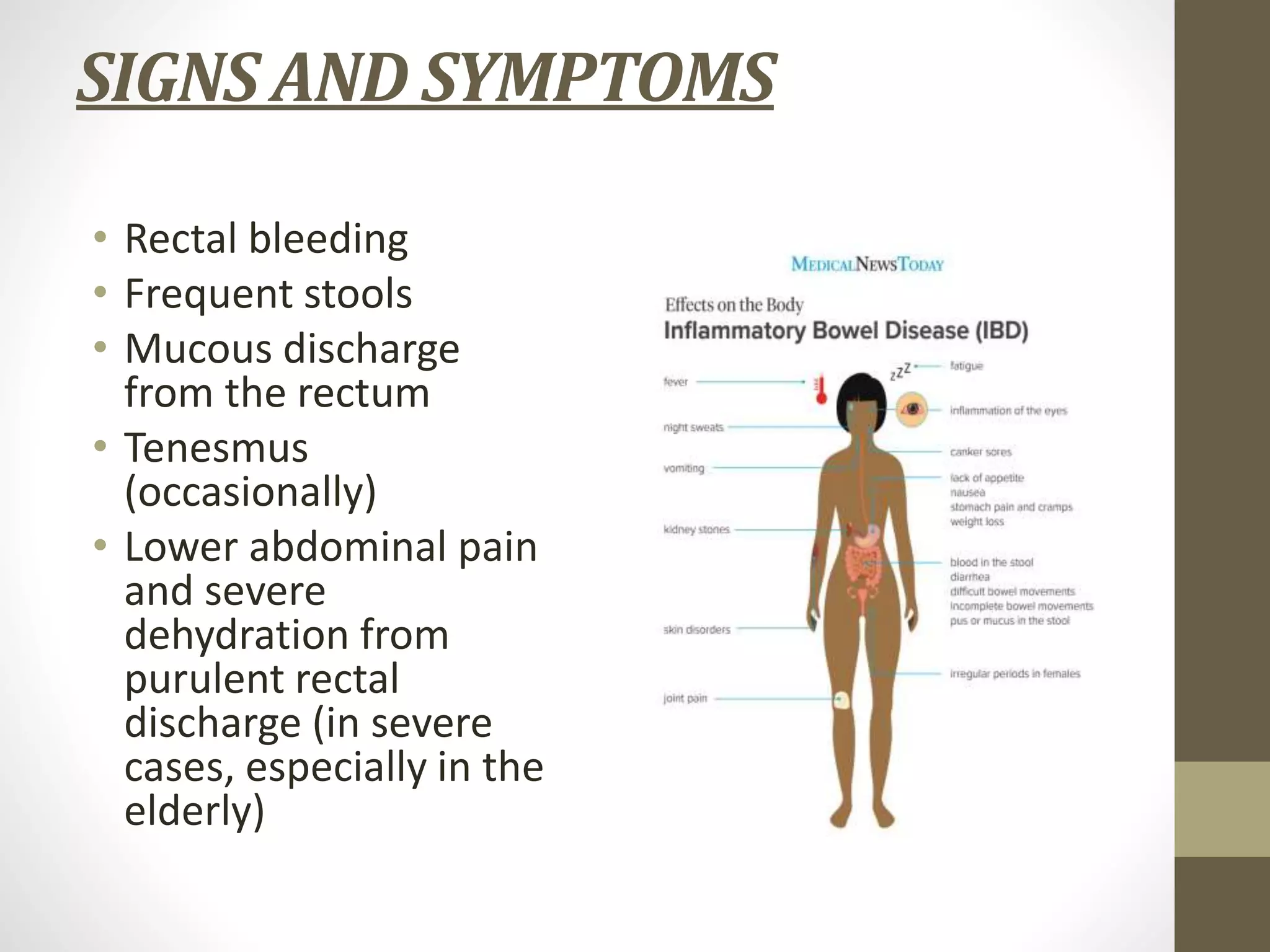
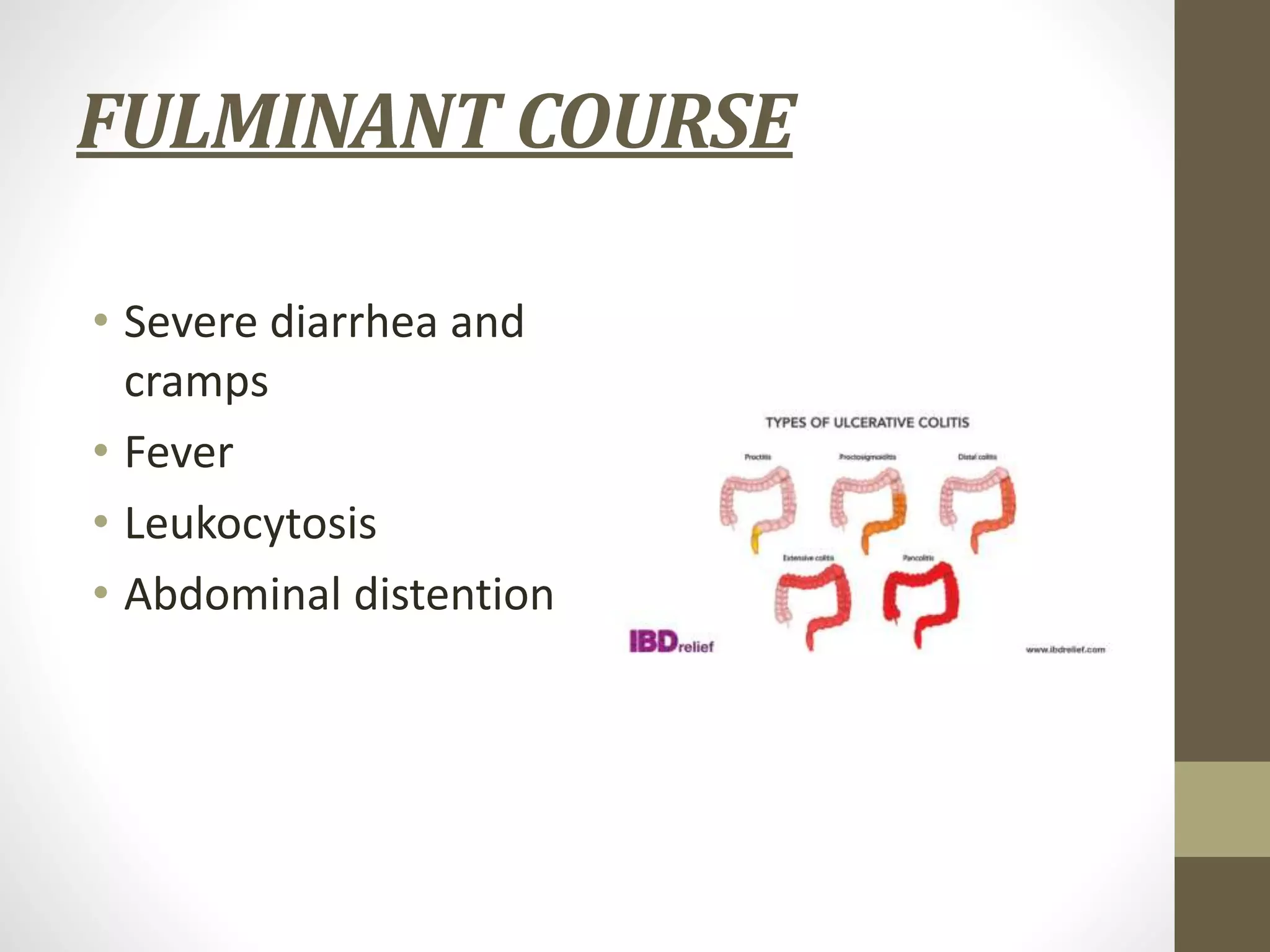
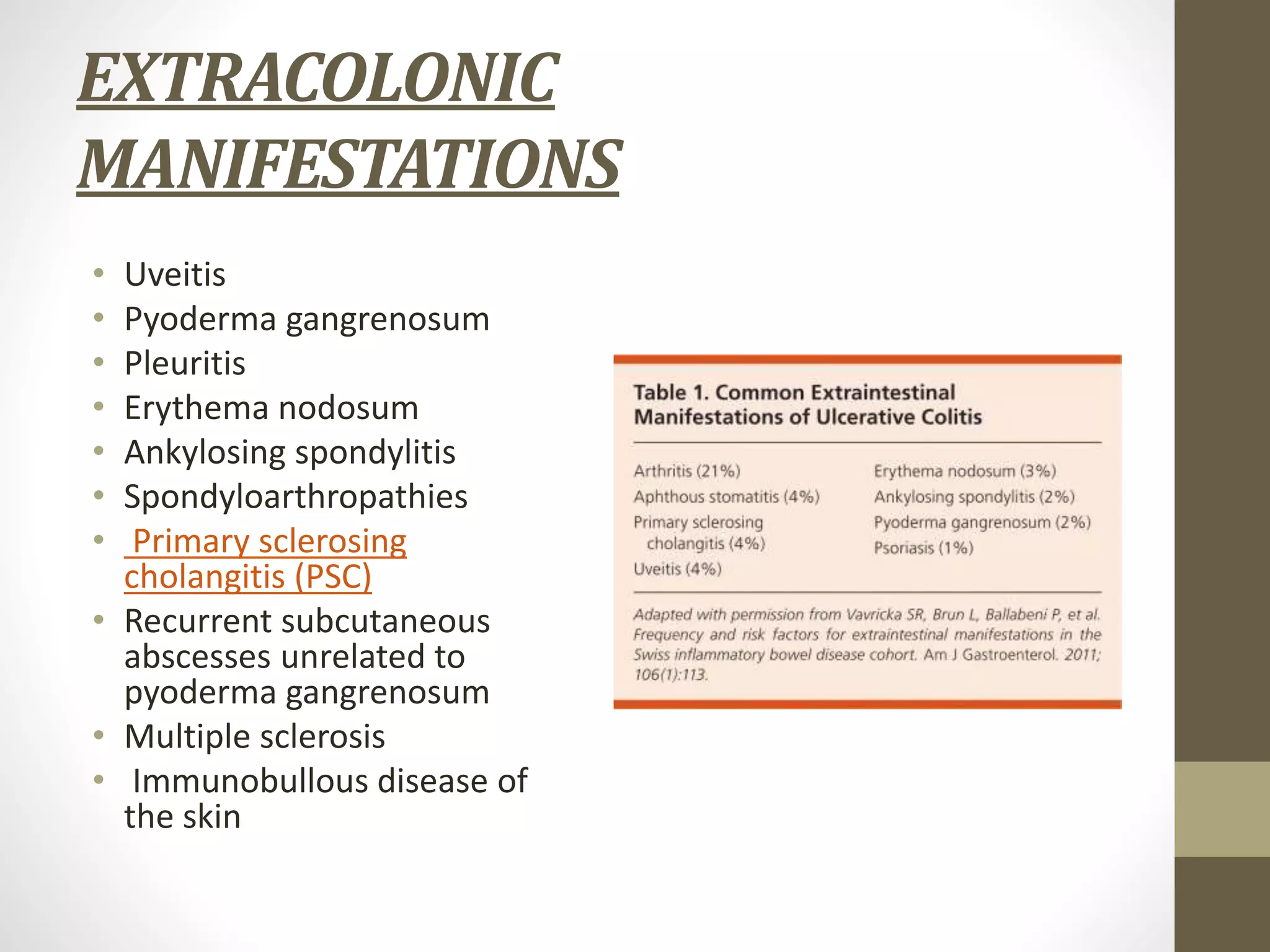
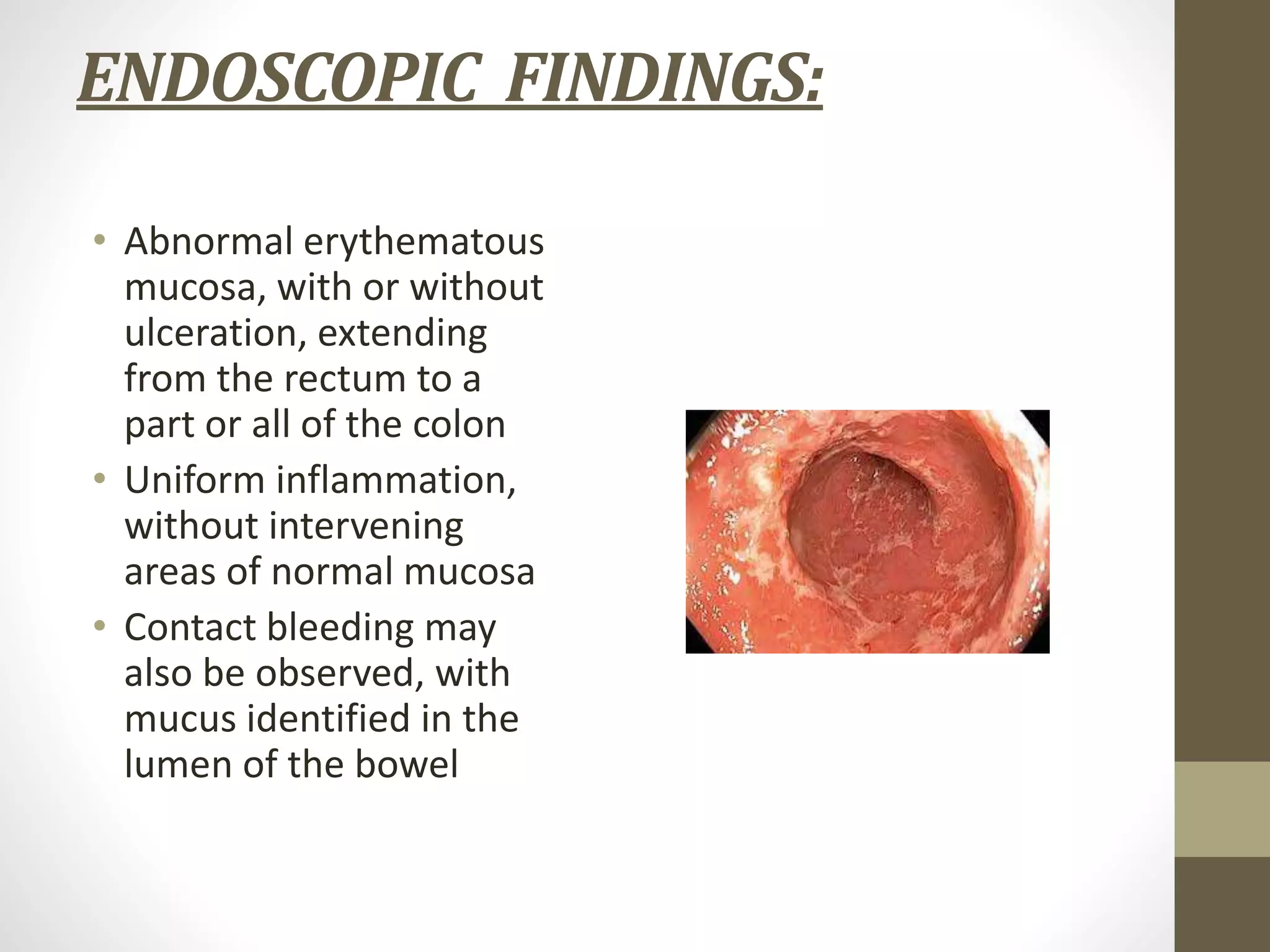
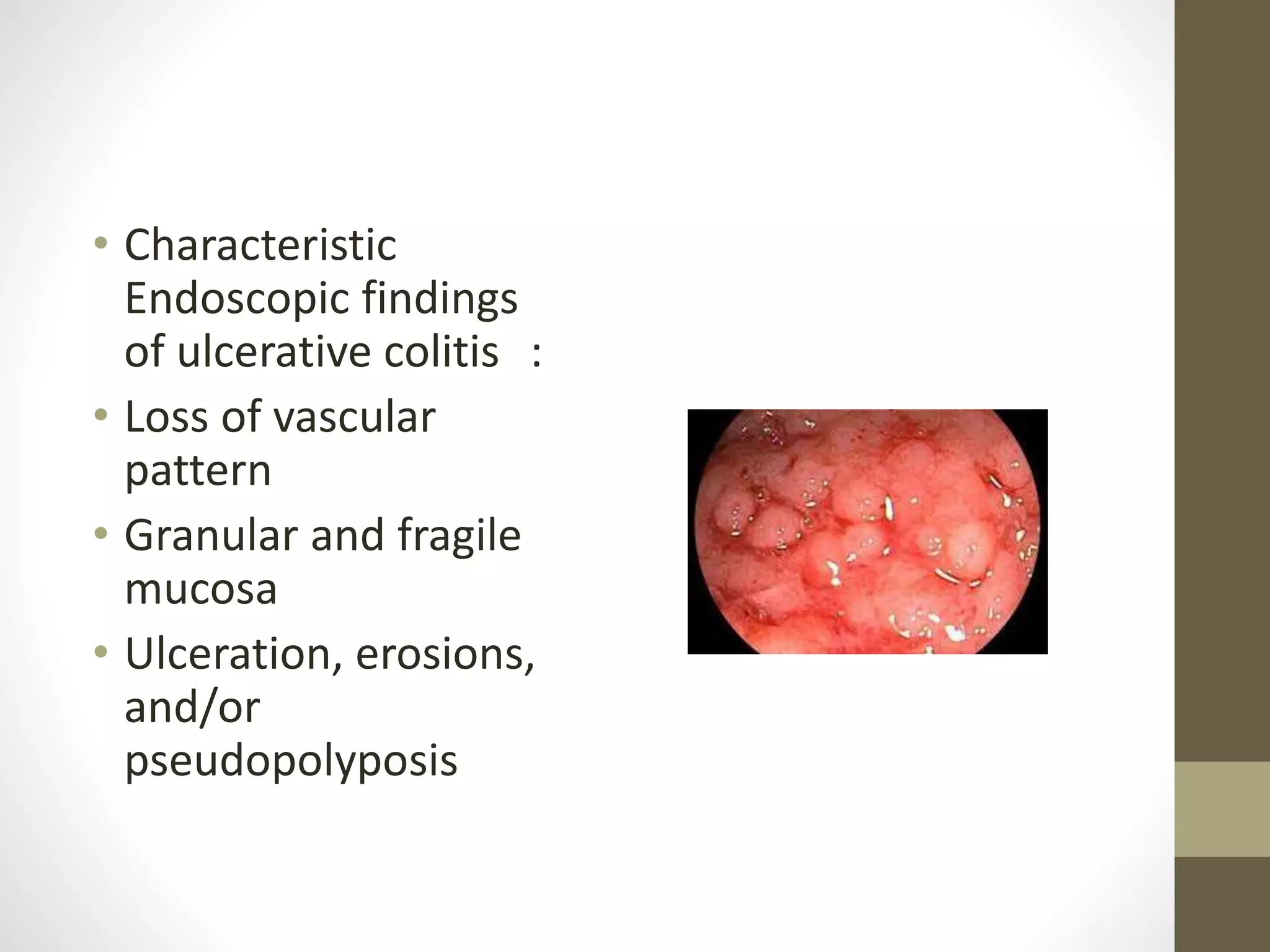
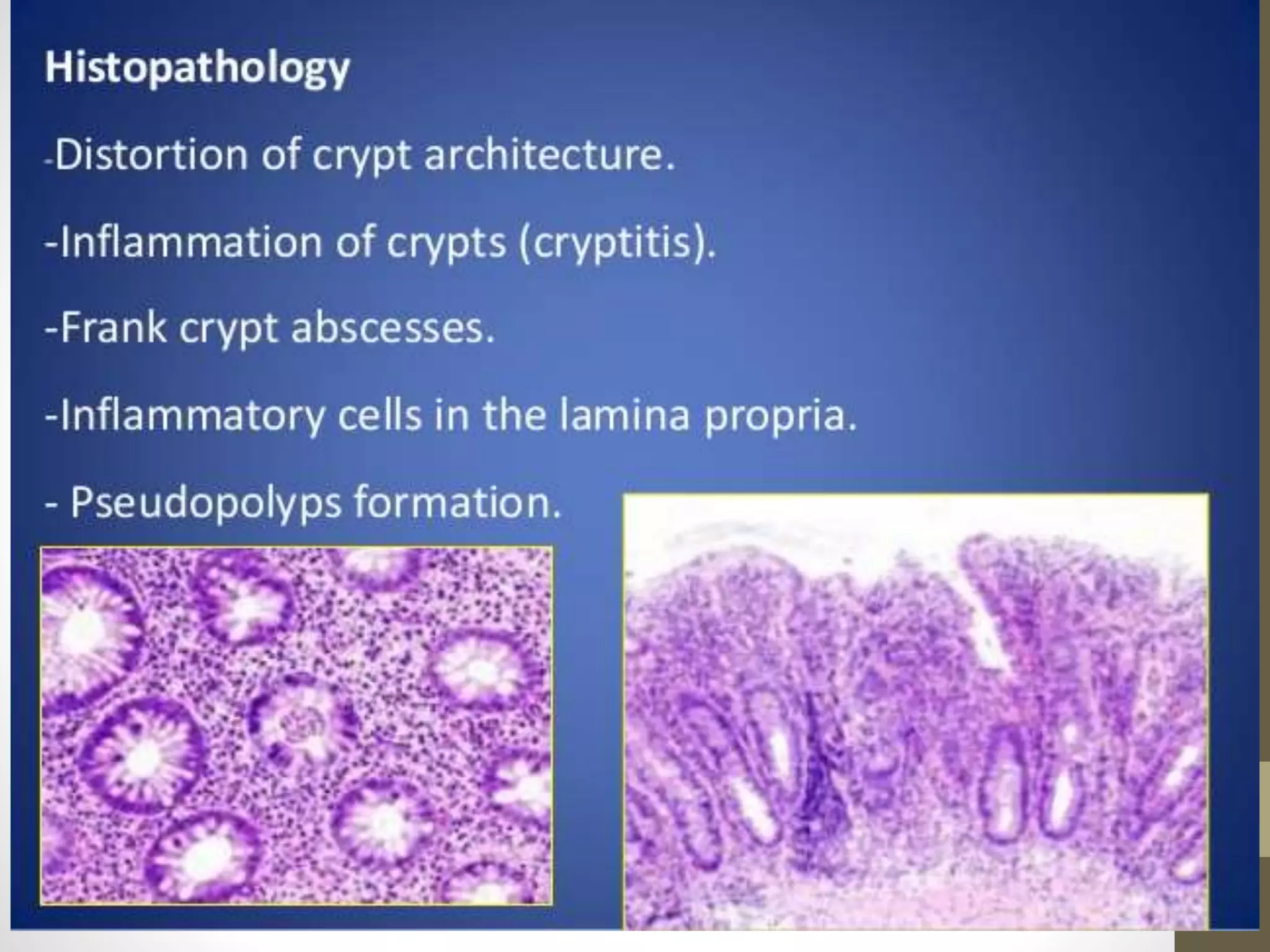
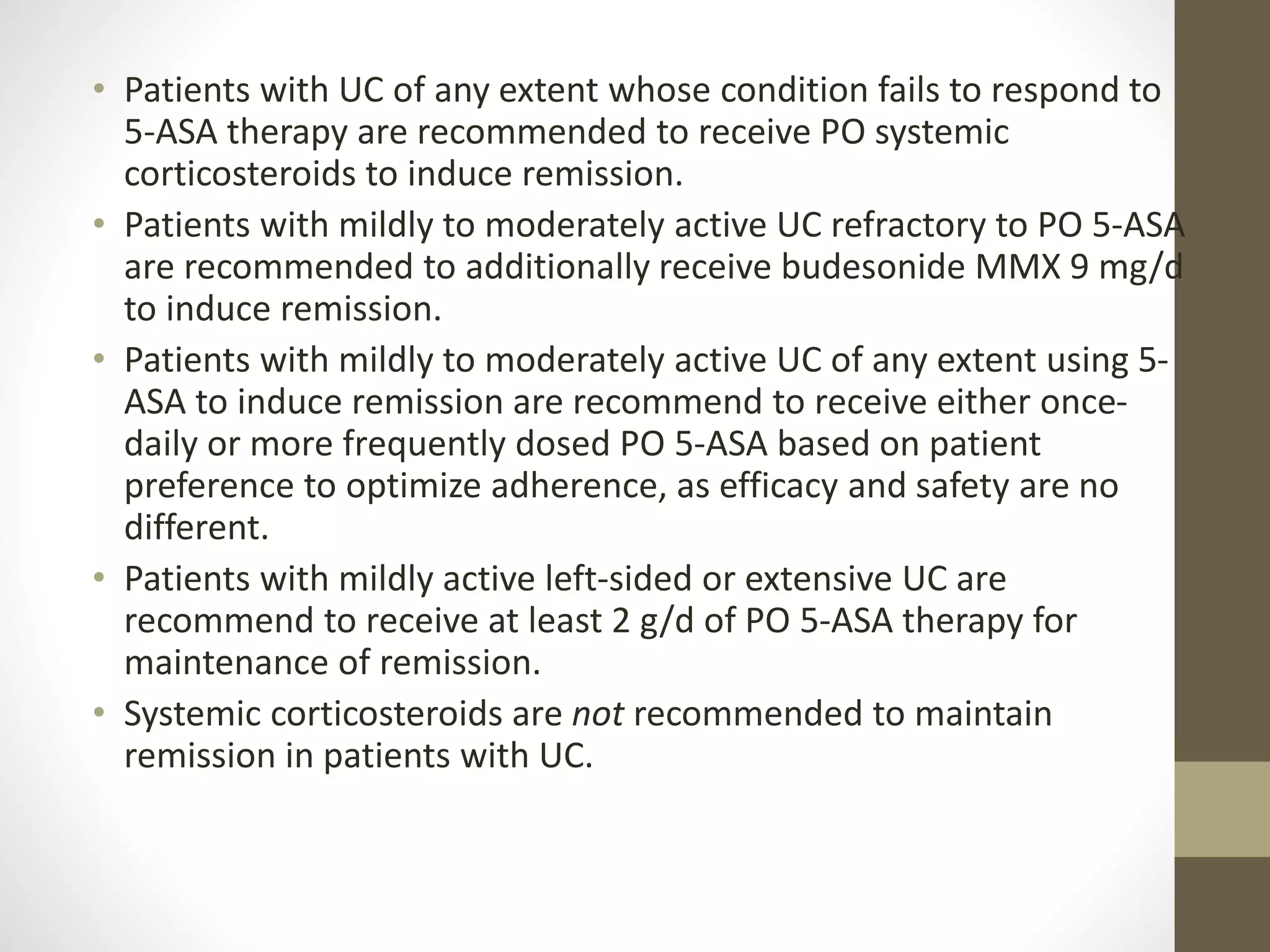
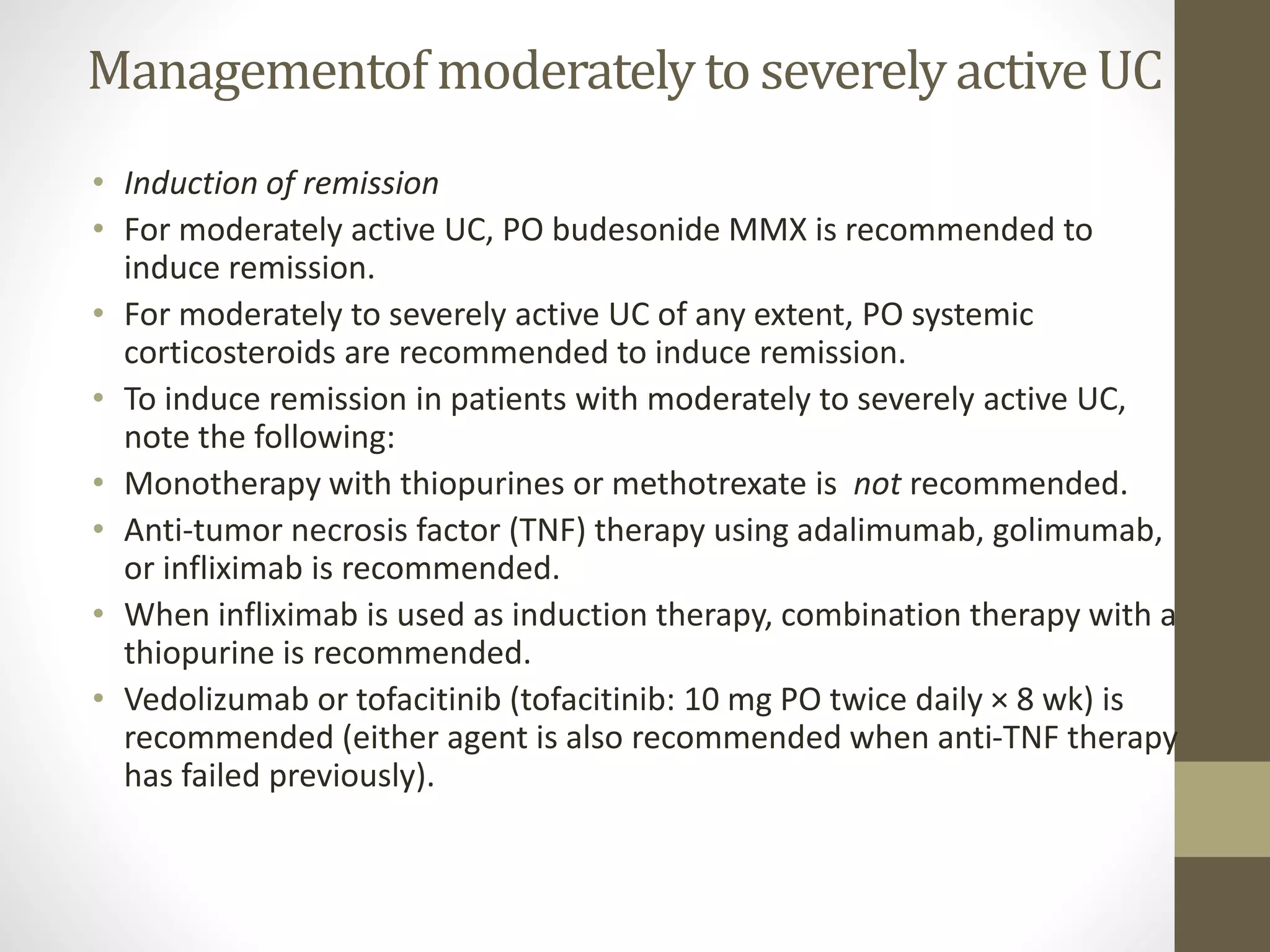
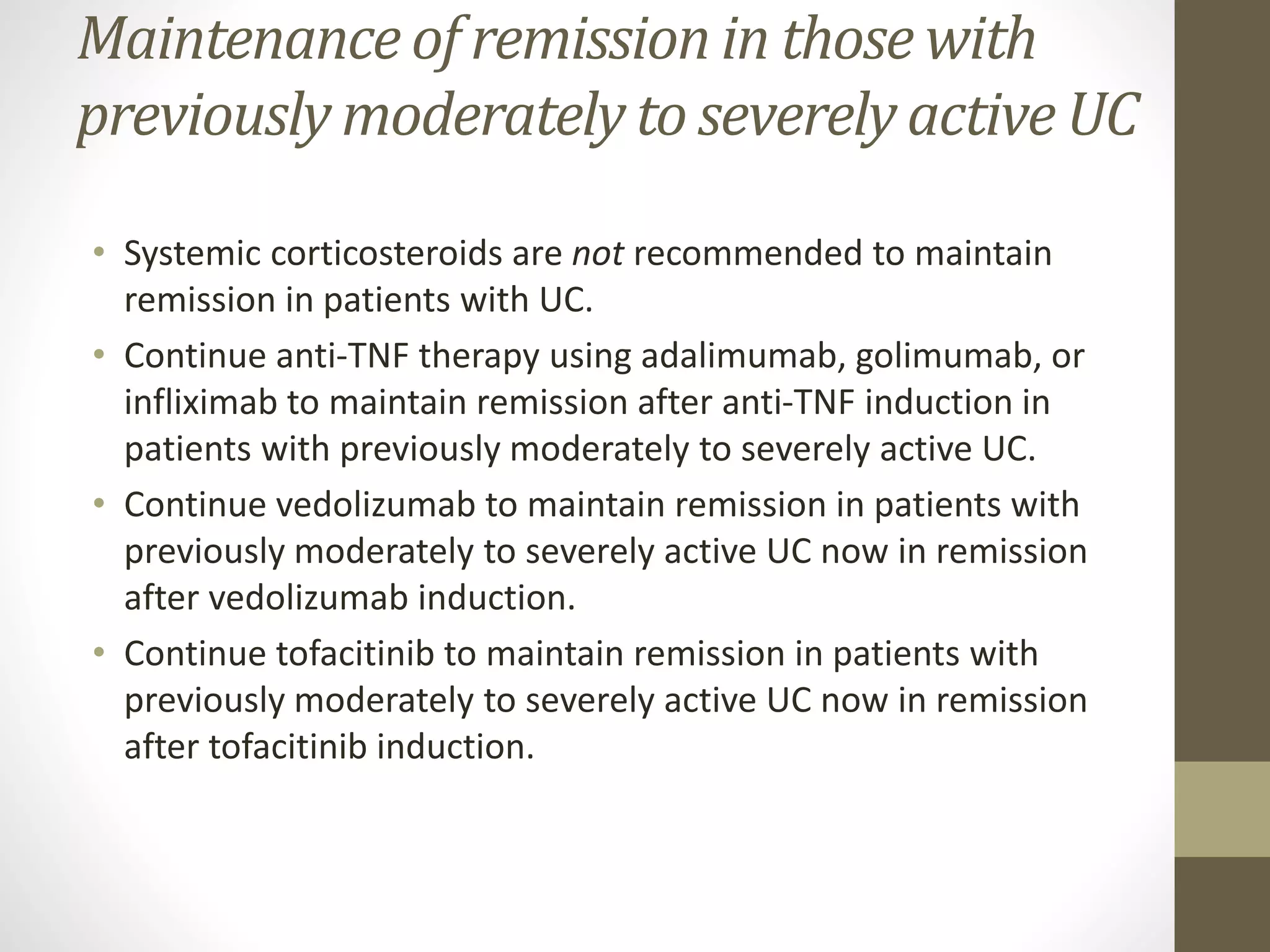
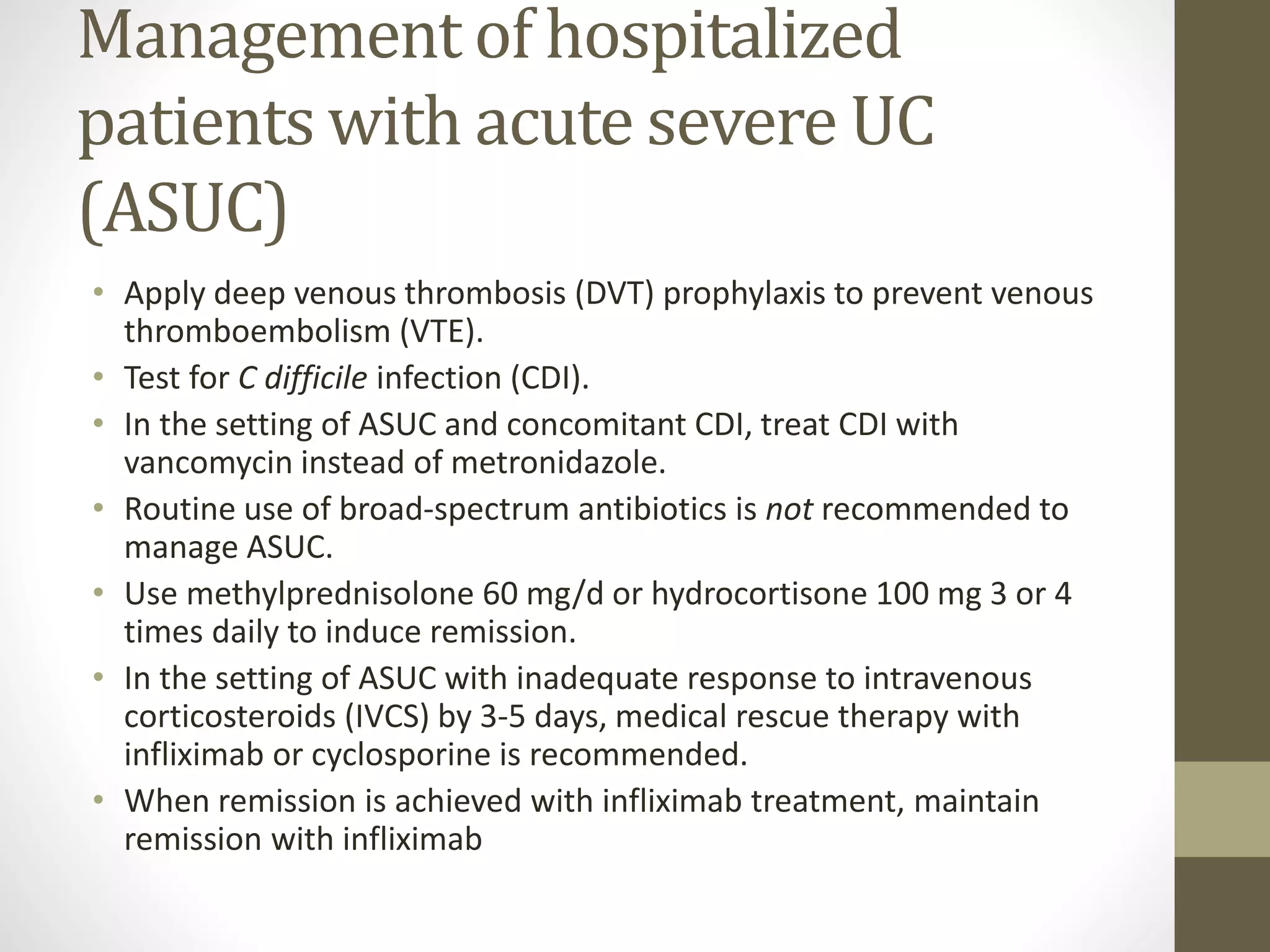

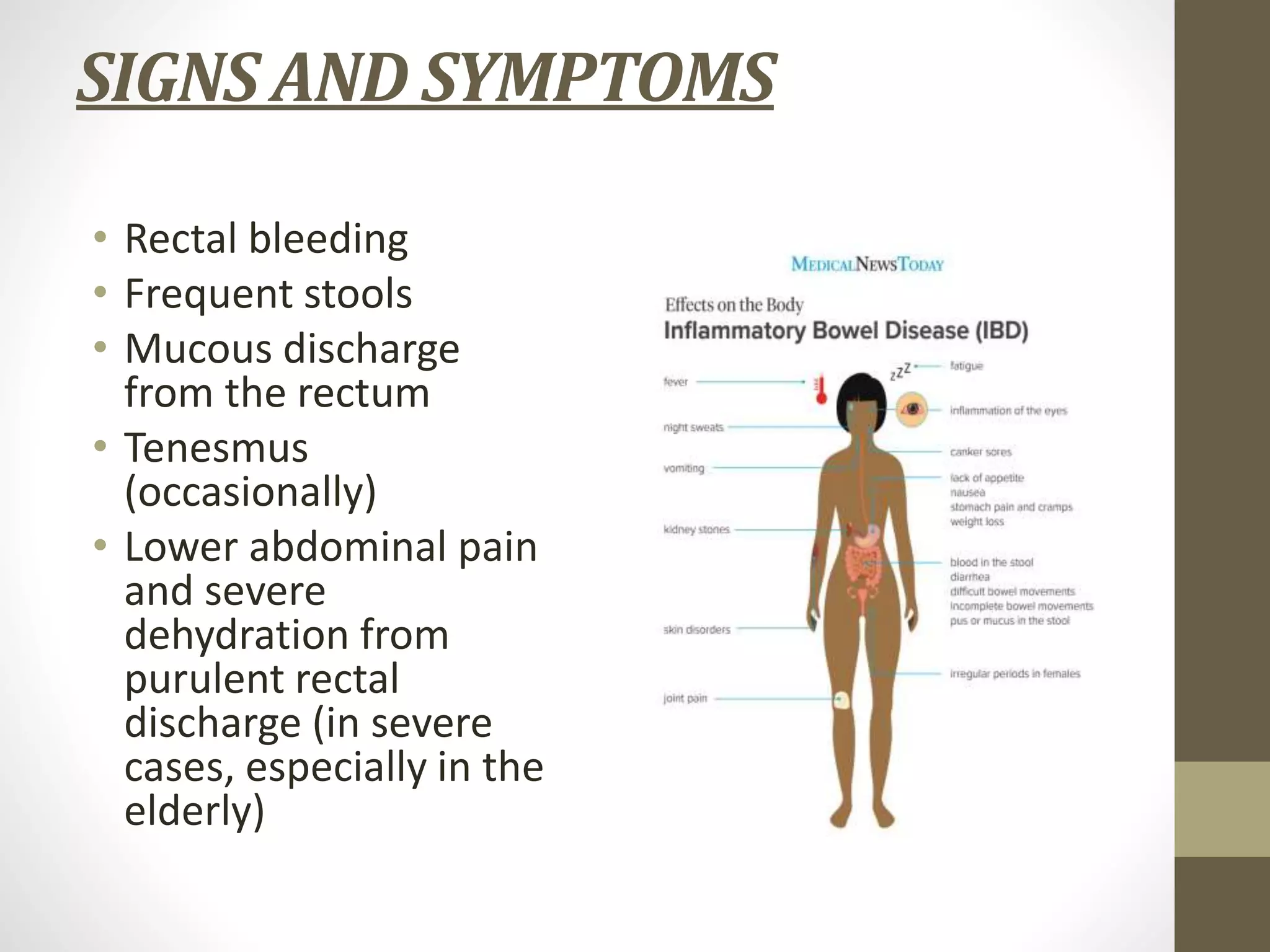
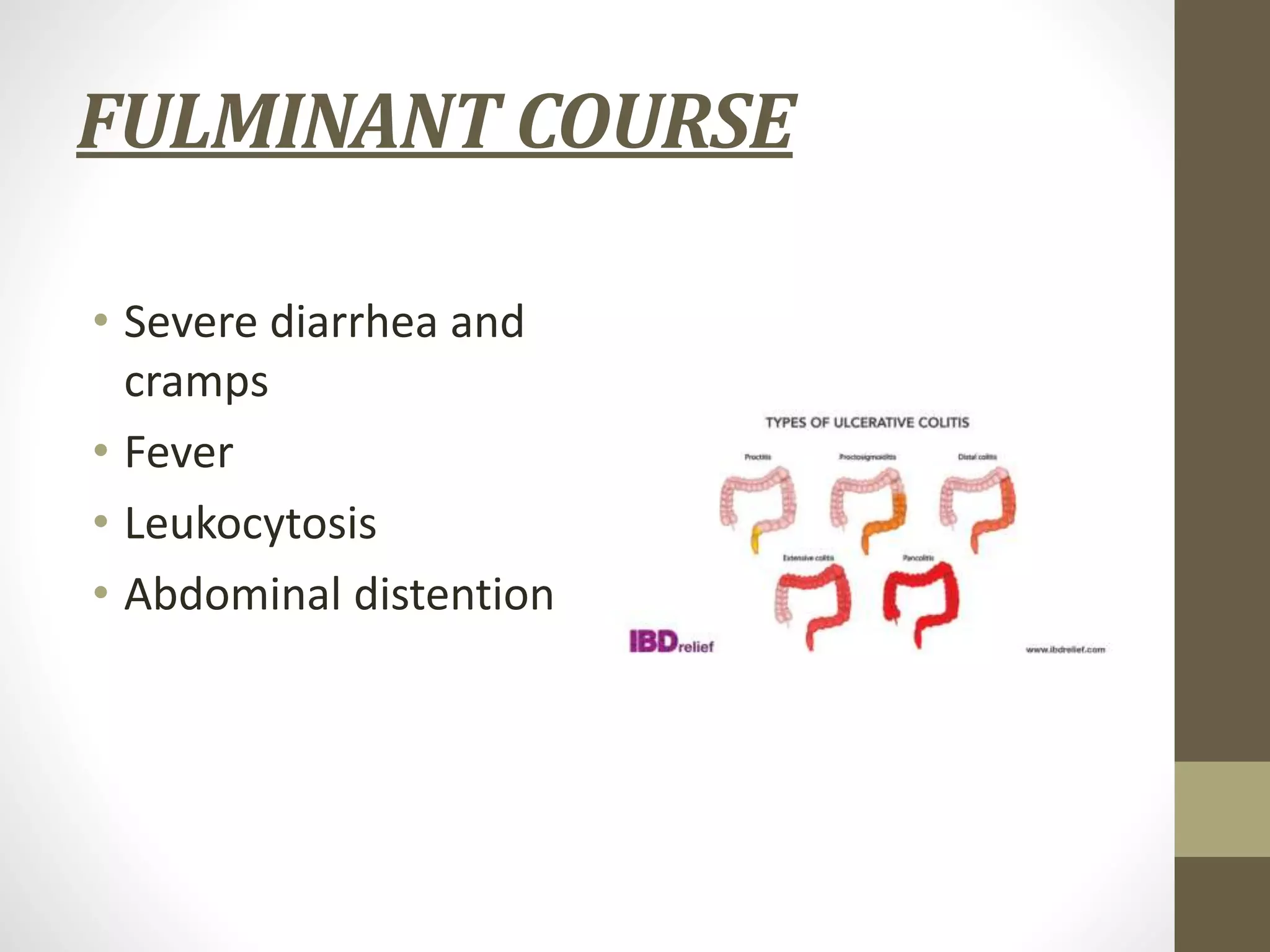
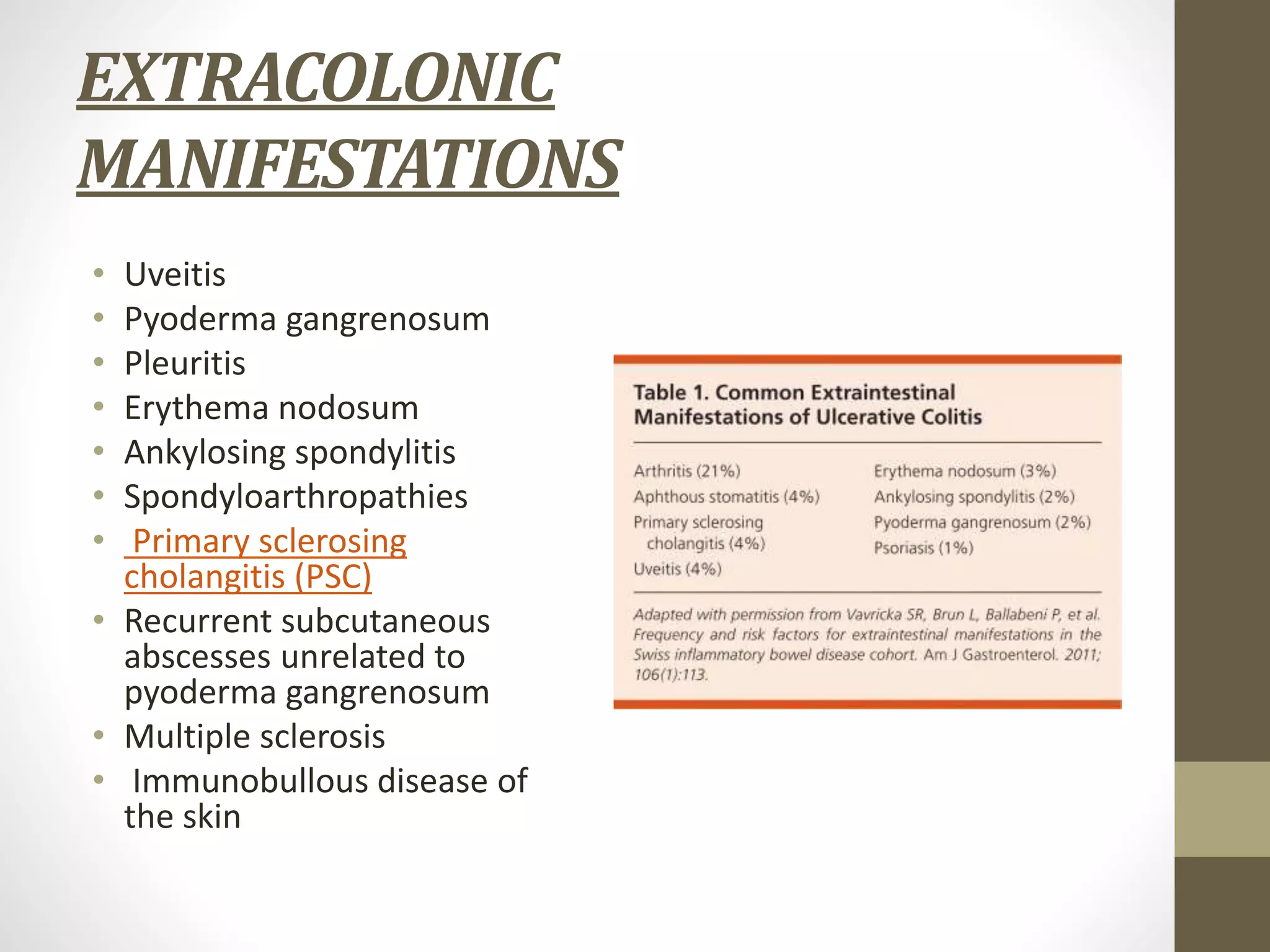
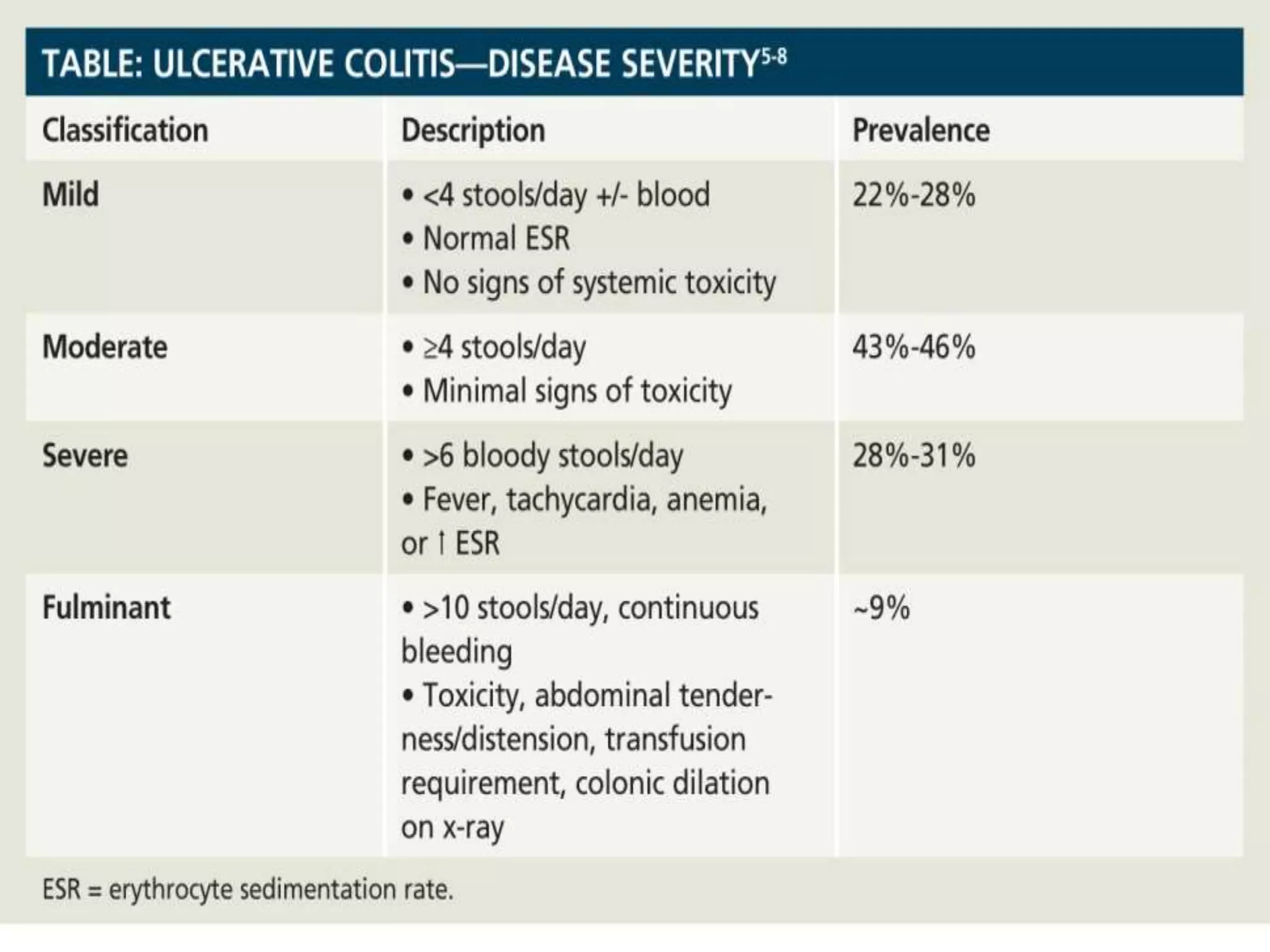
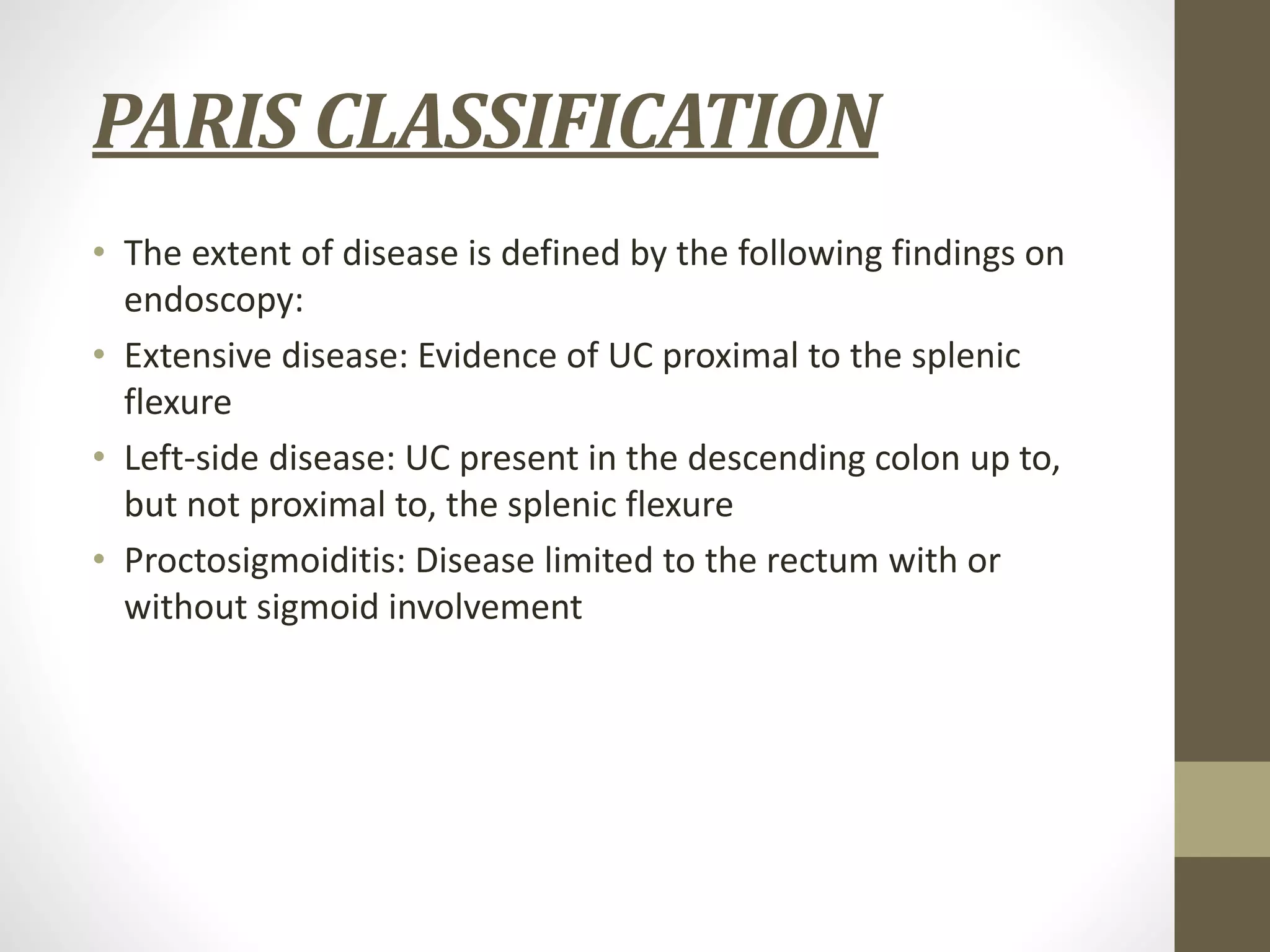
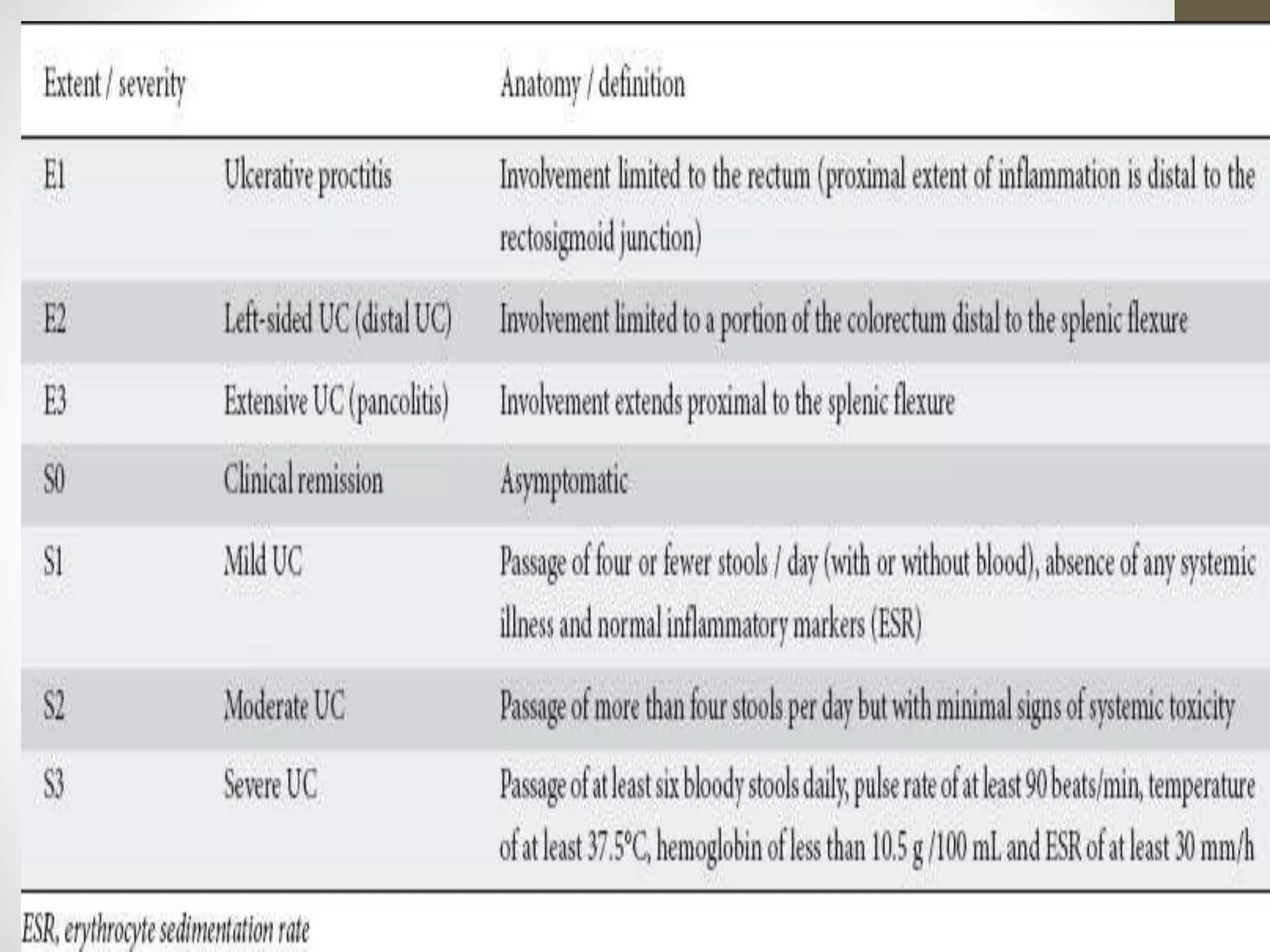
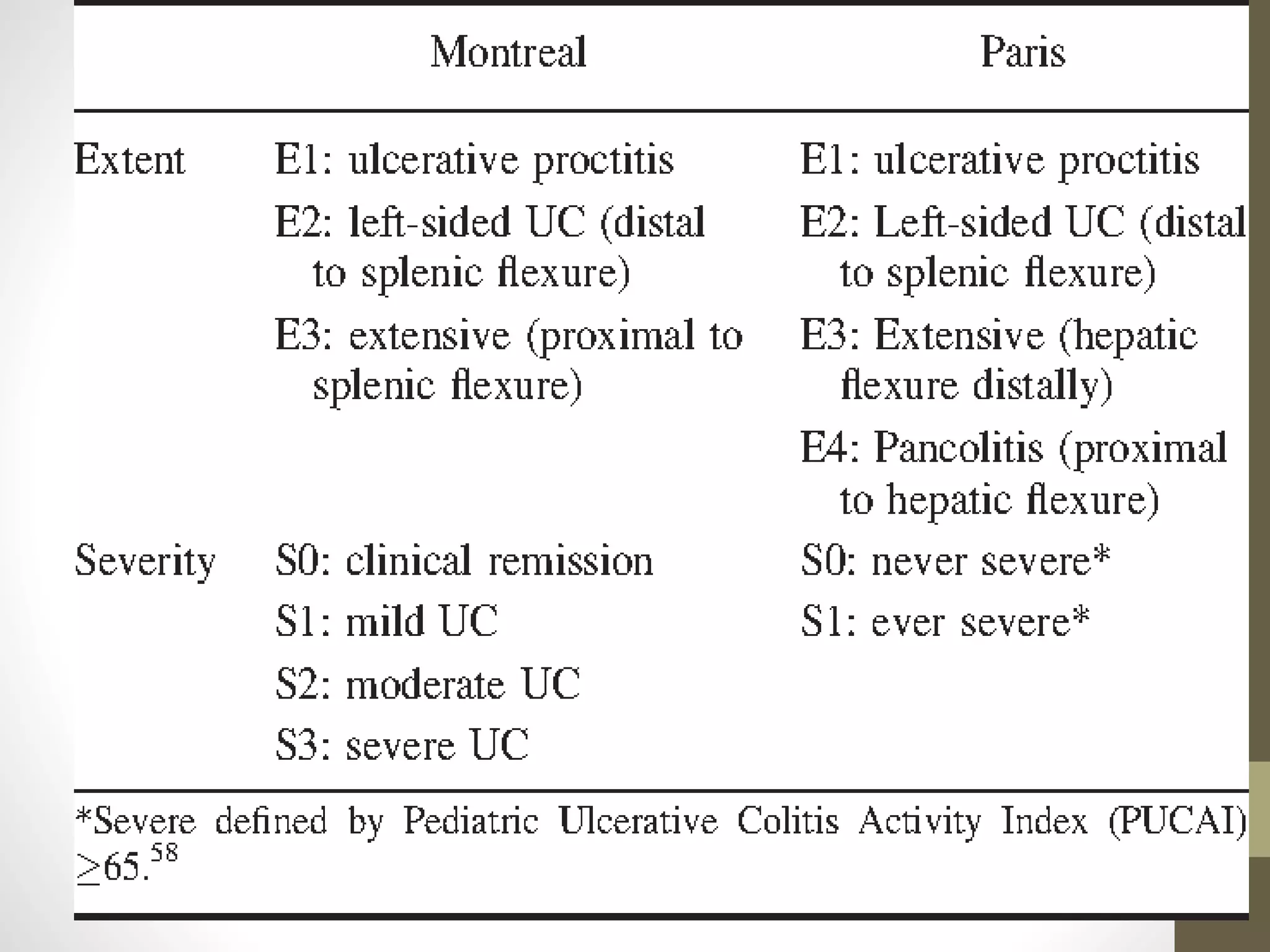
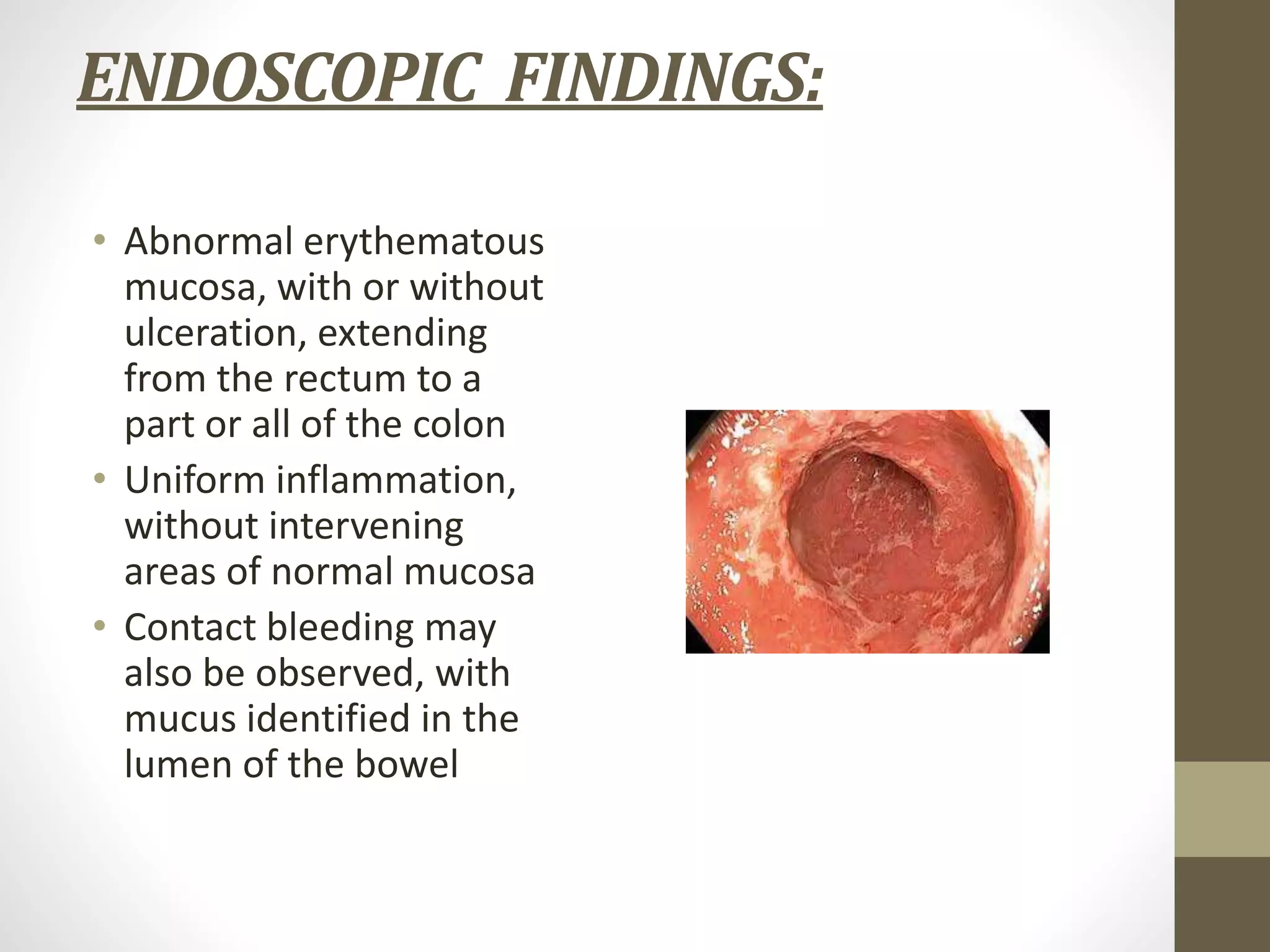
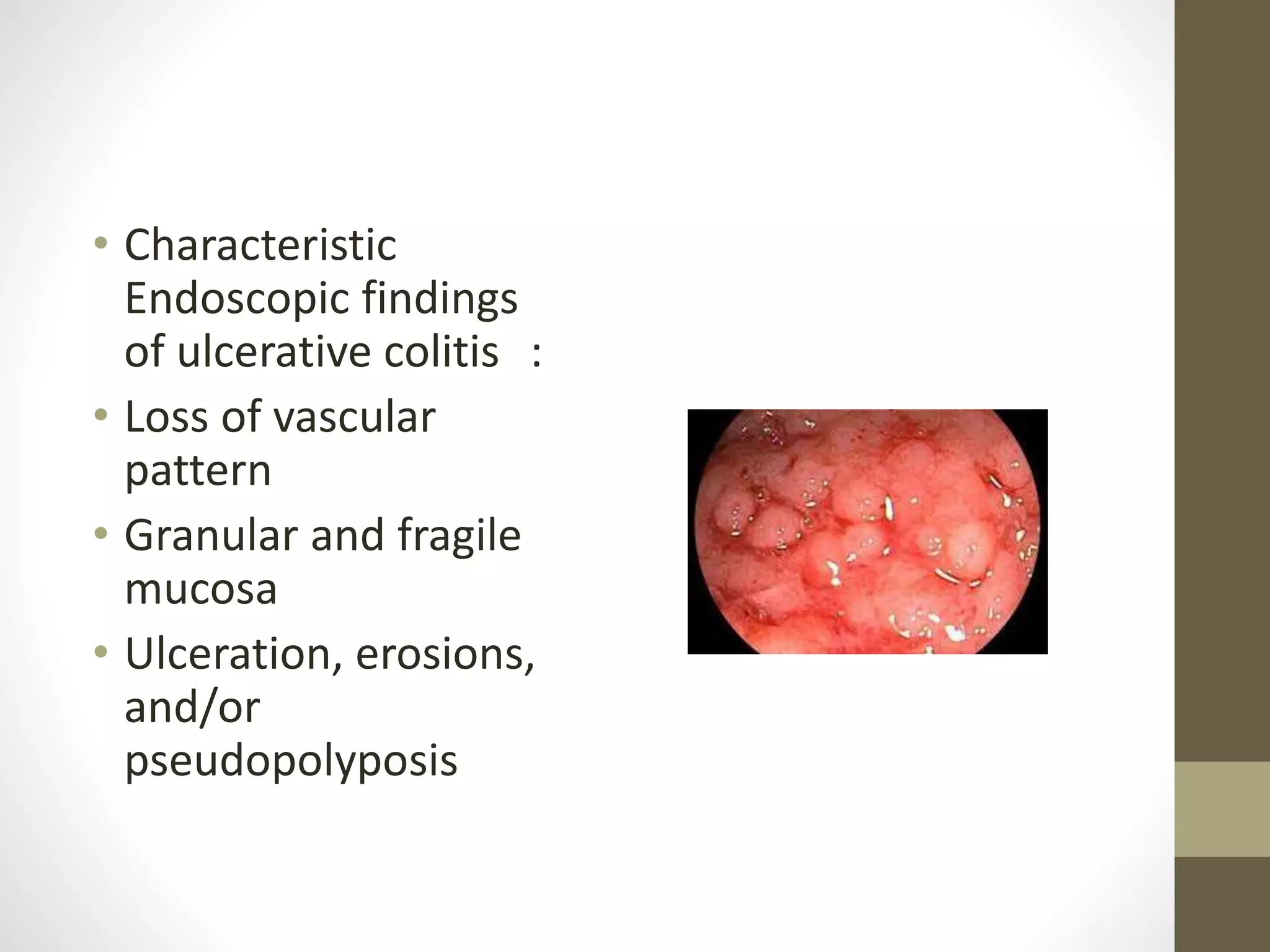
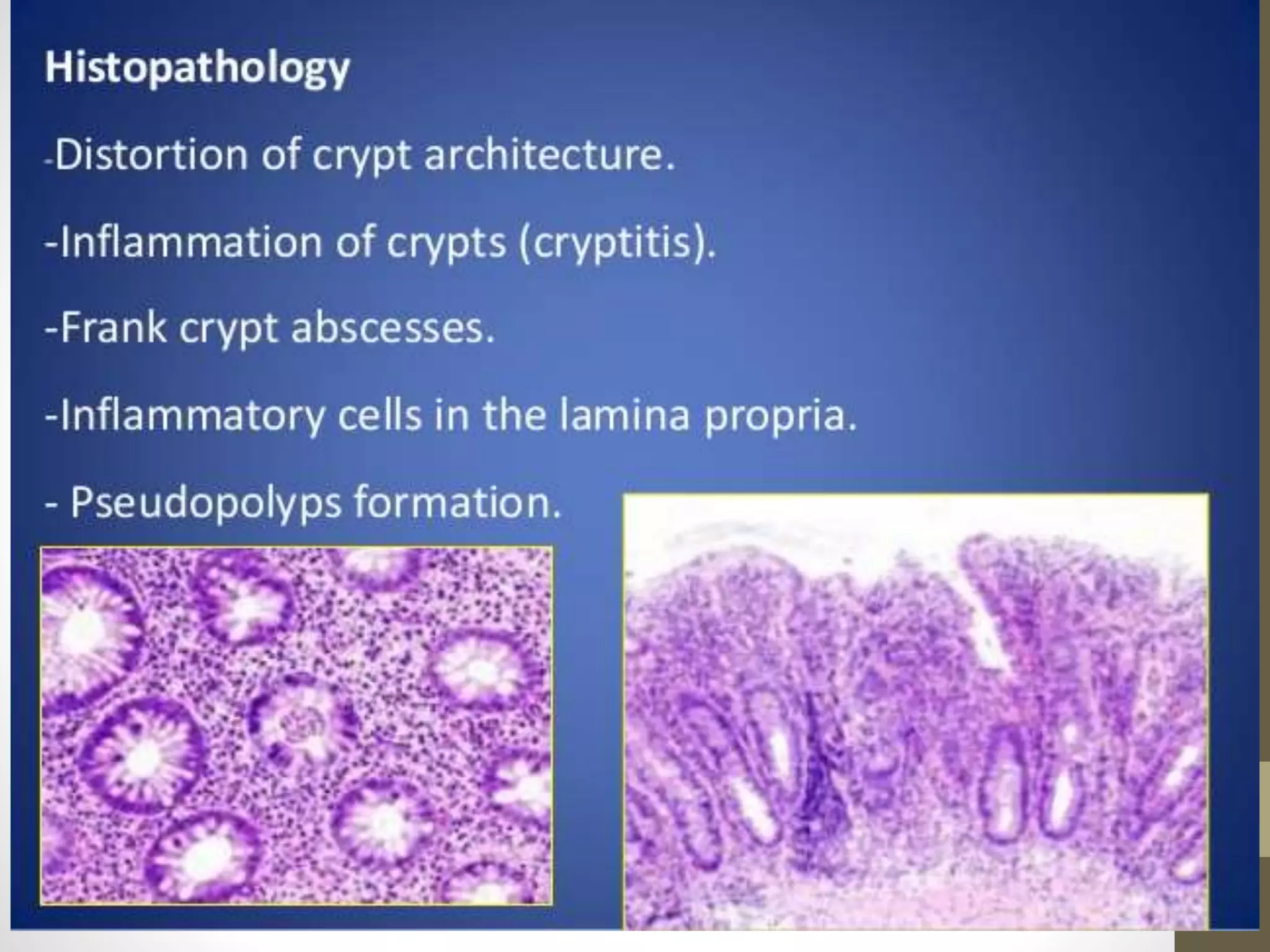
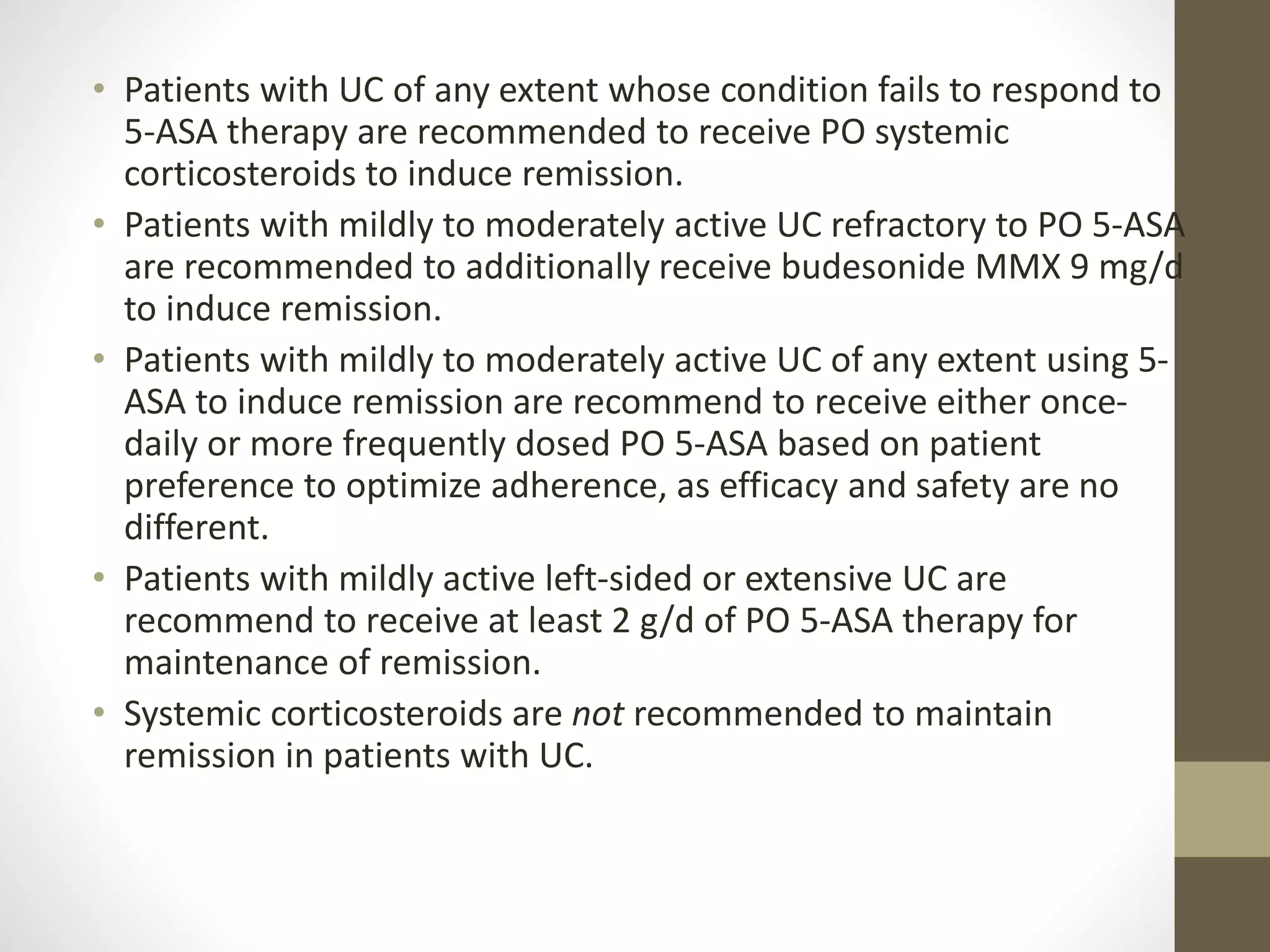
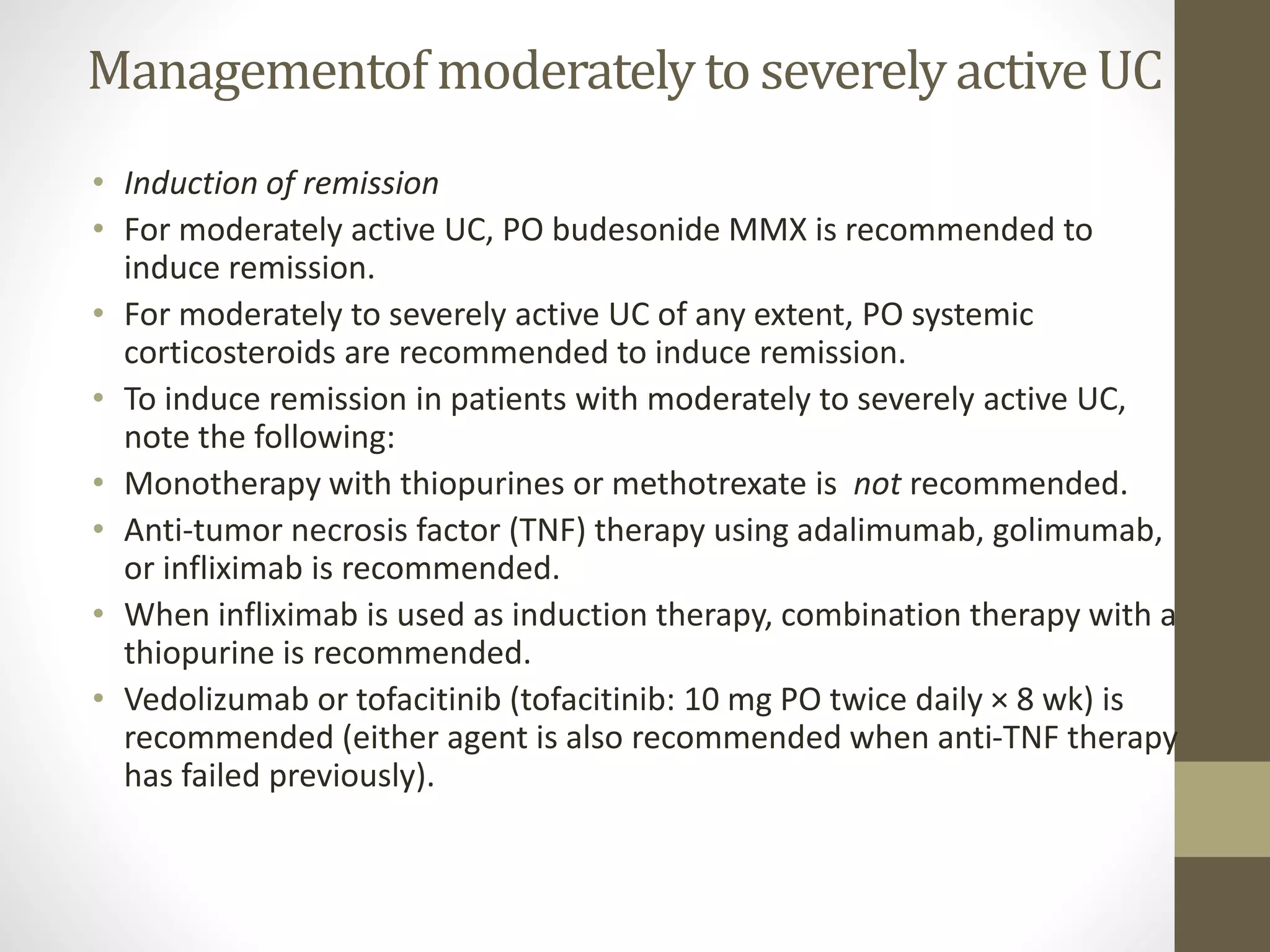
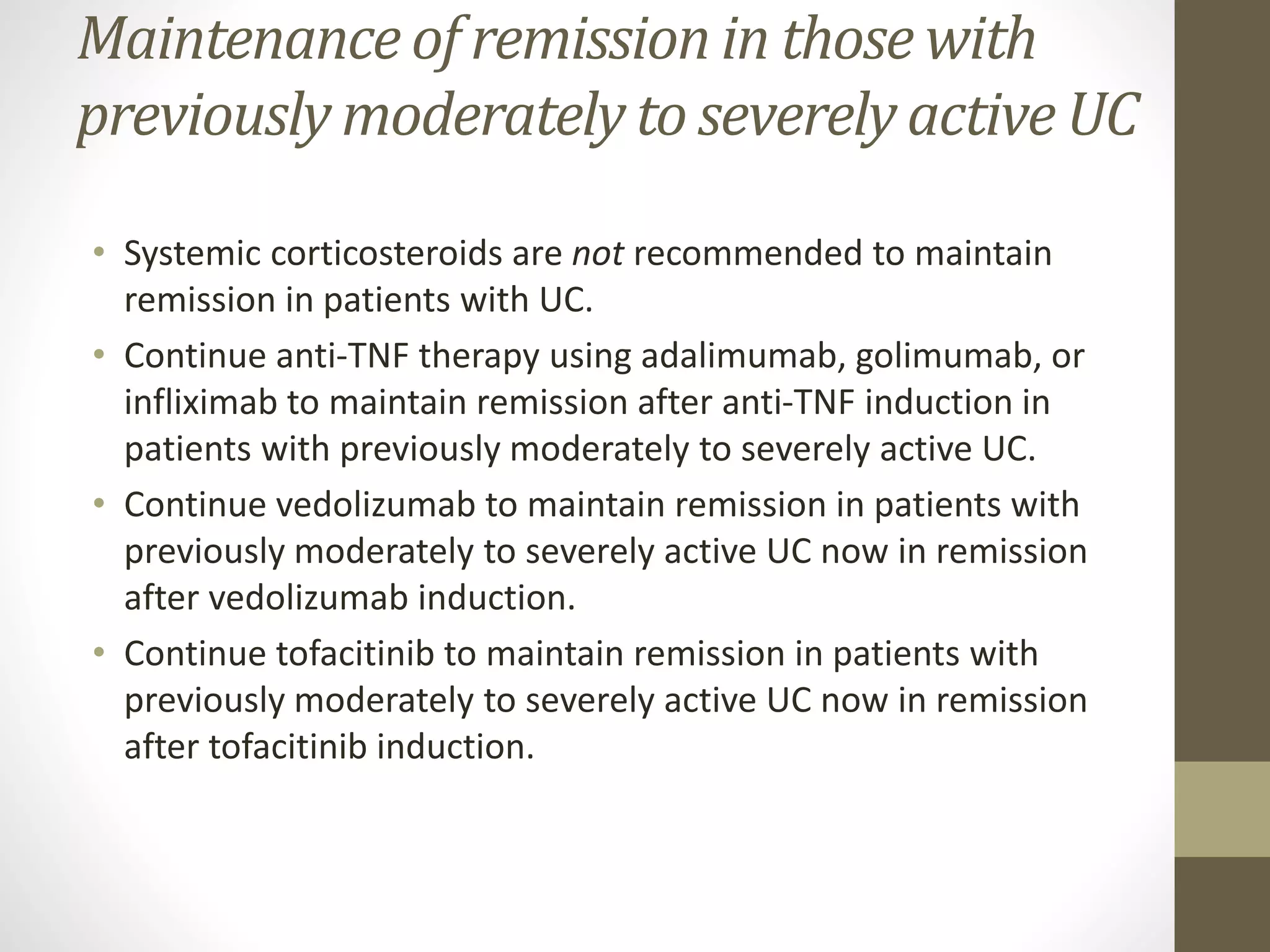
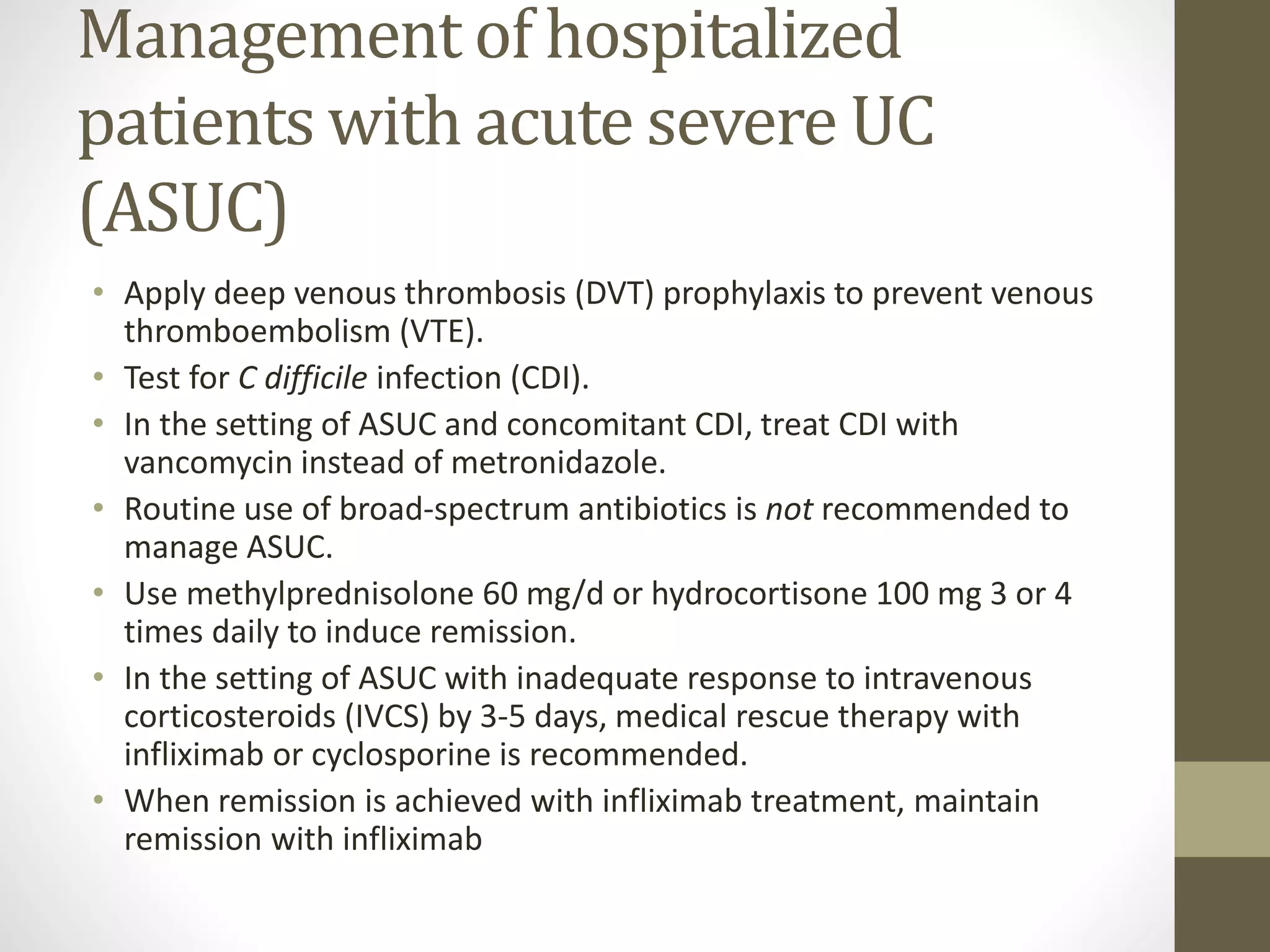
Ulcerative colitis is a type of inflammatory bowel disease that affects the large intestine. It is characterized by inflammation and ulcers in the lining of the colon. The main symptoms include rectal bleeding, frequent diarrhea, and abdominal pain. Diagnosis involves blood tests, colonoscopy, and ruling out other conditions. Treatment focuses on inducing and maintaining remission through medications like mesalamine, corticosteroids, immunosuppressants, and biologics. Surgery may be needed for severe cases or complications that do not respond to medical management. The goals of treatment are to achieve mucosal healing and prevent hospitalizations and surgery.